U.S. Department of Health & Human Services
Email Updates ![]() Font Size
Font Size 
 Print
Print  Download Reader
Download Reader 
HHS Environmental Justice Strategy2012 Environmental Justice Strategy and Implementation Plan (PDF - 778 KB) Message from Secretary Kathleen Sebelius
There’s nothing more important than health. When we live longer, healthier lives, we have more time to do our jobs, volunteer in our neighborhoods, play with our children, and watch our grandchildren grow up. Health is the foundation of our country’s prosperity. Healthy adults are more productive workers, healthy children are better students and healthy families can make bigger contributions to their communities. In our Environmental Justice Strategy and Implementation Plan, you can find many programs that are already making a difference, such as the National Institute of Environmental Health Sciences (NIEHS) Minority Worker Training Program. This program has awarded grants in more than 30 communities across the United States to recruit and train individuals who live in vulnerable communities at risk of exposure to contaminants for employment in the environmental field. The Affordable Care Act, the health reform law of 2010, includes a new community transformation grant program that builds on the Economic Empowerment Zone model. By promoting healthy lifestyles, especially among population groups experiencing the greatest burden of chronic disease, these grants help improve health, reduce health disparities, and control health care spending. The Centers for Disease Control and Prevention made 61 awards, totaling approximately $103 million, to state and local government agencies, Tribes, and territories, and to non-profit organizations. Several awardees are planning to focus on expanding efforts to address healthy and safe physical environments. With the release of our Strategy and Implementation Plan, we are renewing our commitment to working with our Federal partners to promote environmental justice. Equally important, we are reaffirming our commitment to work with communities who are eager to get involved in this effort. We look forward to this collaboration as we continue to focus on building safe and healthy communities. Kathleen Sebelius TABLE OF CONTENTS
EXECUTIVE SUMMARYEnvironmental Justice is “the fair treatment and meaningful involvement of all people regardless of race, color, national origin, or income with respect to the development, implementation, and enforcement of environmental laws, regulations, and policies”. Executive Order 12898, Federal Actions to Address Environmental Justice in Minority Populations and Low-income Populations requires each Federal agency to “make achieving environmental justice part of its mission by identifying and addressing, as appropriate, disproportionately high and adverse human health or environmental effects of its programs, policies, and activities on minority populations and low-income populations.” The Executive Order also states that “each Federal agency responsibility set forth under this order shall apply equally to Native American programs.” The Executive Order, issued in 1994, required each agency to develop an agency-wide environmental justice strategy specific to that agency’s mission. The Department of Health and Human Services (HHS) issued its first Environmental Justice Strategy in 1995. In response to the reinvigoration of the Federal Environmental Justice effort in 2010, HHS has developed a new Environmental Justice Strategy and related implementation actions. The new strategy, 2012 HHS Environmental Justice Strategy and Implementation Plan (2012 HHS EJ Strategy) builds on collaborative efforts across the Department and focuses on the vision of “a nation that equitably promotes healthy community environments and protects the health of all people”. To update the 1995 HHS EJ Strategy, HHS created an Environmental Justice Strategic Planning Committee, composed of representatives from agencies and offices across HHS. The Committee reviewed past and current environmental justice programs and accomplishments to glean lessons learned and build upon successful strategies and activities. HHS also engaged multiple stakeholders during the strategic planning process in order to hear community and other stakeholder concerns, discuss best practices and model programs, and learn about ongoing and emerging environmental justice issues impacting Americans. The 2012 HHS EJ Strategy provides direction for HHS efforts to achieve environmental justice as part of its mission by: (1) identifying and addressing disproportionately high and adverse human health and environmental effects on low-income populations and Indian Tribes, and (2) encouraging the fair treatment and meaningful involvement of affected parties with the goal of building healthy, resilient communities and reducing disparities in health and well-being associated with environmental factors. Driven by public input and HHS support, the strategy maintains the following three guiding principles:
On the basis of the guiding principles, the 2012 HHS EJ Strategy is organized into four strategic elements; (1) Policy Development and Dissemination, (2) Education and Training, (3) Research and Data Collection, Analysis, and Utilization, and (4) Services. The 2012 HHS EJ Strategy reflects new and ongoing actions that are underway or planned for the near term. Each strategic element is aligned with targeted goals, strategies, and actions to be undertaken by HHS. The heightened coordination within and outside of HHS and the engagement of communities and other stakeholders will facilitate the implementation of the 2012 HHS EJ Strategy and support the realization of the vision. SUMMARY OF STRATEGIC ELEMENTS, GOALS, AND STRATEGIES
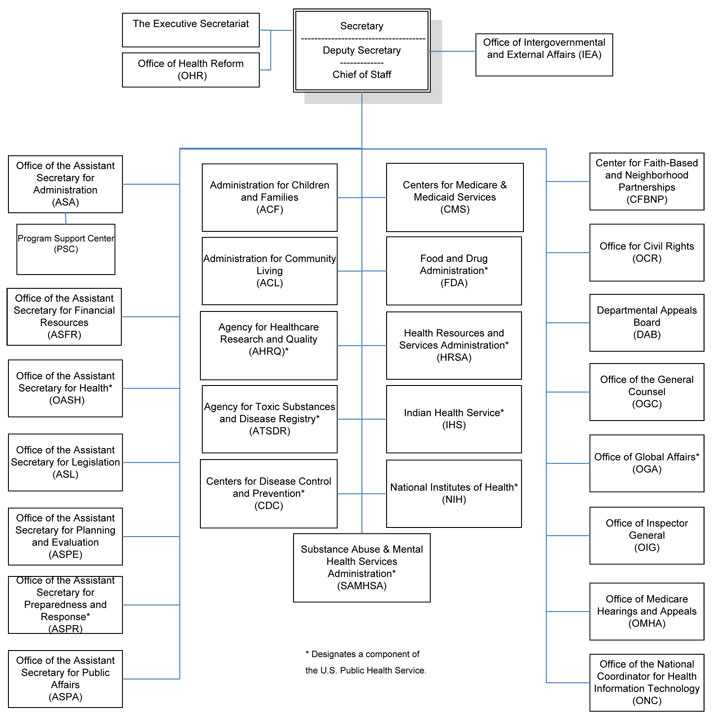
INTRODUCTION AND BACKGROUNDHHS Mission and Role in Environmental Justice The mission of the U.S. Department of Health and Human Services (HHS) is to enhance the health and well-being of Americans by providing for effective health and human services and by fostering sound, sustained advances in the sciences underlying medicine, public health, and social services. HHS is the U.S. government’s principal agency for protecting the health of all Americans and providing essential human services, especially for those who are least able to help themselves. Given the persistent, disproportionate burden of environmental hazards on minority and low-income populations and Indian Tribes, HHS will make achieving environmental justice part of its mission by (1) identifying and addressing disproportionately high and adverse human health and environmental effects on minority and low-income populations and Indian Tribes, and (2) encouraging the fair treatment and meaningful involvement of affected parties with the goal of building healthy, resilient communities and reducing disparities in health and well-being associated with environmental factors. The 2012 HHS Environmental Justice Strategy and Implementation Plan (2012 HHS EJ Strategy) proposes a set of strategic elements, goals, strategies and actions to achieve the Department’s overarching goals, as outlined in the HHS Strategic Plan 2010-2015 1. As demonstrated in the HHS Strategic Plan 2010-2015, HHS’s assets lie in its programs, policies and activities that (1) provide access to health care, (2) help children get a healthy start in life, (3) advance scientific research to promote health and prevent disease, (4) provide human services for the social and economic well-being of individuals and families, (5) promote prevention and wellness for families and communities, (6) protect against domestic and global health threats and (7) ensure the safety of food and drugs. These programs, policies and activities constitute critical tools for achieving health equity and reducing the health disparities that may result from disproportionate exposures to environmental hazards in minority and low-income populations and Indian Tribes. The Relationship of Health and the Environment The environment is a leading determinant of human health and well-being 2. It is well recognized that the social determinants of health, i.e., the conditions in which people are born, grow, live, work, and play, are important factors in the health and well-being of individuals and communities.3. Thus, the concept of environment has evolved to include both the physical and social environments, as well as the interactions between these environments. The physical environment is comprised of the natural environment (i.e., plants, air, water, and weather) and the built environment (i.e., infrastructure such as buildings, roads, parks, and other spaces)4. The social environment is the aggregate of cultural and social institutions, norms, and beliefs that influence the life of an individual or community5. It encompasses health-related behaviors in a community as well as policies within school, work and recreational settings. The social environment also includes socioeconomic conditions (e.g., poverty) and the availability of resources (e.g., educational and employment opportunities, and access to affordable, healthy foods and community-based services) to meet basic daily living needs. The health of communities and populations is further influenced by policies and programs of both governmental and non-governmental sectors. The impact of the environment on human health cannot be overstated. For example, poor air quality, disproportionate exposure to hazards in the workplace, unhealthy housing conditions (e.g., mold, dampness and pest infestation), and the lack of safe areas for physical activity have been linked to chronic conditions such as asthma and other respiratory diseases, cardiovascular disease and obesity6.The built environment can also pose threats to the mental health of individuals, families and communities. For example, studies have shown that housing and neighborhood quality (e.g., condition and functioning) are associated with increased psychological distress and depression7,9 Developmental disabilities have also been associated with prenatal and childhood exposures to environmental toxicants10 Environmental conditions are known to play an important role in producing and maintaining health disparities among minority and low-income populations14 For example, it has been shown that race and socioeconomic status are highly correlated with living near harmful sources of pollution15 Findings indicating the disproportionate siting of hazardous waste facilities in minority and low-income communities gave rise to the environmental justice movement. The Roots of Environmental Justice – A National Concern Environmental justice16 is defined by the U.S. Environmental Protection Agency (EPA) as:
In the early 1970s, a body of literature documenting the existence of environmental inequalities in the United States began to develop.17 These findings led to a series of studies that focused on the location of hazardous waste sites, one of which was conducted in 1983 by the U.S. General Accounting Office (GAO, now called the U.S. Government Accountability Office). The GAO found that blacks comprised the majority of the population in three of four study communities where hazardous waste landfills were located and that the income of at least 26 percent of the populations in all four communities was below the poverty level.18 The 1987 report, Toxic Wastes and Race in the United States,19 identified significant racial and socioeconomic disparities in the distribution of commercial hazardous waste facilities. They were disproportionately located in areas with predominately poor and minority residents. This report, which helped to launch a national environmental justice movement, called attention to the concentrated burden of environmental pollution on minority and low-income populations and Indian Tribes in the United States. Environmental justice advocates and community stakeholders called for greater public participation in the permitting process of these facilities and for more opportunities to address their health concerns. Executive Order Addressing Environmental Justice On February 11, 1994, President William J. Clinton signed Executive Order 12898, Federal Actions to Address Environmental Justice in Minority Populations and Low-Income Populations.20 The Executive Order requires each Federal agency to “make achieving environmental justice part of its mission by identifying and addressing, as appropriate, disproportionately high and adverse human health or environmental effects of its programs, policies, and activities on minority populations and low-income populations.”20 The Executive Order also states “each Federal agency responsibility set forth under this order shall apply equally to Native American programs.”20 The Executive Order created the Federal Interagency Working Group on Environmental Justice (EJ IWG), convened by the EPA Administrator, and required each agency to develop an agency-wide environmental justice strategy specific to that agency’s mission. 1995 HHS Environmental Justice Strategy In accordance with Executive Order 12898, HHS developed its first environmental justice strategy, Strategic Elements for Environmental Justice in 1995.21 The goal of the 1995 HHS Environmental Justice Strategy (1995 HHS EJ Strategy) was to “ensure that disproportionately high and adverse environmental and health effects experienced by low-income and minority populations are addressed, as appropriate, in the programs of the Department of Health and Human Services (HHS), and that these programs encourage the full involvement of affected parties.”21 The objectives of the Strategy addressed six elements: (1) Public Partnerships, (2) Public Education and Training, (3) Services, (4) Data Collection and Analysis, (5) Health Research and (6) Interagency Coordination. HHS Operating Divisions and Staff Divisions developed and implemented programs, initiatives and activities that addressed the elements of the 1995 HHS EJ Strategy. Operating Divisions and Staff Divisions supported more than 70 different programs, initiatives and activities, ranging from public websites and toll-free numbers to technical assistance programs and cooperative agreements, grants and contracts that addressed the needs of communities with environmental justice issues. Below are examples of past and current activities supported by HHS that align with the 1995 HHS EJ Strategy’s elements. Public Partnerships
Public Education and Training
Services
Data Collection and Analysis
Health Research
Interagency Coordination
Current Landscape of Environmental Justice and Health Disparities Since the development and implementation of the 1995 HHS Strategy, progress has been made in identifying and addressing disproportionately high and adverse environmental exposures among minority and low-income populations and Indian Tribes, but inequities persist. Race and poverty continue to be critical determinants of disproportionate exposure to environmental hazards. Despite the advances made to elevate environmental justice as an issue, critical health disparities related to environmental exposures remain. The disparity in asthma prevalence provides a striking example of the effect of disproportionate adverse exposures and health outcomes. The prevalence of asthma is highest among multi-racial Americans, Hispanics of Puerto Rican descent and non-Hispanic blacks, and is also higher among those living in poverty.6. Disproportionate exposures to particulate matter and ozone air pollution contribute to differences in asthma severity. Hispanics, Asians, Pacific Islanders and non-Hispanic blacks are more likely to live in a non-attainment area1 for particulate matter air pollution than non-Hispanic whites.6. The obesity epidemic has highlighted the interaction of the built environment with other biologic, social and cultural factors in contributing to racial and ethnic disparities in the prevalence of obesity.22 Predominantly minority communities have fewer grocery stores and less access to affordable, healthy foods. Poor neighborhoods disproportionately lack outdoor recreation areas that are safe, have a greater density of fast food locations, and are designed with few opportunities for biking and walking..22, 24 Disparities also exist in housing and workplace settings. Inadequate and unhealthy housing contributes to infectious and chronic diseases, injuries, and adverse childhood developmental outcomes. Non-Hispanic blacks, Hispanics, and American Indians/Alaska Natives are at least twice as likely to live in inadequate housing as non-Hispanic whites.6 Workers in lower-status and lower-wage jobs, who are largely minorities, face increased occupational hazards, including chemical exposures, poor working conditions, and psychosocial stressors (e.g., lack of control over working conditions).25 Children and pregnant women are particularly vulnerable to adverse environmental exposures, and minority and low-income children experience significant health disparities due to disproportionate exposure to environmental hazards. Childhood lead poisoning is largely concentrated in poor, minority communities.24 Rates of birth defects in infants born to Navajo women living in uranium mining areas have been shown to be several times higher than the national average.26 Environmental justice and health disparities also cross geographic boundaries impacting urban areas and rural communities. Rural areas share many of the health challenges associated with environmental factors such as obesity, which is in part related to the lack of access to healthy foods. Agricultural workers and communities near industrial farming have unique health issues. Agricultural workers who are licensed pesticide applicators may suffer adverse neurological effects from increased exposure to pesticides in their workplace.27 Industrial farming, in particular concentrated animal feeding operations, can negatively impact health and quality of life. Emissions and chemicals used in such operations have been shown to be disproportionately located in minority and low-income communities of rural areas.28 Studies of extreme weather events, such as heat waves and hurricanes, have demonstrated that low income and minority individuals experience more severe health outcomes and live in communities with less resilience from these disasters than more affluent communities.29 Climate change is anticipated to increase the severity and frequency of such extreme weather events in some parts of the United States. Climate change may also exacerbate problems such as air pollution and inadequate housing quality,30 which may lead to health outcomes such as increased prevalence or severity of asthma and other respiratory conditions, and increased prevalence of mental illness.31, 32 Reinvigorating Federal Environmental Justice Efforts In light of the Obama Administration’s commitment to healthy environments for all Americans, the Federal Interagency Working Group on Environmental Justice was reconvened on September 22, 2010 to protect the health and advance the economic potential of communities overburdened by pollution and other environmental hazards. In August 2011, HHS reaffirmed its commitment to environmental justice by joining 16 Federal agencies in signing a Memorandum of Understanding (MOU) on Environmental Justice and Executive Order 12898.33 The MOU renews each agency’s responsibility to develop an environmental justice strategy and prepare implementation progress reports, establishes structures and procedures to ensure that the Interagency Working Group operates effectively, and identifies areas of focus to be included in agency environmental justice efforts. This agreement provides a roadmap for agencies to coordinate environmental justice efforts and to work together to build healthy and resilient communities. HHS ENVIRONMENTAL JUSTICE STRATEGY OVERVIEWThe HHS vision for environmental justice is as follows:
Development of the 2012 HHS Environmental Justice Strategy To update the 1995 HHS EJ Strategy, HHS created an Environmental Justice Strategic Planning Committee, composed of representatives from Operating Divisions and Staff Divisions across the Department. The Committee reviewed key historical environmental justice documents, including Executive Order 12898, the 1995 HHS Strategy, the Integrated Federal Interagency Environmental Justice Action Agenda, previous HHS environmental justice implementation progress reports and the 2011 Memorandum of Understanding on Environmental Justice. The HHS Strategic Planning Committee also reviewed past and current environmental justice programs and accomplishments across HHS to glean lessons learned and build upon successful strategies and activities. Upholding the environmental justice principle of meaningful involvement, HHS engaged stakeholders during the strategic planning process in order to hear community and other stakeholder concerns, discuss best practices and model programs, and learn about ongoing and emerging environmental justice issues impacting communities. Stakeholders included community-based and grassroots organizations; state, local, and tribal governments; academia; non-governmental organizations; and members of the general public. HHS representatives participated in every stakeholder meeting hosted by the Federal Interagency Working Group on Environmental Justice across the country (Appendix A. HHS Environmental Justice Stakeholder Engagement). In addition, HHS hosted a listening session in Mobile, Alabama, conducted an environmental justice webinar, and hosted an Environmental Justice Thought Leaders Meeting in Washington, DC. HHS also held a sixty-day online comment period for the Draft 2012 HHS EJ Strategy. The public comment period yielded more than one hundred comments from seventeen sources representing non-profit organizations, State and Tribal entities, academic institutions, advocacy groups and individuals. These comments led to enhancements to the HHS EJ Strategy and affirmed support for the strategy vision, guiding principles, goals, strategies and actions. The Strategy’s implementation steps addressed a number of issues raised by commenters. Commenters asked that HHS continue to engage stakeholders as the Strategy is implemented. HHS will continue to engage community and other stakeholders during the implementation of the HHS EJ Strategy. Guiding Principles and Statutes for the HHS Environmental Justice Strategy In conceptualizing and implementing the 2012 HHS Environmental Justice Strategy (2012 HHS Strategy), HHS will uphold three guiding principles, of which the first two were elements of the 1995 HHS EJ Strategy:
Environmental justice highlights the importance of meaningful involvement through community partnership and engagement.2 Recognizing that communities with environmental justice concerns often have less capacity to access public participation opportunities, HHS will also bolster compliance with the following existing policies and statutes in order to advance environmental justice:
Key Concepts for the HHS Environmental Justice Strategy The 2012 HHS Strategy builds on the 1995 HHS EJ Strategy and the Institute of Medicine’s (IOM) 1999 report entitled, Toward Environmental Justice: Research, Education, and Health Policy Needs. In this report, the IOM assessed potential adverse human health effects caused by environmental hazards in communities of concern and made recommendations in the areas of public health, biomedical research, education and health policy. The IOM described environmental justice as a “concept that addresses in a cross-cutting and integrative manner the physical and social health issues related to the distribution of environmental benefits and burdens among populations, particularly in degraded and hazardous physical environments occupied by minority or disadvantaged populations.”40 The concepts, definitions and framework outlined in the IOM report remain relevant to the challenges and opportunities for addressing environmental justice today. Strategic Elements of the HHS Environmental Justice Strategy The 2012 EJ HHS Strategy is organized into four interrelated strategic elements that mirror the elements of the 1995 HHS EJ Strategy, and includes a new strategic element on Policy Development and Dissemination. This element was added in recognition of the influence of Federal, state, local, tribal and territorial policies on health. Furthermore, the Memorandum of Understanding on Environmental Justice and Executive Order 12898 calls for Federal agencies to address topic areas such as Title VI of the Civil Rights Act of 1964, the National Environmental Policy Act and climate change in their updated strategies. These topic areas are addressed under Policy Development and Dissemination. The four strategic elements are:
For each strategic element, the 2012 HHS EJ Strategy describes background information, specific goals, strategies and actions to be undertaken by designated HHS Operating Divisions and Staff Divisions. Implementation, Reporting and Accountability Successful implementation of the 2012 HHS EJ Strategy will require leveraging multiple opportunities. Many of the actions can be accomplished through improved coordination and integration of existing activities, whereas others are subject to the availability of funds. With a focus on efficiency, transparency and accountability, HHS will monitor and assess the 2012 HHS EJ Strategy. The HHS Environmental Justice Working Group, convened by the Office of the Assistant Secretary for Health and composed of representatives from several HHS agencies and offices, will track the progress on implementing the 2012 HHS EJ Strategy. HHS will regularly seek public input, in particular from impacted communities, through mechanisms such as the community outreach efforts of the Federal Interagency Working Group on Environmental Justice. HHS will also prepare Annual Implementation Progress Reports that will be made publicly available, as outlined in the Memorandum of Understanding on Environmental Justice. Leveraging Key Initiatives The 2012 HHS EJ Strategy builds upon the Administration’s and HHS’s commitment to prevention and wellness and the reduction of health disparities. There are several key national and departmental initiatives that HHS can leverage to advance environmental justice and to promote and protect the health and well-being of minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures.
STRATEGIC ELEMENTSI. Policy Development and DisseminationEffective implementation of policies, such as legislation, regulation, executive orders, policy directives and program guidance can serve as key tools to advance environmental justice. In particular, community residents and advocates have frequently cited Title VI of the Civil Rights Act of 1964 and the National Environmental Policy Act as important levers for achieving environmental justice, in addition to Executive Order 12898.51, 52 Signed in 2009, Executive Order 13514, Federal Leadership in Environmental, Energy, and Economic Performance, represents a new opportunity for environmental justice through its focus on sustainability. All of these directives govern certain actions undertaken by the Federal government and/or entities that receive Federal funding. Furthermore, the Memorandum of Understanding on Environmental Justice and Executive Order 12898, signed in August 2011 by HHS and 16 other Federal departments and agencies, outlines initial areas of focus for Federal environmental justice activities. These areas of focus include Title VI of the Civil Rights Act of 1964, the National Environmental Policy Act and climate change. HHS can also develop and disseminate policy guidance for specific HHS programs and activities, such as its grant programs. Title VI of the Civil Rights Act of 1964 Title VI of the Civil Rights Act of 1964 (“Title VI”) and its implementing regulations at 45 C.F.R. Part 80 serve as tools to assist in the enforcement of environmental justice efforts. Title VI states that “No person in the United States shall, on the ground of race, color, or national origin, be excluded from participation in, be denied the benefits of, or be subjected to discrimination under any program or activity receiving Federal financial assistance.” HHS has separate responsibilities under Title VI and Executive Order 12898. At HHS, the Office for Civil Rights (OCR) is charged with Title VI enforcement and ensuring that Federal money for health care and social service programs is not used to support programs or activities that discriminate on the basis of race, color or national origin. Where Title VI provides enforceable rights for aggrieved individuals, Executive Order 12898 directs Federal agency action towards achieving environmental justice “by identifying and addressing, as appropriate, disproportionately high and adverse human health or environmental effects of its programs, policies, and activities on minority populations and low-income populations…”20 without providing individual rights or remedies. Therefore, OCR’s Title VI enforcement program is allied with Executive Order 12898, and is an essential component of HHS’s efforts in achieving equitable health outcomes for all. National Environmental Policy Act Enacted in 1970, the National Environmental Policy Act (NEPA) sets forth requirements to ensure that environmental factors are considered in Federal agency decision-making.53 NEPA establishes procedural requirements for all Federal agencies in preparing Environmental Assessments (EAs) and Environmental Impact Statements (EISs). EAs and EISs contain statements of the environmental effects of proposed Federal agency actions. Within HHS, many EAs and EISs pertain to proposed decisions concerning facilities, particularly construction or repurposing of facilities. However, other actions are also evaluated for their environmental impact. For example, the Food and Drug Administration considers the environmental impacts (use and disposal) resulting from the Federal action of approving a drug or food/feed additive application. HHS consideration of environmental justice within the NEPA process can occur in various ways, including:
Federal agencies including HHS are required to periodically update their NEPA policies. After the issuance of Executive Order 12898, the White House Council on Environmental Quality issued guidance in support of identifying and addressing environmental justice concerns in the NEPA process.54 Sustainability and Executive Order 13514: Federal Leadership in Environmental, Energy, and Economic Performance Sustainability has been defined as “the enduring prosperity of all living things.”54 By this measure, sustainability is directly linked to the health of humans, the health of the environment and the health of economic systems that support and promote our well-being. Executive Order 13514, signed on October 5, 2009, establishes an integrated strategy towards sustainability in the Federal government and makes reduction of greenhouse gas emissions (GHG) a priority for Federal agencies. The Executive Order requires Federal agencies to reduce GHG emissions caused by their activities and sets goals in other areas of environmental stewardship, such as efficient use of water and reduction of waste. As called for by Executive Order, HHS developed a Strategic Sustainability Performance Plan55 that is updated annually. Through the Performance Plan, HHS will ensure that its actions promote health and well-being and do not add to the burden of illness borne by any community or population, including minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures. Strategies to accomplish this goal include (1) reducing greenhouse gas emissions through technological, programmatic and behavioral change, (2) decreasing the amount of mercury released into the air from combustion of fossil fuels and (3) reducing other sources of air pollution that are associated with negative health effects. Other strategies HHS will employ include reducing HHS consumption of resources and responsibly managing our waste, actions that can reduce the amount of toxins that enter water sources and food chains. Reuse and recycling efforts reduce harmful emissions and lessen the amount of land devoted to landfills and raw material extraction. Reduction or elimination of toxic substances in materials and services that HHS uses reduces exposures in communities that produce them and among those exposed to them throughout their lifecycle. Climate Change Directives A number of Federal initiatives call for increased awareness of and preparation for the impacts of climate change, including Executive Order 13514 and the recommendations of the Interagency Climate Change Adaptation Task Force.56 HHS can improve the resiliency of vulnerable individuals and marginalized communities, through increased understanding of the human health impacts of climate change and preparedness planning at the state and local levels. Health outcomes that are sensitive to climate change include asthma, cardiovascular disease, stroke, heat-related illnesses and deaths, and mental and stress-related disorders.31 Populations that are most vulnerable to the effects of climate change include impoverished populations, women, children, racial and ethnic minorities, immigrants, the frail elderly, persons with disabilities and refugees.31, 57, 58 Climate change adaptation and mitigation strategies3 should be tailored to the needs of vulnerable communities and populations and not cause adverse impacts on these populations. HHS programs provide services to individuals in these populations, many of which have disproportionate health burdens. Through policy development and dissemination initiatives, HHS will engage in actions related to Title VI, the National Environmental Policy Act, sustainability, climate change and opportunities to advance health and environmental justice in HHS programs and policies. With regard to climate change and sustainability, multidimensional actions will be undertaken, including research, surveillance, education, services and policy.
Strategies and Actions A. Integrate environmental justice principles and strategies into the implementation of key statutes and policies that may impact minority and low-income populations and Indian Tribes (e.g., Title VI of the Civil Rights Act of 1964, the National Environmental Policy Act and Executive Order 13514). Action A.1 Incorporate, where feasible and appropriate, environmental justice in award criteria of HHS grants and other funding opportunities. Lead: HHS Environmental Justice Working Group
Action A.2 Update existing public information materials on Title VI to include information and resources on environmental justice. Update the HHS Office for Civil Rights website, adding a special topic area on environmental justice and information for minority and low-income populations and Indian Tribes. Lead: HHS Office for Civil Rights
Action A.3 Conduct outreach events to educate local communities on the purpose and functions of the HHS Office for Civil Rights and to solicit public input on how the HHS Office for Civil Rights can best serve local communities. Outreach event locations will include communities with minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures. Information and resources on Title VI and environmental justice will be shared during the outreach events. Lead: HHS Office for Civil Rights
Action A.4 Update the HHS NEPA Policy (HHS General Administration Manual 30) to incorporate relevant environmental justice guidance and the principles of environmental justice. HHS will consult with the Council on Environmental Quality and HHS Operating Divisions, review and compare NEPA policy documents from other agencies, assess overall HHS NEPA compliance and update categorical exclusions and relevant procedures. Lead: ASA; Participating: CDC, FDA, HRSA, IHS, NIH
Action B.1 Integrate environmental justice principles and the 2012 HHS Environmental Justice Strategy actions into the HHS Strategic Sustainability Performance Plan (SSPP) to prevent and reduce adverse impacts on vulnerable populations, including minority and low-income populations and Indian Tribes. Lead: ASA
Action B.2 Conduct a vulnerability assessment of HHS’s programs to climate change and develop an adaptation strategy, as required by Executive Order 13514. The vulnerability assessment and adaptation strategy will enable HHS to develop actions to build resilience of the Department to climate change risks and therefore minimize adverse impacts on vulnerable populations, including minority and low-income populations and Indian Tribes. Lead: ASA; Participating: NIH (NIEHS), CDC (NCEH), ACF
Action B.3 Promote the consideration of factors such as health, environment, distributive impacts and equity in the development of Federal agencies’ policies and program planning. Lead: ASA, ASPE; Participating: HHS Environmental Justice Working Group
Action B.4 Advance research that contributes to a better understanding of the relationship between health, sustainability, and environmental quality to support environmental justice efforts and initiatives. Lead: NIH (NIEHS)
Action B.5 Support research on potential health impacts of climate change, including the impacts of climate mitigation and adaptation measures, that includes methodologies such as community-based participatory research and incorporates environmental justice principles. Lead: NIH (NIEHS)
Action B.6 Produce guidance for state, local, territorial, and tribal health departments on integrating extreme weather and public health surveillance systems with special emphasis on communities most vulnerable to changes in extreme weather patterns, including minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures. Lead: CDC (NCEH)
Action B.7 Develop guidance on identifying the spatial and temporal extent of climate and extreme weather vulnerability and risk within communities containing existing environmental inequalities. Lead: CDC (NCEH)
Action B.8 Develop guidance on how state, local, territorial, and tribal public health departments can adopt policies and programs that minimize climate-related health impacts among vulnerable populations, including minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures. Lead: CDC (NCEH)
Action B.9 Build community resilience and sustainable, stronger health and emergency response systems in at-risk populations with disproportionately high and adverse environmental exposures to prevent or reduce emerging health threats and chronic health problems. Strategies and actions undertaken through the implementation of the National Health Security Strategy will support this effort. Participating: ASPR, CDC, other HHS Operating Divisions and Staff Divisions
C. Provide consultation and/or partner with other Federal departments, where appropriate and feasible, on environmental policies, programs and initiatives that may impact health and well-being, with particular attention to minority and low-income populations and Indian Tribes. Action C.1 Collaborate, where appropriate and feasible, with Federal partners on initiatives related to sustainability and healthy settings (e.g. communities, schools, housing and workplaces) to advance a “health in all policies” approach to prevent or reduce negative impacts on minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures. Lead: OASH; Participating: ASPE, ACF, HHS Environmental Justice Working Group
II. Education and TrainingEducation and training are fundamental strategies to achieve environmental justice and build healthy community environments. Through education and training, individuals, families and communities become more informed and empowered to actively address health concerns about harmful environmental exposures. Effective education and training should be comprehensive, targeting not only residents and workers with disproportionately high and adverse environmental exposures, but also health professionals, human services providers, and relevant government officials and employees that develop and implement programs, policies and activities impacting and serving these communities. The Insitute of Medicine (IOM), in its 1999 report Toward Environmental Justice: Research, Education, and Health Policy Needs39, described the sentiments of community members the committee met during site visits as “defenseless” and “abandoned” in confronting environmental challenges in their communities. The IOM recognized the importance of education as part of the solution to building a well-informed community. The IOM identified that primary health care providers lack specific training in environmental and occupational medicine. Limited education and training in environmental health and environmental justice is also a challenge in public health professional education. These findings led the IOM to recommend that environmental justice and environmental health should be a focus of educational efforts, specifically by enhancing health professionals’ knowledge and improving the general public’s awareness and understanding of these issues. Twelve years after the publication of this landmark IOM report, the need for education and training on environmental justice and health remain. Stakeholders and community residents continue to identify the need for access to information on environmental exposures and health effects, the need for community resources to address unmet health and services needs, and the limited availability of providers who understand environmental health concerns. Advocates highlight the importance of public engagement as a fundamental principle of environmental justice. As part of this effort, there are also urgent needs for training government employees and researchers to enhance their skills in community engagement, cultural competency and risk communication. They can then partner with and support communities with disproportionately high and adverse environmental exposures more effectively60,61. HHS will implement a multi-sectoral approach to education and training in health and environmental justice targeted to the following stakeholders: (1) community and the public, (2) professionals (health care workforce, public health professionals, and human services providers) and (3) the HHS workforce.
A.1 Increase public awareness of and access to information on health and environmental justice by developing an HHS environmental justice website. This website will serve as a point of entry for the public to learn about HHS activities and resources related to environmental justice. Lead: ASH, NIH (NIEHS), ASPA; Participating: ACF, ATSDR, CDC, NIH (NIMHD, NLM)
Action A.2 Partner with other Federal departments to develop and implement integrated educational outreach and intervention programs for agricultural workers and their families, focused on environmental hazards from the work environment, as well as from unhealthy housing, poor sanitation, food insecurity and other neighborhood environmental issues. Lead: CDC (NIOSH), NIH (NIEHS); Participating: HRSA
Action A.3 Prepare guidance for HHS-funded worker training programs that are designed to assist disadvantaged communities. The guidance will include information on innovative techniques to improve the effectiveness and efficiency of these programs. It will also provide model strategies to address barriers to successful program implementation (e.g., trainees who lack access to transportation or trainees who have low educational attainment). Lead: NIH (NIEHS); Participating: CDC (NIOSH), OMH
B. Enhance health professionals’ and human services providers’ education and training in environmental health and environmental justice.
Action B.1 Expand and promote educational outreach on health and environmental justice, including continuing education programs, to primary health care and behavioral health care providers, other health professionals, public health professionals and the human services workforce. Lead: ATSDR, HRSA; Participating: ACF, CDC (NCEH, NIOSH) , OMH
Action B.2 Incorporate environmental justice and environmental and occupational safety and health education in the training curricula of community health workers and Promotores de Salud that is underway as part of the HHS Action Plan to Reduce Racial and Ethnic Health Disparities. Also incorporate this education component into the training curricula of community health representatives within the Indian Health Service and HRSA, through coordination with OMH. Lead: OMH; Participating: ATSDR, CDC (NIOSH), CMS, IHS, NIH (NIEHS)
Action B.3 Increase partnerships with Historically Black Colleges and Universities, Tribal Colleges and Universities, and Hispanic-Serving Institutions. Strengthen collaborations with the academic institutions in the National Institute of Environmental Health Sciences (NIEHS) Partnerships for Environmental Public Health Program, as well as the National Institute for Occupational Safety and Health (NIOSH)-initiated Education and Research Centers. Through these collaborations, promote education and training programs aimed at eliminating disparities in environmental health and occupational safety and health. Lead: NIH (NIEHS, NIHMD); Participating: ATSDR, CDC (NCEH, NIOSH), HRSA, IHS, OMH
C. Increase the knowledge and understanding of health and environmental justice across HHS agencies and among HHS employees. Action C.1 Develop and implement a training program for HHS employees on the principles and practice of environmental justice, including community engagement. The program will enhance HHS workforce competency on environmental justice and build capacity to work effectively with communities. The program will also improve the effectiveness and efficiency of HHS programs and policies tailored to environmental issues and minority and low-income populations and Indian Tribes. Various mechanisms, such as environmental justice training modules, curricula and webinars, will be used. Lead: ASA, OMH; Participating: ACF, NIH (NIEHS)
III. Research and Data Collection, Analysis and UtilizationAs early as the 1980s, research and data in the environmental and health sciences provided evidence that minority and low-income populations and Indian Tribes bore disproportionate burdens of exposure to environmental hazards.19 Mapping, using technology such as geographic information systems (GIS), has been and continues to be one of the leading data collection and analysis tools to plot environmental hazards spatially and then determine the socio-demographics of the potentially affected population in order to assess disproportionate exposure.62 Recent studies demonstrate that the disparate distribution of hazardous waste facilities continues to exist.63 Furthermore, minority and low-income populations and Indian Tribes are more likely to live and work in unhealthy environments (e.g., inadequate or unhealthy housing and communities with unhealthy air quality).6.Environmental disparities contribute to many health disparities (e.g., low birth weight, infant and adult mortality, asthma, cardiovascular disease and psychosocial stress) between minority and low-income populations and Indian Tribes as compared to the general population.17,39 Current research focuses on assessing environmental exposures through both modeling of exposures and measurement of specific chemicals in residents living adjacent to environmental hazards. This work includes assessments of exposure to multiple hazardous agents and of cumulative exposures over time.64,65 Studies have also addressed the relationship between environmental exposures and specific health effects, such as asthma, cancer and chronic lung disease. The clearest relationship between environmental exposures and health is the exposure of children and workers to lead and the presence of elevated lead in their blood.66 Many studies have shown the toxic effects of lead on the nervous system, blood and other body systems. Despite the strong evidence on the health effects of lead exposure, researching and concluding that an environmental exposure causes a specific health effect has proved challenging. Progress has been made over time in data analysis methods, however important limitations persist. A significant limitation is obtaining data that reliably establish a relationship between the environmental exposure and the socio-demographic characteristics of the populations at risk.67 Populations that live near environmental hazards are often small and have other risk factors for disease, in part related to their minority and low-income status. These other risk factors may include social, behavioral and economic risk factors for poor health.39 In some cases, researchers in the field of environmental justice conclude that social factors are integral to understanding the development of disproportionate and adverse environmental exposures and that additional research is needed to better understand the interaction of environmental and social factors in the attainment of environmental justice.17 In its 1999 report, Toward Environmental Justice: Research, Education, and Health Policy Needs, the Institute of Medicine (IOM) noted the need to improve collection and coordination of environmental health information to better link it to specific populations and communities of concern. The IOM recommended that environmental justice research should serve to “improve the science base, involve the affected population, and communicate the findings to all stakeholders.”39 Data collection, essential to understanding environmental hazards and community health status, is an ongoing challenge for communities.59 Through the research and data collection, analysis, and utilization strategic element, HHS will strive to address research challenges and data deficiencies related to health and environmental justice in order to contribute to and facilitate an improved understanding of the relationship between exposure to environmental hazards and health effects. This effort will aim to inform programs, policies and interventions to eliminate health disparities associated with preventable environmental factors.
Strategies and Actions A. Increase the involvement of minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures in research and in data collection and utilization, and communicate findings to stakeholders. Action A.1 Draft and implement guidance to HHS agencies conducting or funding research in partnership with minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures. The guidance will focus on strategies to promote the environmental justice principles of meaningful involvement and timely communication of information to communities and will reflect key statutes such as Title VI of the Civil Rights Act of 196438 and Section 508 of the Rehabilitation Act of 197335. Moreover, the guidance should address the following issues, as outlined in Executive Order 12898:
Action A.2 Host a Health and Environmental Justice Workshop periodically in conjunction with disproportionately impacted communities. The workshop will (1) present the state of the science in health and environmental justice, (2) explore emerging research areas and existing research and data gaps, (3) solicit public input on research and data needs, and (4) disseminate findings of recent research on health and environmental justice. Lead: HHS Environmental Justice Working Group
Action A.3 Increase public access to information about research and data by expanding the Environmental Justice web pages of the National Library of Medicine’s Specialized Information Services to serve as a clearinghouse of basic, clinical, behavioral, health services and health disparities research and to provide access to information resources on health and environmental justice such as databases, funding opportunities, health information, fact sheets and conferences. Lead: NIH (NLM); Participating: OASH, ATSDR, CDC (NCEH, NIOSH), IHS, NIH (NIEHS and other ICs)
B. Identify and characterize environmental and occupational factors that have disproportionately high and adverse human health or environmental effects on minority and low-income populations and Indian Tribes. Action B.1 Strengthen capacity for research on the health effects of disproportionately high and adverse environmental exposures in minority and low-income populations and Indian Tribes through programs such as (1) the Building Research Infrastructure Capacity and the Centers of Excellence Program at the National Institute on Minority Health and Health Disparities (NIMHD), (2) the Partnerships for Environmental Public Health Program at the National Institute of Environmental Health Sciences (NIEHS), and (3) the Education and Research Centers initiated by the National Institute for Occupational Safety and Health (NIOSH). Participating: NIEHS, NIMHD, NIOSH, IHS, EPA
C. Bolster the efforts of HHS, state, local, territorial and tribal agencies, as well as non-governmental organizations, to collect, maintain and analyze data on disproportionately high and adverse environmental and occupational exposures and on health effects in minority and low-income populations and Indian Tribes. Action C.1 Promote inclusion of questions related to industry, occupation and other parameters of the workplace in HHS-supported surveys and other data collection instruments. Promote analysis of data related to occupational safety and health collected from HHS-supported surveys and other data collection instruments. Lead: NIOSH; Participating: NCEH, ASPE, IHS
Action C.2 Partner with EPA and other Federal departments to review and update community mapping tools and other databases designed to identify minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures and health effects. Through this partnership and in collaboration with impacted communities and other external stakeholders, key environmental and human health indicators for inclusion in these mapping systems will be determined in order to maximize the effectiveness and utility of these databases for communities, governmental agencies, researchers, policymakers and the general public. Lead: CDC (NCEH, NIOSH); Participating: ASPE, IHS, NIH (NIEHS, NIMHD), ONC, EPA
Action C.3 Expand information on health disparities and environmental justice concepts on the National Center for Environmental Health’s (NCEH) National Environmental Public Health Tracking Network and the National Institute for Occupational Safety and Health’s (NIOSH) State–Based Surveillance System to include: (1) additional data and measures to better identify and assess the status of environmental health in minority populations, low-income populations and other vulnerable populations at the local, state and national levels and (2) links to relevant websites and community mapping tools. Lead: CDC (NCEH, NIOSH); Participating: OMH, NIH, IHS, EPA
IV. ServicesHealth is greatly influenced by the social, economic, policy, built and natural environments. The public’s health is at risk when faced with poverty and food insecurity, lack of clean water and air, inadequate or unsafe housing and neighborhood environments, and inadequate health care.68 Minority and low-income populations and Indian Tribes have greater exposure to adverse environmental and occupational hazards. For example, people of color make up 56 percent of those living in neighborhoods located near the nation’s commercial hazardous waste facilities62 This disproportionate exposure is compounded by the fact that minorities are more likely to have inadequate access to a primary care physician, often receive poorer quality of care and face barriers in seeking preventive and acute care69,70 Such communities often have the most pressing need for health care and social services.71 Health and human services for minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures should be targeted to meet multiple health and social concerns. Interventions are needed that identify community health needs and link community members to health services and programs. Numerous resources are essential for building community capacity to address environmental health challenges. Assessment tools, appropriate testing for environmental hazards and the extent of human exposures to hazards, technical assistance, access to quality primary and behavioral health care and community-based services are some examples. Moreover, affected communities should be empowered through active partnership to access, utilize and leverage the resources of government and other institutions.72 Tools such as community health assessments (CHA) can be used to identify environmental health issues within a community. Health impact assessments (HIA) can be used to evaluate potential health effects of development projects and land-use decisions.73 CHA and the Community Health Improvement Process help communities prioritize identified health issues, develop action plans and monitor progress. As an emerging field of practice in the United States, the HIA methodology incorporates potential public health impacts into the decision-making process for plans, project, and policies that traditionally fall outside of the public health arena.72 Through the services strategic element, HHS will utilize its resources and collaborations to improve the quality of primary and behavioral health care in minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures. HHS will also help build community capacity to identify and address community health needs and economic development.
Strategies and Actions A. Increase the capacity of health professionals delivering care and services to minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures to prevent, diagnose and treat medical and behavioral health conditions associated with adverse environmental exposures. Action A.1 Promote inclusion and use of environmental and occupational exposure history in electronic health records (EHR). Lead: ATSDR, CDC (NIOSH), ONC; Participating: CMS, HRSA, IHS
Action A.2 Promote the availability of specialty resources in environmental health such as the Pediatric Environmental Health Specialty Units (PEHSU) to health care providers for consultation in the care and treatment of minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures. Lead: ATSDR; Participating: HRSA, IHS, SAMHSA
Action A.3 Improve the quality of behavioral health care received by minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures by
B. Improve capacity to identify minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures, as well as the physical and behavioral health conditions and concerns of communities affected by these exposures. Action B.1 Evaluate the use of health impact assessments4 (HIA) in minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures to achieve risk reduction and reduce health disparities. Lead: OMH, CDC, ATSDR; Participating: ASPE, OASH
C. Provide technical assistance and information resources to minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures in order to empower communities to address identified health and human services needs. Action C.1 Build community capacity to conduct community health assessments through collaborations with national public health organizations and other Federal agencies and through the development of new tools, or the enhancement of existing tools,[5] for identifying minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures and associated health conditions Lead: CDC, ATSDR; Participating: HRSA, IHS, NIH (NIEHS, NIMHD), SAMHSA
Action C.2 Assess health and human services needs for minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures. Lead: CDC, ATSDR; Participating: ACF, AoA, HRSA, IHS, SAMHSA
Action C.3 Increase outreach to minority populations and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures to raise their awareness of the availability of technical assistance for applying for HHS funding to address their health and human services needs Lead: HRSA, HHS Environmental Justice Working Group
D. Provide funding opportunities and technical assistance, where appropriate and feasible, to advance the economic potential and social well-being of minority and low-income populations and Indian Tribes with disproportionately high and adverse environmental exposures.
Action D.1 Expand funding opportunities, where appropriate and feasible, to underserved communities for economic development and social services through additional outreach and intra-agency partnerships. Provide outreach to potential applicants who have been underserved by funding in the past and enact policies that promote funding underserved applicants. Partner within agency programs to allow underserved populations with limited capability to apply for and manage economic development grants, as with the Native Asset Building Initiative. Lead: ACF
REFERENCES[1]Non-Attainment Area: Any area that does not meet (or that contributes to ambient air quality in a nearby area that does not meet) the national primary or secondary ambient air quality standard for the pollutant (42 USC Chapter 85 – Air Pollution Prevention and Control). [2]Community engagement is defined as “the process of working collaboratively with groups of people who are affiliated by geographic proximity, special interests, or similar situations with respect to issues affecting their well-being.” CTSA Consortium and the Community Engagement Key Function Committee. Principles of Community Engagement Second Ed. NIH Publication (No. 11-7782). 2011. [3]Climate change adaptation refers to actions being taken to lessen the impact on health and the environment due to changes that cannot be prevented through mitigation. Climate change mitigation refers to actions being taken to reduce greenhouse gas emissions and to enhance the sinks that trap or remove carbon from the atmosphere to reduce the extent of global climate change. A Human Health Perspective On Climate Change: A Report Outlining the Research Needs on the Human Health Effects of Climate Change. 2010 [4] Though Health Impact Assessment is a generic tool, its foundation has the capability to enhance many environmental justice issues. It provides a framework to systematically approach health, disparities, and vulnerable populations in decision-making processes. [5] There are a number of existing tools for conducting community health assessments, including MAPP, PATCH, and PACE EH, that could be used or modified for this purpose. 1U.S. Department of Health and Human Services (HHS), “U.S. Department of Health and Human Services Strategic Plan Fiscal Years 2010 -2015.” http://www.hhs.gov/secretary/about/priorities/strategicplan2010-2015.pdf 2Institute of Medicine (IOM).Leading Health Indicators for Healthy People 2020: Letter Report. Washington, DC: The National Academies Press, 2011. 3Commission on Social Determinants of Health (CSDH). Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health. Geneva: World Health Organization, 2008. 4County Health Rankings – Robert Wood Johnson Foundation and University of Wisconsin Population Health Institute. http://www.countyhealthrankings.org/health-factors/built-environment 5The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. “Phase I Report Recommendations for the Framework and Format of Healthy People 2020.” http://healthypeople.gov/2020/about/advisory/PhaseI.pdf 6 Centers for Disease Control and Prevention (CDC). Health Disparities and Inequalities Report – United States, 2011. MMWR Supplement 60(2011):1-113 7Robert Wood Johnson Foundation. Where We Live Matters for Our Health: Neighborhoods and Health. Issue Brief Series: Exploring the Social Determinants of Health Neighborhoods and Health. Princeton, NJ: RWJF, 2011. 8] Evans, G. The Built Environment and Mental Health. Journal of Urban Health 80(2003): 536-555. 9 Galea, S., et al. Urban Built Environment and Depression: A Multilevel Analysis. Journal of Epidemiology and Community Health 59(2005): 822-827. 10Miodovnik, A. Environmental Neurotoxicants and Development Brain. Mt Sinai Journal of Medicine 78(2011):58–77. 11Satcher, D., Friel, S., and Bell, R. Natural and Manmade Disasters and Mental Health. Journal of the American Medical Association 298(2007): 2540-2542. [12]World Health Organization (WHO). “Preventing Disease Through Healthy Environments: Towards an Estimate of the Environmental Burden of Disease.” http://www.who.int/quantifying_ehimpacts/publications/preventingdisease.pdf 13Transande, L. and Liu, Y. Reducing the Staggering Costs of Environmental Disease in Children, Estimated at $76.6 Billion in 2008. Health Affairs 30(2011):863-870. 14Gee. G. and Payne-Sturges, D.C. Environmental Health Disparities: A Framework Integrating Psychosocial and Environmental Concepts. Environmental Health Perspectives 112(2004):1645-1653. 15Brown P. Race, Class, and Environmental Health: A Review and Systematization of the Literature. Environmental Research 69(1995):15-30. 16U.S. Environmental Protection Agency (EPA). “Environmental Justice.” http://www.epa.gov/environmentaljustice 17Brulle, R.J and Pellow, D.N. Health Environmental Justice: Human Health and Environmental Inequalities. Annual Review of Public Health 27(2006): 103-124. 18U.S. General Accounting Office (GAO), Siting of Hazardous Waste Landfills and Their Correlation with Racial and Economic Status of Surrounding Communities. Washington, DC: U.S. GAO, 1983. 19United Church of Christ Commission for Racial Justice. Toxic Wastes and Race in the United States: A National Study on the Racial and Socio-Economic Characteristics of Communities Surrounding Hazardous Waste Sites. New York: United Church of Christ, 1987. 20Executive Order No. 12898, 59 Fed. Reg. 7629 (Feb. 11, 1994) 21U.S. Department of Health and Human Services (HHS) 1995 Environmental Justice Strategy, Washington, DC: U.S. DHHS, 1995. 22Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics 117(2006):417-424. 23Robert Wood Johnson Foundation. Work Matters for Health. Issue Brief Series: Exploring the Social Determinants of Health Neighborhoods and Health. Princeton, NJ: RWJF, 2011. 24Landrigan, P. Rauh, V.A., and Galvez, M. Environmental Justice and the Health of Children. Mount Sinai Journal of Medicine 77(2010):78-187. 25Robert Wood Johnson Foundation. Work Matters for Health. Issue Brief Series: Exploring the Social Determinants of Health: Work and Health. Princeton, NJ: RWJF, 2011. 26Shields LM, et.al. Navajo birth outcomes in the Shiprock uranium mining area. Health Physics 63(1992):542-51. 27 Tanner CM, et.al. Rotenone, Paraquat and Parkinson's disease. Environmental Health Perspectives 119(2011):866-872. 28Donham, K. et. al. Community Health and Socioeconomic Issues Surrounding Concentrated Animal Feeding Operations. Environmental Health Perspectives 115(2007):317-320. 29Balbus, JM and Malina, C. Identifying Vulnerable Subpopulations for Climate Change Health Effects in the United States. Environmental Defense Fund 51(2009):33-37. 30Thomas R. K., Melillo, J.M. and Peterson, T.C. (Eds). Global Climate Change Impacts in the United States, New York: Cambridge University Press, 2009. 31Portier, C.J., et.al. A Human Health Perspective On Climate Change: A Report Outlining the Research Needs on the Human Health Effects of Climate Change. Research Triangle Park, NC: Environmental Health Perspectives/National Institute of Environmental Health Sciences, 2010. 32Sastry, N. and Landingham, M. One Year Later: Mental Illness Prevalence and Disparities among New Orleans Residents Displaced by Hurricane Katrina. American Journal of Public Health 99(2009): S725–S731. 33Federal Interagency Working Group on Environmental Justice (IWG). “Memorandum of Understanding on Environmental Justice and Executive Order 12898.” http://www.epa.gov/compliance/ej/resources/publications/interagency/ej-mou-2011-08.pdf 34Exec. Order No.13166, 65 Fed. Reg. 20938 (Aug. 16, 2000). 35 Section 504 of the Rehabilitation Act of 1973, as amended, 29 U.S.C. § 794. 36Section 508 of the Rehabilitation Act of 1973, as amended, 29 U.S.C. § 794d. 37Exec. Order No.13175, 65 Fed. Reg. 29003 (Nov. 6, 2000). 38Exec. Order No.13567, 76 Fed. Reg. 15181 (Jun. 13, 2011). 39Title VI of the Civil Rights Act of 1964, 42 U.S.C. 2000d, et seq. 40Institute of Medicine (IOM). Toward Environmental Justice: Research, Education, and Health Policy Needs. Washington, DC. The National Academies Press, 1999. [41]Patient Protection and Affordable Care Act of 2010, Pub. L. No. 111-148, 124 Stat.119 (2010). 42Centers for Disease Control and Prevention (CDC).“Community Transformation Grants (CTGs).” http://www.cdc.gov/communitytransformation/ 43 National Prevention, Health Promotion and Public Health Council. “National Prevention Strategy.” http://www.healthcare.gov/prevention/nphpphc/strategy/report.pdf 44U.S. Department of Health and Human Services (HHS).Office of Disease Prevention and Health Promotion, Healthy People 2020. www.healthypeople.gov 45U.S. Department of Health and Human Services (HHS), Office of Minority Health.” National Partnership for Action to End Health Disparities.” http://www.minorityhealth.hhs.gov/npa/templates/browse.aspx?&lvl=2&lvlid=34 46Let’s Move! “Let’s Move: America’s Move to Raise a Healthier Generation of Kids.” www.letsmove.gov. 47America’s Great Outdoors. “America’s Great Outdoors: A Promise to Future Generations.” http://americasgreatoutdoors.gov/. 48 U.S. Department of Health and Human Services (HHS). “2011 Strategic Sustainability Performance Plan.” http://www.hhs.gov/about/sustainability/2011plan_summary.html 49 Exec. Order No, 13514, 74 Fed. Reg. 52117 (Oct. 8, 2009). 50U.S. Department of Health and Human Services (HHS).Office of the Assistant Secretary for Preparedness and Response. “National Health Security Strategy.” http://www.phe.gov/Preparedness/planning/authority/nhss/strategy/Documents/nhss-final.pdf 51Ross, H.E. Using NEPA in the Fight for Environmental Justice. William & Mary Environmental Law & Policy Review 18(1994): 353-374. 52U.S. Commission on Civil Rights. Not in My Backyard: Executive Order 12898 and Title VI as Tools for Achieving Environmental Justice. Washington, DC: U.S. Commission on Civil Rights. 2003. 53National Environmental Policy Act, 42 U.S.C. Chapter 55, Section 4321. 54U.S. Council on Environmental Quality (CEQ). Environmental Justice: Guidance Under the National Environmental Policy Act. Washington, DC: U.S. CEQ. 1997. 55U.S Department of Health and Human Services (HHS). 2010 Strategic Sustainability Performance Plan. Washington, DC: U.S. HHS, 2010. 56U.S. Council on Environmental Quality, “Interagency Climate Change Adaptation Task Force.” http://www.whitehouse.gov/administration/eop/ceq/initiatives/adaptation 57National Wildlife Federation. Facing the Storm: Indian Tribes, Climate-Induced Weather Extremes, and the Future for Indian Country: National Wildlife Federation 2011 Report. Boulder, CO: National Wildlife Federation, 2011. 58Johnson, D.P., Wilson, J.S. and Luber, G.C. Socioeconomic Indicators of Heat-Related Health Risk Supplemented with Remotely Sensed Data. International Journal of Health Geographics 8(2009):1-13. [59]Stahl, T., Wismar, M., Ollila, E., Lahtinen, E., Leppo, K., editors. Health in All Policies: Prospects and potentials: European Observatory on Health Systems and Policy; Ministry of Social Affairs and Health, Finland; 2006. [60]National Conversation on Public Health and Chemical Exposures. “Education and Communication Work Group Report.” http://www.nationalconversation.us/docs/national-conversation-document-library/education_and_communication_final_report.pdf 61 National Conversation on Public Health and Chemical Exposures. “Addressing Public Health and Chemical Exposures: An Action Agenda.” http://www.nationalconversation.us/docs/national-conversation-document-library/national-conversation-action-agenda.pdf?Status=Master 62Maantay, J. Mapping Environmental Injustices: Pitfalls and Potential of Geographic Information Systems in Assessing Environmental Health and Equity. Environmental Health Perspectives 110(2002): 161–171. 63Bullard, R.D., Mohai, P., Saha, R., and Wright, B. Toxic Wastes and Race at Twenty 1987-2007. The United Church of Christ (2007):1-160. 64Sexton, K., and Linder, S.H. The Role of Cumulative Risk Assessment in Decisions About Environmental Justice. International Journal of Environmental Research and Public Health 7(2010):4037-4049. 65Su, J.G., Morello-Frosch, R., Jesdale, B.M., Kyle, A.D., Shamasunder, B., and Jerrett, M. An Index for Assessing Demographic Inequalities in Cumulative Environmental Hazards with Application to Los Angeles, California. Environmental Science Technology 43(2009):7626–7634. 66Agency for Toxic Substances and Disease Registry. “Toxicological Profile for Lead.” http://www.atsdr.cdc.gov/ToxProfiles/tp13.pdf 67Chakraborty, J., Maantay, J.A., and Brender JD. Disproportionate Proximity to Environmental Health Hazards: Methods, Models, and Measurement. American Journal of Public Health (2011):e1-e10. 68Institute of Medicine (IOM). The Future of the Public’s Health in the 21st Century. Washington, DC: The National Academies Press, 2003. 69National Association of Community Health Centers, Inc. “Access Denied: A Look at America’s Medically Disenfranchised.” http://www.graham-center.org/PreBuilt/Access_Denied.pdf 70Agency for Healthcare Research and Quality (AHRQ). “National Healthcare Disparities Report, 2008.” www.ahrq.gov/qual/measurix.htm 71U.N Committee on the Elimination of Racial Discrimination. “Unequal Health Outcomes in the United States: Racial and Ethnic Disparities in Health Care Treatment and Access, The Role of Social and Environmental Determinants of Health, and the Responsibility of the State.” http://www.prrac.org/pdf/CERDhealthEnvironmentReport.pdf 72Lee, C. Environmental Justice: Building a unified vision of health and the environment. Environmental Health Perspectives 110(2002):141–144. 73 Brookings Institute. Partnering with Communities: Federal Models of Community-Based Programs. Washington, DC: Brookings Institute, 2010. Appendix AHHS Environmental Justice Stakeholder Engagement HHS participated in and facilitated several events and meetings to seek public input on the 2012 HHS Environmental Justice Strategy. HHS participated in all of the Interagency Working Group on Environmental Justice (EJ IWG) stakeholder listening sessions and served as the Federal agency host for the EJ IWG stakeholder meetings in Boston, Iowa, and Chicago. HHS also hosted an Environmental Justice listening session in Mobile, Alabama, sponsored an Environmental Justice Webinar, and hosted an Environmental Justice Thought Leaders Meeting in Washington, DC. A list of environmental justice stakeholder meetings that HHS participated in is included in the table below.
Appendix BGlossary of TermsAffordable Care Act – Health reform legislation that was signed into law in March 2010, putting in place comprehensive health insurance reforms to expand access to health insurance and health care, lower health care costs, and enhance the quality of health care for all Americans. Patient Protection and Affordable Care Act of 2010, 42 U.S.C. 18001, et seq. Built Environment – Human-made (versus natural) resources and infrastructure designed to support human activity, such as buildings, roads, parks, and other amenities. Climate Change Adaptation – Refers to actions being taken to lessen the impact on health and the environment due to changes that cannot be prevented through mitigation. Climate Change Mitigation – Refers to actions being taken to reduce greenhouse gas emissions and to enhance the sinks that trap or remove carbon from the atmosphere to reduce the extent of global climate change. Community-Based Participatory Research – An applied collaborative approach that enables community residents to more actively participate in the full spectrum of research (from conception – design – conduct – analysis – interpretation – conclusions – communication of results) with a goal of influencing change in community health, systems, programs or policies. Community Engagement – The process of working collaboratively with and through groups of people affiliated by geographic proximity, special interest, or similar situations to address issues affecting the well-being of those people. It is a powerful vehicle for bringing about environmental and behavioral changes that will improve the health of the community and its members. It often involves partnerships and coalitions that help mobilize resources and influence systems, change relationships among partners, and serve as catalysts for changing policies, programs, and practices. Community Health Assessment – Community health assessment is a call for regularly and systematically collecting, analyzing, and making available information on the health of a community, including statistics on health status, community health needs, epidemiologic and other studies of health problems. Often this can take the form of community needs assessments, which are intended to assist the community in adapting and responding to important health problems and risks. Increasingly, moving beyond problems and deficits toward an analysis of community strengths and resources is becoming recognized as a critical part of understanding a community’s health. Cumulative Impacts – The impact on the environment which results from the incremental impact of the action when added to other past, present, and reasonably foreseeable future actions regardless of what agency (Federal or non-Federal) or person undertakes such other actions. Cumulative impacts can result from individually minor but collectively significant actions taking place over a period of time. Cumulative Environmental Exposure – Exposure to one or more chemical, biological, physical, or radiological agents across environmental media (e.g., air, water, soil) from single or multiple sources, over time in one or more locations, that have the potential for deleterious effects to the environment and/or human health. Disproportionately high and adverse environmental effects – When determining whether environmental effects are disproportionately high and adverse, agencies are to consider the following three factors to the extent practicable:
Council on Environmental Quality, Executive Office of the President. Environmental Justice: Guidance Under the National Environmental Policy Act. Washington, DC: Executive Office of the President; 10 Dec 1997, pages 25-30. Disproportionately high and adverse human health effects – When determining whether human health effects are disproportionately high and adverse, agencies are to consider the following three factors to the extent practicable:
Council on Environmental Quality, Executive Office of the President. Environmental Justice: Guidance Under the National Environmental Policy Act. Washington, DC: Executive Office of the President; 10 Dec 1997, pages 25-30. Environmental Assessment – (a) A concise public document for which a Federal agency is responsible that serves to (1) briefly provide sufficient evidence and analysis for determining whether to prepare an environmental impact statement (EIS) or a finding of no significant impact (FONSI), (2) aid an agency’s compliance with the National Environmental Policy Act when no EIS is necessary and (3) facilitate preparation of an EIS when one is necessary. (b) Includes brief discussions of the need for the proposal, of alternatives as required by section 102(2)(3), of the environmental impacts of the proposed action and alternatives, and a listing of agencies and persons consulted. Environmental Exposure – Contact with a substance by swallowing, breathing, or touching the skin or eyes. Exposure may be short-term [acute exposure], of intermediate duration, or long-term [chronic exposure]. Environmental Hazard – Situations or materials that pose a threat to human health and safety in the built or natural environment, as well as to the health and safety of other animals and plants, and to the proper functioning of an ecosystem, habitat, or other natural resource. Environmental Health – Environmental health addresses all the physical, chemical, and biological factors external to a person, and all the related factors impacting behaviors. It encompasses the assessment and control of those environmental factors that can potentially affect health. It is targeted towards preventing disease and creating health-supportive environments. This definition excludes behavior not related to environment, as well as behavior related to the social and cultural environment, and genetics. Environmental Impact Statement (EIS) – An EIS is a detailed analysis that serves to insure that the policies and goals defined in the National Environmental Policy Act (NEPA) are infused into the ongoing programs and actions of the federal agency. EISs are generally prepared for projects that the proposing agency views as having significant prospective environmental impacts. The EIS should provide a discussion of significant environmental impacts and reasonable alternatives (including a No Action alternative) which would avoid or minimize adverse impacts or enhance the quality of the human environment. The formal decision document resulting from a completed EIS is termed a “Record of Decision” (ROD). Environmental Justice – The fair treatment and meaningful involvement of all people regardless of race, color, national origin, or income with respect to the development, implementation, and enforcement of environmental laws, regulations, and policies. Environmental Stressor – Physical, chemical, or biological entities that can induce adverse effects on ecosystems or human health. Executive Order 12898 – Executive Order entitled Federal Actions to Address Environmental Justice in Minority and Low-Income Populations (1994), requiring each Federal agency to make achieving environmental justice part of its mission by identifying and addressing, as appropriate, disproportionately high and adverse human health or environmental effects of its programs, policies, and activities on minority and low-income populations in the United States and its territories and possessions, the District of Columbia, the Commonwealth of Puerto Rico, and the Commonwealth of the Mariana Islands. Executive Order 13514 – Executive Order entitled Federal Leadership in Environmental, Energy, and Economic Performance (2009), establishing an integrated strategy towards sustainability in the Federal government and making reduction of greenhouse gas emissions a priority for Federal agencies. The Executive Order requires all Federal agencies to minimize the environmental impacts of their activities and to strengthen the vitality and livability of the communities in which Federal facilities are located. Fair Treatment – No group of people, including racial, ethnic, or socioeconomic group should bear a disproportionate share of the negative environmental consequences resulting from industrial, municipal, and commercial operations or the execution of federal, state, local and tribal programs or policies. Health Disparities – A particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage. Health disparities adversely affect groups of people who have systematically experienced greater obstacles to health based on their racial or ethnic group; religion; socioeconomic status; gender; age; mental health; cognitive, sensory, or physical disability; sexual orientation or gender identity; geographic location; or other characteristics historically linked to discrimination or exclusion. Health Equity – Attainment of the highest level of health for all people. Achieving health equity requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and the elimination of health and health care disparities. Health Impact Assessment (HIA) – HIA is a systematic process that uses an array of data sources and analytic methods and considers input from stakeholders to determine the potential effects of a proposed policy, plan, program, or project on the health of a population and the distribution of those effects within the population. HIA provides recommendations on monitoring and managing those effects. Healthy People – Initiative that provides science-based, 10-year national objectives for improving the health of all Americans. HHS Action Plan to Reduce Racial and Ethnic Health Disparities – The HHS Action Plan to Reduce Racial and Ethnic Health Disparities provides a coordinated roadmap for a nation free of disparities in health and healthcare. It identifies and promotes integrated approaches, evidence-based programs, and best practices to reduce health disparities. HHS Strategic Sustainability Performance Plan (SSPP) – The HHS Strategic Sustainability Performance Plan, established under Executive Order 13514, affirms that sustainability is integral to the HHS mission, to protect the health of all Americans and provide essential human services, especially for those who are least able to help themselves. Sustainability has been defined as “the enduring prosperity of all living things” and by this measure, is directly linked to the health of humans, the health of the environment, and the health of economic systems that support and promote our well-being. This linkage of human health, environmental health and economic health is referred to as the triple health bottom line and is integral to HHS’s mission and the sustainability mandates of Executive Order (EO) 13514. The HHS SSPP establishes an integrated strategy to move HHS towards sustainability. Meaningful Involvement – (1) Potentially affected community residents have an appropriate opportunity to participate in decisions about a proposed activity that will affect their environment and/or health; (2) the public contribution can influence the regulatory agency’s decision; (3) the concerns of all participants involved will be considered in the decision making process; and (4) the decision makers seek out and facilitate the involvement of those potentially affected. Memorandum of Understanding on Environmental Justice and Executive Order 12898 - Multiple Environmental Exposure – Exposure to any combination of two or more chemical, biological, physical or radiological agents (or two or more agents from two or more of these categories) from single or multiple sources that have the potential for deleterious effects to the environment and/or human health. National Environmental Policy Act (NEPA) – An environmental law enacted in 1970 that requires Federal agencies to integrate environmental values into their decision making processes by considering the environmental impacts of their proposed actions and reasonable alternatives to those actions. National Health Security Strategy (NHSS) – The NHSS is the first comprehensive strategy focusing specifically on the Nation’s goals of protecting people’s health in the case of an emergency. The purpose of the NHSS is to guide the Nation’s efforts to minimize the risks associated with a wide range of potential large-scale incidents that put the health and well-being of the Nation’s people at risk, whether at home, in the workplace, or in any other setting. National health security is a state in which the Nation and its people are prepared for, protected from, and resilient in the face of health threats or incidents with potentially negative health consequences. National Prevention Strategy – The National Prevention Strategy, called for in the Affordable Care Act, is a comprehensive plan to increase the number of Americans who are healthy at every stage of life. It aims to guide our nation in the most effective and achievable means for improving health and well-being. The Strategy prioritizes prevention by integrating recommendations and actions across multiple settings to improve health and save lives. Natural Environment – Components of the environment that includes plants, atmosphere, weather, and topography. Occupational Safety and Health – All aspects of workers’ health, including primary prevention of occupational hazards, protection and promotion of health at work, employment conditions, and a better response from health systems to workers’ health. Physical Environment – Includes the natural environment (i.e., plants, atmosphere, weather, and topography) and the built environment (i.e., buildings, spaces, transportation systems, and products that are created or modified by people). Physical environments can consist of particular individual or institutional settings, such as homes, worksites, schools, health care settings, or recreational settings. Surrounding neighborhoods and related community areas where individuals live, work, travel, play, and conduct their other daily activities are elements of the physical environment. Racial/Ethnic Minority – 1) The term racial and ethnic minority group means American Indians (including Alaskan Natives, Eskimos, and Aleuts); Asian Americans; Native Hawaiians and other Pacific Islanders; Blacks; and Hispanics. 2) The term Hispanic means individuals whose origin is Mexican, Puerto Rican, Cuban, Central or South American, or any other Spanish-speaking country. Social Determinants of Health – The conditions in which people are born, grow, live, work and age, including the health system. These circumstances are shaped by the distribution of money, power and resources at global, national and local levels, which are themselves influenced by policy choices. Social Environment – Includes interactions with family, friends, coworkers, and others in the community, as well as societal attitudes, norms, and expectations. It encompasses social relationships and policies within settings such as schools, neighborhoods, workplaces, businesses, places of worship, health care settings, recreation facilities, and other public places. It includes the social aspects of health-related behaviors (e.g., tobacco use, substance use, physical activity) in the community. It also encompasses social institutions, such as law enforcement and governmental as well as non-governmental organizations. Economic policy is one important component of the social environment. Sustainability – The enduring prosperity of all living things. Title VI of the Civil Rights Act of 1964 – Federal law that states that no person in the United States shall on the ground of race, color, or national origin, be excluded from participation in, be denied the benefits of, or be otherwise subjected to discrimination under any program or activity receiving Federal financial assistance. Vulnerable Populations – Vulnerable populations include the uninsured, the poor, the elderly, children, those living with mental or physical disabilities, racial and ethnic minorities, and the terminally ill. The vulnerability that these groups experience usually can be attributed to one or some combination of three factors: economic status or geographic location; health, functional, or developmental status; or ability to communicate. Appendix CAcronyms
Appendix DU.S. Department of Health and Human Services (HHS) |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Every American deserves to have a clean, safe and healthy environment. Today, we understand better than ever before that our health is not only dependent on what happens in the doctor’s office but is determined by the air we breathe, the water we drink and the communities we call home. Over the past two years, the Administration and our agency have taken unprecedented steps to ensure strong protection from environmental and health hazards for all Americans.
Every American deserves to have a clean, safe and healthy environment. Today, we understand better than ever before that our health is not only dependent on what happens in the doctor’s office but is determined by the air we breathe, the water we drink and the communities we call home. Over the past two years, the Administration and our agency have taken unprecedented steps to ensure strong protection from environmental and health hazards for all Americans.