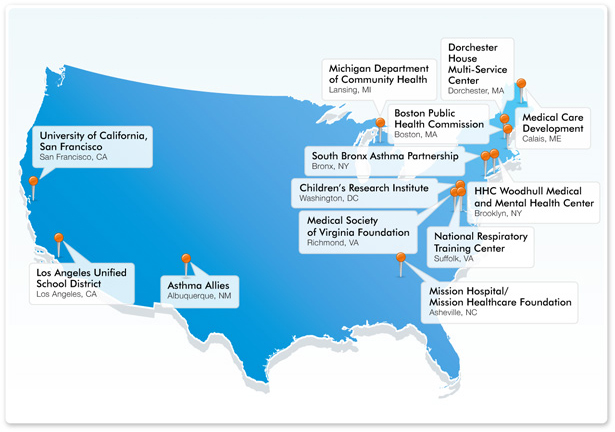
NACI Demonstration Projects: Putting Asthma-Control Best Practices into Practice
The NACI is funding 13 demonstration projects across the United States to design and implement innovative interventions to apply GIP Report recommendations and strategies.
The 13 projects will address barriers to guidelines implementation and asthma disparities and will receive a total of $1.3 million in funding over the course of two years (see NHLBI's NACI Demonstration Projects press release). Altogether, they will reach thousands of patients, families, and caregivers ; health care professionals ; schools and childcare settings ; states, communities, and coalitions ; employers, employees, and worksites ; and public and private purchasers and insurers in a broad array of settings across the country.
Outcomes from the demonstration projects will help inform the NACI and the broader asthma community about best practices to promote the adoption of asthma guidelines and improve the quality of asthma care nationwide.
Project Descriptions
Asthma Allies (Albuquerque, NM)
Located in Albuquerque and Santa Fe, New Mexico, the Asthma Allies' Home Visit Asthma Management Program (Home VAMP) educated newly diagnosed patients with asthma on asthma self-management and utilizes in-home interventions to decrease their exposure to asthma triggers. The program fell within Priority Area 2 of the NACI Action Plan: Indoor Environmental Asthma Triggers – Education and Exposure Reduction. [Full Profile]
[back]
Boston Public Health Commission (Boston, MA)
The Boston Home Visit Coordination Pilot was a program of the Boston Public Health Commission, in collaboration with clinical, community, and advocacy partners, and payers, to demonstrate the effectiveness of citywide asthma home visiting interventions. The program, which focused on the needs of low-income residents and racial, ethnic, and linguistic minorities, utilized home-based asthma education and advocacy services with health workers, clinical practice, and an online referral and follow-up system accessible to clinicians and public health officials. The project was designed to result in a replicable model for asthma home visiting, including forms, training, protocols and health insurance coverage. [Full Profile]
[back]
Children’s Research Institute (Washington, DC)
Located in the District of Columbia, Children’s Research Institute created a program designed to break the cycle of emergency department recidivism for asthma among disadvantaged urban and minority children. The program created new linkages among three key players at the Children’s National Medical Center to transition high users of emergency department care to longitudinal care by primary care physicians, and an electronic standardized Asthma Encounter Form that communicates essential patient information needed to coordinate efforts by the three key players. [Full Profile]
[back]
Dorchester House Multi-Service Center (Dorchester, MA)
The Spirometry Integration Project (SIP) was conducted by Dorchester House Multi-Service Center and designed to improve upon the past success of the Asthma Care Improvement Program (ACIP) to keep disadvantaged minority children out of the emergency department by training and equipping primary care providers with spirometry tools and knowledge. The objective of the project was to increase accuracy for the diagnosis, assessment of severity and control, and prescribing for asthma in Dorchester, Massachusetts. [Full Profile]
[back]
HHC Woodhull Medical and Mental Health Center (Brooklyn, NY)
Physician Asthma Care Education Reinforcement (PACER), ran by HHC Woodhull Medical and Mental Health Center, sought to increase the application of a single standard of care based on the EPR-3 asthma guidelines for patients in Brooklyn, New York. The program used an expert coach that trained and counseled providers on the EPR-3 guidelines as an expansion of the Physician Asthma Care Education (PACE) and Nurse Asthma Care Education (NACE) programs. The program also empowered patients through the distribution of updated PREP (People Reaching Empowerment Program) for asthma cards. [Full Profile]
[back]
Los Angeles Unified School District (Los Angeles, CA)
The Enhanced Strategies for Schools (ESS) project was an innovative venture by the Los Angeles Unified School District’s (LAUSD) Nursing Services Asthma Program. It sought to strengthen links among students, families, providers, and schools by utilizing Web-based trainings and user-friendly tools to increase understanding of asthma symptoms and control. Other goals of the project were to increase the number of written asthma action plans for students at LAUSD and to reduce the number of irritants and allergens that trigger asthma at home and school. [Full Profile]
[back]
Medical Care Development (Calais, ME)
Medical Care Development (MCD) developed the Asthma Practice Improvement Project in collaboration with Calais Regional Medical Services and Calais Hospital in Washington County, Maine. The goal of the Asthma Practice Improvement Project was to improve the care of those with asthma by working with rural medical practices in a learning collaborative model. Key focus areas of the project were to provide medical education based on the EPR-3 guidelines, increase relationships between providers and their local community, and assure that asthma care is well understood by patients and families. MCD also worked in partnership with Maine CDC’s Asthma Prevention and Control Program. [Full Profile]
[back]
Medical Society of Virginia Foundation (Richmond, VA)
This project aimed to expand the Improving Asthma Care and Treatment (IMPACT) project of the Medical Society of Virginia Foundation by adding a pediatric component based on the EPR-3. It educated pediatricians and their staff about how to incorporate the principles of the chronic care model and practice redesign as well as the principles of quality improvement to demonstrate improvements in health care delivery and asthma patient care. Pediatric health care providers in central Virginia, especially those that serve diverse racial and ethnic patient populations, were targeted. [Full Profile]
[back]
Michigan Department of Community Health (Lansing, MI)
The Michigan Department of Community Health (MDCH) Asthma Prevention and Control Program, in collaboration with partners from the Asthma Initiative of Michigan (AIM), worked to address Michigan’s asthma burden through a program called the Asthma Guideline Implementation Steps and Tools (GIST). Through GIST, simple tools and redesign measures were created to help clinicians and health care providers incorporate all six of the key messages of the GIP Report into their everyday practice. These tools were piloted in two practices where they will be evaluated for impact on asthma action plans, asthma control assessment, and inhaled corticosteroid prescriptions. [Full Profile]
[back]
Mission Hospital/Mission Healthcare Foundation (Asheville, NC)
Mission Hospital’s Asthma Disease Management Program and Mission Healthcare Foundation designed a program for rural Western North Carolina to address health disparities in minority children suffering from asthma. Through this program, children and families were given care and education in their local settings—homes, childcare centers, and schools. The program’s ultimate goal was to subjectively improve a patient’s quality of life, decrease school absenteeism, and decrease emergency department utilization and/or inpatient visits—resulting in cost avoidance. Key collaborators include the North Carolina Asthma Program, Asthma Alliance of North Carolina, Western North Carolina School Systems and Child Care Centers, and North Carolina Department of Environmental and Natural Resources. [Full Profile]
[back]
National Respiratory Training Center (Suffolk, VA)
EPR-3: Medical Providers as Asthma Guideline Implementation Champions (EPR-3 MAGIC) was a nationwide program run by the National Respiratory Training Center. It provided a comprehensive and evidence-based medical education program for nurse practitioners, that utilized distance-learning and in-person training methods. The program was implemented in collaboration with three nurse practitioner organizations—American Academy of Nurse Practitioners (AANP), American College of Nurse Practitioners (ACNP), and National Association of Pediatric Nurse Practitioners (NAPNAP). The project also developed EPR-3 champions who disseminated the guidelines in their local communities and evaluated the continuing medical education program. [Full Profile]
[back]
South Bronx Asthma Partnership/Bronx-Lebanon Hospital (Bronx, NY)
The "Asthma Passport" was a project designed by the South Bronx Asthma Partnership and Bronx-Lebanon Hospital Center to bridge gaps in asthma control by empowering both health care providers and parents of children with asthma in the South Bronx with specific knowledge, skills, and confidence to effectively navigate the critical components of the written asthma action plan. A palm-sized Asthma Passport served as a guide to promote skill-based, literacy-sensitive asthma self-management education. A provider curriculum and a parent curriculum, both based on the Asthma Passport, helped to align patient and provider communication and their goals for asthma control. SOBRAP conducted this project at 11 Bronx-based childcare centers, where 0 to 4-year-olds make more asthma-related emergency department visits than any other age group. [Full Profile]
[back]
University of California, San Francisco (San Francisco, CA)
UCSF's partnership addressed childhood asthma health disparities by applying a physician asthma care education training program to improve physician-patient communication in asthma care and asthma outcomes. This program included instruction on the NHLBI’s asthma guidelines and reviewed key asthma messages and specific communication techniques. Clear communication and a partnership for care are crucial for implementing all six GIP priority messages in everyday practice. UCSF applied the program to address the needs of a diverse population in California and evaluated potential modifications to acknowledge the cultural and logistical differences in addressing the needs of a minority and underserved population. [Full Profile]
[back]
















 Twitter
Twitter
 Facebook
Facebook YouTube
YouTube