Multistate Outbreak of Listeriosis Linked to Whole Cantaloupes from Jensen Farms, Colorado
August 27, 2012 (FINAL Update Addendum)
On this Page
Outbreak Highlights
- This multistate outbreak of Listeria monocytogenes infections (listeriosis) ended in October, 2011.
- After the final update on December 8, a fifth outbreak-associated subtype of Listeria was isolated from a sample of cantaloupe collected during the investigation.
- The fifth subtype matches that of Listeria isolated from one patient. This patient's illness had been reported, but had not previously been linked to the outbreak. Therefore, this case has been added to the number of outbreak-associated illnesses. This brings the total number of outbreak-associated illnesses to 147 persons infected with any of the five outbreak-associated subtypes of Listeria. These persons lived in 28 states.
- The number of outbreak-associated deaths has increased by three since December 8, 2011. In total, 33 deaths from outbreak-associated cases of listeriosis have been reported to CDC. In addition, one woman pregnant at the time of illness had a miscarriage.
- Ten other deaths not attributed to listeriosis occurred among persons who had been infected with an outbreak-associated subtype. State and local public health officials reviewed causes of death listed on death certificates to determine whether to attribute these deaths to listeriosis. Deaths included in this review occurred as recently as February 29, 2012.
- Go to August 27, 2012 for a full report.
- Timeline of Events: Multistate Outbreak of Listeriosis Linked to Whole Cantaloupes from Jensen Farms, Colorado—United States, 2011
- Listeria is a rare but important cause of human illness in the United States. More information about listeriosis and recommendations to reduce the risk of getting listeriosis from food are available at CDC's Listeriosis webpage.
- For more information on multistate foodborne disease outbreaks, please visit CDC's Multistate Foodborne Outbreaks page.
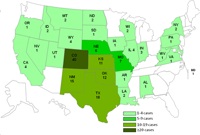
Case Count Map
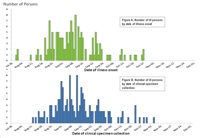
Epi Curve
Timeline of Events
Note: The final update for the investigation was published online on December 8, 2011. CDC has published this addendum to provide updated final numbers of outbreak-associated illnesses and deaths.
Introduction
CDC collaborated with public health officials in numerous states, including Colorado, as well as the U.S. Food and Drug Administration (FDA) to investigate a multistate outbreak of listeriosis that occurred from August through October, 2011. Listeriosis is a serious infection usually caused by eating food contaminated with the bacterium Listeria monocytogenes. Investigators used DNA analysis of Listeria bacteria isolated from patients to identify cases of illness that may have been part of this outbreak. The Listeria bacteria were obtained from diagnostic testing; pulsed-field gel electrophoresis (PFGE) was used to determine DNA fingerprint patterns. Investigators used data from PulseNet, the national subtyping network made up of state and local public health laboratories and federal food regulatory laboratories that performs molecular surveillance of foodborne infections.
After the final update on December 8, investigators learned that a Listeria isolate that had been isolated from a sample of cut cantaloupe from a patient’s home during the outbreak investigation had a PFGE pattern combination that was different from the four known pattern combinations in the outbreak. A search of the PulseNet database for matching DNA fingerprint patterns from isolates collected during the outbreak time period identified one human matching isolate. The person from whom the Listeria was isolated reported eating cantaloupe before becoming ill; this case was added to the case count.
A total of 147 persons infected with any of the five outbreak-associated subtypes of Listeria monocytogenes were reported to CDC from 28 states. The number of infected persons identified in each state was as follows: Alabama (1), Arkansas (1), California (4), Colorado (40), Idaho (2), Illinois (4), Indiana (3), Iowa (1), Kansas (11), Louisiana (2), Maryland (1), Missouri (7), Montana (2), Nebraska (6), Nevada (1), New Mexico (15), New York (2), North Dakota (2), Oklahoma (12), Oregon (1), Pennsylvania (1), South Dakota (1), Texas (18), Utah (1), Virginia (1), West Virginia (1), Wisconsin (2), and Wyoming (4).
Among persons for whom information was available, reported illness onset ranged from July 31, 2011 through October 27, 2011. Ages ranged from <1 to 96 years, with a median age of 78 years. Most ill persons were over 60 years old. Fifty-eight percent of ill persons were female. Among the 145 ill persons with available information on whether they were hospitalized, 143 (99%) were hospitalized. Thirty-three outbreak-associated deaths were reported: Colorado (9), Indiana (1), Kansas (3), Louisiana (2), Maryland (1), Missouri (3), Montana (1), Nebraska (1), New Mexico (5), New York (2), Oklahoma (1), Texas (2), and Wyoming (2). Among persons who died, ages ranged from 48 to 96 years, with a median age of 81 years. In addition, one woman pregnant at the time of illness had a miscarriage. Ten deaths not attributed to listeriosis occurred among persons who had been infected with an outbreak-associated subtype. State and local public health officials reviewed causes of death listed on death certificates to determine whether to attribute these deaths to listeriosis. Deaths included in this review occurred as recently as February 29, 2012.
Seven of the illnesses were related to a pregnancy; three were diagnosed in newborns and four were diagnosed in pregnant women. One miscarriage was reported.
The outbreak can be visually described with a chart showing the number of persons who became ill each day. This chart is called an epidemic curve or epi curve. Please see the description of the steps in a foodborne outbreak investigation for more details.
About 800 laboratory-confirmed cases of Listeria infection are reported each year in the United States and typically 3 or 4 outbreaks are identified. The foods that typically cause these outbreaks have been Mexican-style soft cheeses made with unpasteurized milk, deli meats, and hot dogs. In the past, produce was not often identified as a source, but sprouts caused an outbreak in 2009, and precut celery caused an outbreak in 2010.
Investigation of the Outbreak
Collaborative investigations by local, state, and federal public health and regulatory agencies indicated that the source of the outbreak was whole cantaloupe grown at Jensen Farms’ production fields in Granada, Colorado. Among the 144 ill persons with available information on what they ate, 134 (93%) reported consuming cantaloupe in the month before illness onset. Several ill persons remembered the type of cantaloupes they had eaten and said they were Rocky Ford cantaloupes, which are grown in the Rocky Ford region of southeastern Colorado. Source tracing of the cantaloupes that ill persons ate indicated that they came from Jensen Farms, and were marketed as being from the Rocky Ford region. These cantaloupes were shipped from July 29 through September 10 to at least 24 states , with possible further distribution.
The Colorado Department of Public Health and Environment isolated Listeria monocytogenes from cantaloupe samples collected from grocery stores and from ill persons’ homes. Colorado state officials determined that these cantaloupes came from Jensen Farms. FDA isolated Listeria monocytogenes outbreak subtypes from samples from equipment and cantaloupe from the Jensen Farms’ packing facility in Granada, Colorado. FDA worked closely with CDC, the firms involved, and public health authorities in states where illnesses occurred to determine the cause of contamination. Cantaloupes from other farms were not linked to this outbreak
Clinical Features/Signs and Symptoms
Listeriosis is a serious infection caused by eating food contaminated with the bacterium Listeria monocytogenes. The disease primarily affects older adults, persons with weakened immune systems, pregnant women, and newborns. Less commonly, persons without these risk factors can be affected.
A person with listeriosis usually has fever and muscle aches, often preceded by diarrhea or other gastrointestinal symptoms. Almost everyone who is diagnosed with listeriosis has invasive infection (meaning that the bacteria spread from their intestines to the bloodstream or other body sites).
Listeriosis is treated with antibiotics. Persons in the high-risk category, including older adults, persons with weakened immune systems, and pregnant women, who experience flu-like symptoms within 2 months after eating contaminated food should seek medical care and tell the physician or health care provider about eating the contaminated food.
The symptoms vary with the infected person:
- High-risk persons other than pregnant women: Symptoms can include fever, muscle aches, headache, stiff neck, confusion, loss of balance, and convulsions.
- Pregnant women: Pregnant women typically experience only a mild, flu-like illness. However, infection during pregnancy can lead to miscarriage, stillbirth, premature delivery, or life-threatening infection of the newborn.
- Healthy persons. Healthy persons occasionally develop invasive listeriosis. In addition, persons exposed to a very large dose of Listeria bacteria can develop a non-invasive illness (meaning that the bacteria do not spread into their blood stream or other sites) with diarrhea and fever.
If a person has eaten food contaminated with Listeria bacteria and does not have any symptoms, most experts believe that no tests or treatment are needed, even for persons at higher risk for listeriosis.
More general information about listeriosis can be found at the CDC's Listeriosis webpage.
Recall
On September 14, 2011, FDA issued a press release to announce that Jensen Farms issued a voluntary recall of its Rocky Ford-brand cantaloupes after they were linked to a multistate outbreak of listeriosis. On September 23, 2011, FDA issued a press release to announce a recall from Carol’s Cuts LLC, a Kansas food processor. The company recalled 594 pounds of fresh-cut cantaloupe, which were packaged in 5-pound trays as chunks and as an ingredient in an 8-ounce mixed fruit medley, because the cantaloupes originated from Jensen Farms. On October 6, FDA posted a press release that announced a recall from Fruit Fresh Up, Inc., a New York food processor. The company recalled 4,800 individual packages of fresh cut cantaloupe and cut mixed fruit containing cantaloupe, because the cantaloupe originated from Jensen Farms. The fresh cut fruit subject to this recall was sold between August 31 and September 11, 2011.
Advice to Consumers
This outbreak is over. However, Listeria is still an important cause of human illness in the United States.
Who is most at risk?
- Listeriosis primarily affects older adults, persons with weakened immune systems, pregnant women, and newborns.
- Persons who think they might have become ill from eating contaminated food should consult their doctor immediately if they have symptoms. People can develop listeriosis up to two months after eating contaminated food.
- Recommendations for preventing listeriosis from foods other than cantaloupes are available at CDC's Listeriosis webpage on prevention.
For more information about listeriosis and recommendations to reduce your risk of getting listeriosis go to CDC's Listeriosis webpage on prevention.
For more information on produce safety go to FDA's Produce Safety webpage
Key Resources
CDC's Role in Food Safety
CDC leads federal efforts to gather data on foodborne illnesses, investigate foodborne outbreaks and monitor the effectiveness of prevention and control efforts. CDC is not a food safety regulatory agency but works closely with the food safety regulatory agencies, in particular, with FDA and U.S. Department of Agriculture's Food Safety and Inspection Service. CDC also plays a key role in building state and local health department epidemiology, laboratory and environmental health capacity to support foodborne disease surveillance and outbreak response. Notably, CDC data can be used to help document the effectiveness of regulatory interventions.
Previous Updates
Contact Us:
- Centers for Disease Control and Prevention
1600 Clifton Rd
Atlanta, GA 30333 - 800-CDC-INFO
(800-232-4636)
TTY: (888) 232-6348 - New Hours of Operation
8am-8pm ET/Monday-Friday
Closed Holidays - cdcinfo@cdc.gov