Topics in Brief: Comorbid Drug Abuse and Mental Illness
Revised October 2007
What is Comorbidity and What Are Its Causes?
When two disorders or illnesses occur simultaneously in the same person, they are called comorbid. Surveys show that drug abuse and other mental illnesses are often comorbid. Six out of ten people with a substance use disorder also suffer from another form of mental illness. But the high prevalence of these comorbidities does not mean that one condition caused the other, even if one appeared first. In fact, there are at least three scenarios that we should consider:
- Drug abuse can cause a mental illness.
- Mental illness can lead to drug abuse.
- Drug abuse and mental disorders are both caused by other common risk factors.
In reality, all three scenarios can contribute, in varying degrees, to the establishment of specific comorbid mental disorders and addiction.
Why Do Drug Abuse and Mental Disorders Commonly Co-occur?
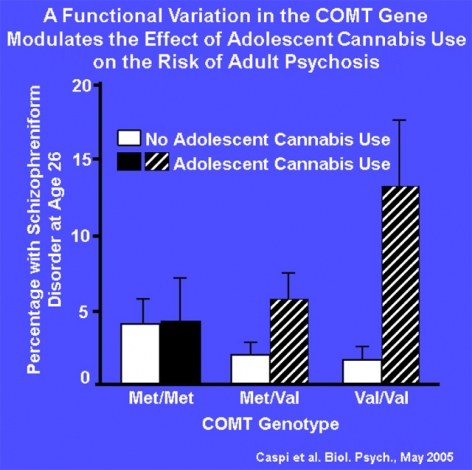 The COMT gene, which is known to modulate the risk for schizophrenia, comes in two forms: "Met" and "Val". The hatched vertical bars in this figure show that individuals with one or two copies of the Val variant are more likely to develop symptoms of psychosis and even schizophrenic-type disorders if they used cannabis during adolescence. This study highlights the complex interactions between genetics, drug exposure, and age of use in the risk for developing a mental disorder.
The COMT gene, which is known to modulate the risk for schizophrenia, comes in two forms: "Met" and "Val". The hatched vertical bars in this figure show that individuals with one or two copies of the Val variant are more likely to develop symptoms of psychosis and even schizophrenic-type disorders if they used cannabis during adolescence. This study highlights the complex interactions between genetics, drug exposure, and age of use in the risk for developing a mental disorder.- Overlapping genetic vulnerabilities. Mounting evidence suggests that common genetic factors may predispose individuals to both mental disorders and addiction or to having a greater risk of the second disorder once the first appears.
- Overlapping environmental triggers. Stress, trauma (e.g., physical or sexual abuse), and early exposure to drugs are common factors that can lead to addiction and to mental illness, particularly in those with underlying genetic vulnerabilities.
- Involvement of similar brain regions. Some areas of the brain are affected by both drug abuse and mental disorders. For example, brain circuits linked to reward processing as well as those implicated in the stress response are affected by abused substances and also show abnormalities in specific mental disorders.
- Drug abuse and mental illness are developmental disorders. They often begin in adolescence or even childhood, periods when the brain is undergoing dramatic developmental changes. Early exposure to drugs of abuse can change the brain in ways that increase the risk for mental illness (figure), just as early symptoms of a mental disorder may increase vulnerability to drug abuse.
How Common Are Comorbid Drug Abuse and Mental Disorders?
Compared with the general population:
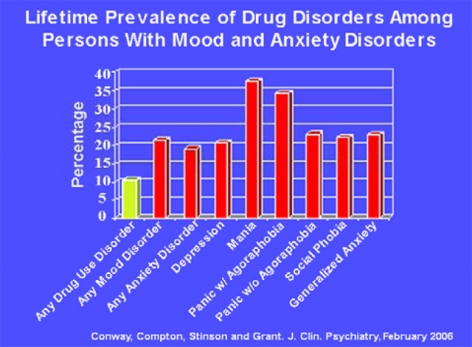
- patients with mood or anxiety disorders are about twice as likely to also suffer from a drug disorder (figure).
- patients with drug disorders are roughly twice as likely to be diagnosed with mood or anxiety disorders.
The rates of specific comorbidities also vary by gender. Among men and women in drug treatment, antisocial personality disorder is more common in men, while women have higher rates of major depression, posttraumatic stress disorder, and other anxiety disorders.
How Can Comorbidity Be Diagnosed and Treated?
The high rate of comorbid substance abuse and mental illness points to the need for a comprehensive approach that identifies, evaluates, and simultaneously treats both disorders. Patients with co-occurring disorders often exhibit more severe symptoms than those caused by either disorder alone, underscoring the need for integrated treatment. Careful diagnosis and monitoring will help ensure that symptoms related to drug abuse (e.g., intoxication, withdrawal) are not mistaken for a discrete mental disorder. Even in people whose comorbidities do not occur simultaneously, research shows that mental disorders can increase vulnerability to subsequent drug abuse and that drug abuse constitutes a risk factor for subsequent mental disorders. Therefore, diagnosis and treatment of one disorder will likely reduce risk for the other, or at least improve its prognosis. The need to develop effective interventions to treat both conditions concurrently is strongly supported by research, but has been difficult to implement in practice because:
- The health care systems in place to treat substance abuse and mental illness are typically disconnected, hence inefficient. Physicians tend to treat patients with mental illnesses, whereas a mix of providers with varying backgrounds deliver drug abuse treatment.
- Some substance abuse treatment centers are biased against using any medications, including those necessary to treat patients with severe mental disorders.
Still, behavioral treatment options customized for a given age group or gender have shown promise for treating drug abuse and mental disorder comorbidities, and research is under way to identify medications targeting both disorders. Clinicians and researchers generally agree that broad-spectrum diagnosis and concurrent therapy (pharmacological and behavioral) will lead to better outcomes for patients with comorbid disorders.
The stigma attached to substance abuse and mental disorders often hinders early diagnosis and proper treatment. Greater understanding resulting from recent scientific findings that substance abuse and mental illness disrupt some of the same brain functions will reduce the social stigma that hinders treatment seeking, quality, and access by patients with either or both conditions.