Learning to breastfeed
- How breast milk is made
- What you can do before you give birth
- Tips for getting off to a good start
- Bringing your baby to the breast to latch
- How often should I breastfeed? How long should feedings be?
- Breastfeeding holds
- Tips for making it work
- Making plenty of milk
- How to know your baby is getting enough milk
- How long should I breastfeed?
- More information on learning to breastfeed
Keep in mind that breastfeeding is a learned skill. It requires patience and practice. For some women, the learning stages can be frustrating and uncomfortable. And some situations make breastfeeding even harder, such as babies born early or health problems in the mother. The good news is that it will get easier, and support for breastfeeding mothers is growing. Keep in mind that you make milk in response to your baby sucking at the breast. The more milk your baby removes from the breasts, the more milk you will make.
How breast milk is made
 |
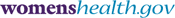
Knowing how the breast works to produce milk can help you understand the breastfeeding process. The breast itself is a gland that is made up of several parts, including:
- Glandular tissue – body tissue that makes and releases one or more substances for use in the body. Some glands make fluids that affect tissues or organs. Others make hormones or assist with blood production. In the breast, this tissue is involved in milk production.
- Connective tissue – a type of body tissue that supports other tissues and binds them together. This tissue provides support in the breast.
- Blood – fluid in the body made up of plasma, red and white blood cells, and platelets. Blood carries oxygen and nutrients to and waste materials away from all body tissues. In the breast, blood nourishes the breast tissue and provides nutrients needed for milk production.
- Lymph – the almost colorless fluid that travels through the lymphatic system and carries cells that help fight infection and disease. Lymph tissue in the breast helps remove waste.
- Nerves – cells that are the building blocks of the nervous system (the system that records and transmits information chemically and electrically within a person). Nerve tissue in the breast makes breasts sensitive to touch, allowing the baby’s sucking to stimulate the let-down or milk-ejection reflex and milk production. Learn more about let-down reflex.
- Fatty tissue – connective tissue that contains stored fat. It is also known as adipose tissue. Fatty tissue in the breast protects the breast from injury. Fatty tissue is what mostly affects the size of a woman’s breast. Breast size does not have an effect on the amount of milk or the quality of milk a woman makes.
Special cells inside your breasts make milk. These cells are called alveoli (al-VEE-uh-leye). When your breasts become fuller and tender during pregnancy, this is a sign that the alveoli are getting ready to work. Some women do not feel these changes in their breasts. Others may sense these changes after their baby is born.
The alveoli make milk in response to the hormone prolactin (proh-LAK-tin). Prolactin rises when the baby suckles. Another hormone, oxytocin (oks-ee-TOH-suhn), causes small muscles around the cells to contract and move the milk through a series of small tubes called milk ducts. This moving of the milk is called let-down reflex. Learn more about let-down reflex.
Oxytocin also causes the muscles of the uterus to contract during and after birth. This helps the uterus to get back to its original size. It also lessens any bleeding a woman may have after giving birth. The release of both prolactin and oxytocin may be responsible in part for a mother’s intense feeling of needing to be with her baby.
A let-down reflex or milk ejection reflex is a conditioned reflex ejecting milk from the alveoli through the ducts to the sinuses of the breast and the nipple. This reflex makes it easier to breastfeed your baby. Let-down happens a few seconds to several minutes after you start breastfeeding your baby. It can happen a few times during a feeding, too. You may feel a tingle in your breast or you may feel a little uncomfortable. Keep in mind that some women don’t feel anything. Let-down can happen at other times, too, such as when you hear your baby cry or when you may just be thinking about your baby. If your milk lets down as more of a gush and it bothers your baby, try expressing some milk by hand before you start breastfeeding.
What you can do before you give birth
A woman who is thinking about how to feed her baby values her partner’s advice. A father’s approval and support of breastfeeding can boost the mother’s confidence and help her to overcome challenges. But supporting a woman’s choice to breastfeed is not the father’s only role. Although the bond between mother and baby is important, so is the bond between father and baby. Babies need cuddles and hugs from their dads, too! In fact, skin-to-skin contact helps baby and father bond much like it does for mother and baby.
To prepare for breastfeeding, the most important thing you can do is have confidence in yourself. Committing to breastfeeding starts with the belief that you can do it!
Other steps you can take to prepare for breastfeeding:
- Get good prenatal care, which can help you avoid early delivery. Babies born too early often need special care, which can make breastfeeding harder.
- Tell your health care provider about your plans to breastfeed, and ask if the place where you plan to deliver your baby has the staff and set-up to support successful breastfeeding. Some hospitals and birth centers have taken special steps to create the best possible environment for successful breastfeeding. They are called Baby-Friendly Hospitals and Birth Centers. Women who deliver in a baby-friendly facility are promised the information and support they need to breastfeed their infants.
- Take a breastfeeding class. Pregnant women who learn about how to breastfeed are more likely to be successful than those who do not. Breastfeeding classes offer pregnant women and their partners the chance to prepare and ask questions before the baby’s arrival.
- Ask your health care provider to recommend a lactation consultant. You can establish a relationship before the baby comes, or be ready if you need help after the baby is born.
- Talk to your health care provider about your health. Discuss any breast surgery or injury you may have had. If you have depression or are taking medications, discuss treatment options that can work with breastfeeding.
- Tell your health care provider that you would like to breastfeed your newborn baby as soon as possible after delivery. The sucking instinct is very strong within the first hour of life.
- Talk to friends who have breastfed or consider joining a breastfeeding support group.
- Talk to fathers, partners, and other
family members about how they
can help. Partners and family members can:
- Support the breastfeeding relationship by being kind and encouraging.
- Show their love and appreciation for all of the work that is put into breastfeeding.
- Be good listeners when a mother needs to talk through breastfeeding concerns.
- Make sure the mother has enough to drink and gets enough rest, help around the house, and take care of other children at home.
- Give emotional nourishment to the child through playing and cuddling.
Tips for getting off to a good start
After you have the baby, these steps can help you get off to a great start:
- Breastfeed as soon as possible after birth.
- Ask for an on-site lactation consultant to come help you.
- Ask the staff not to give your baby other food or formula, unless it is medically necessary.
- Allow your baby to stay in your hospital room all day and night so that you can breastfeed often. Or, ask the nurses to bring you your baby for feedings.
- Try to avoid giving your baby any pacifiers or artificial nipples so that he or she gets used to latching onto just your breast.
Bringing your baby to the breast to latch
Some babies latch on right away and, for some, it takes more time.
When awake, your baby will move his or her head back and forth, looking and feeling for the breast with his or her mouth and lips. The steps below can help you get your baby to “latch” on to the breast to start eating. Keep in mind that there is no one way to start breastfeeding. As long as the baby is latched on well, how you get there is up to you.
- Hold your baby, wearing only a diaper, against your bare chest. Hold the baby upright with his or her head under your chin. Your baby will be comfortable in that cozy valley between your breasts. You can ask your partner or a nurse to place a blanket across your baby’s back and bring your bedcovers over you both. Your skin temperature will rise to warm your baby.
- Support his or her neck and shoulders with one hand and hips with the other. He or she may move in an effort to find your breast.
- Your baby’s head should be tilted back slightly to make it easy to suck and swallow. With his or her head back and mouth open, the tongue is naturally down and ready for the breast to go on top of it.
- Allow your breast to hang naturally. When your baby feels it with his or her cheek, he or she may open his or her mouth wide and reach it up and over the nipple. You can also guide the baby to latch on as you see in the illustrations below.
- At first, your baby’s nose will be lined up opposite your nipple. As his or her chin presses into your breast, his or her wide, open mouth will get a large mouthful of breast for a deep latch. Keep in mind that your baby can breathe at the breast. The nostrils flare to allow air in.
- Do not put your hands on your baby’s head. As it tilts back, support your baby’s upper back and shoulders with the palm of your hand and pull your baby in close.
Getting your baby to latch
 |
1. Tickle the baby’s lips to encourage him or her to open wide. |
 |
2. Pull your baby close so that the chin and lower jaw moves into your breast first. |
 |
3. Watch the lower lip and aim it as far from base of nipple as possible, so the baby takes a large mouthful of breast. |
Click on the start button for a demonstration
Signs of a good latch
A good latch is important for your baby to breastfeed effectively and for your comfort. During the early days of breastfeeding, it can take time and patience for your baby to latch on well.
- The latch feels comfortable to you, without hurting or pinching. How it feels is more important than how it looks.
- Your baby’s chest is against your body and he or she does not have to turn his or her head while drinking.
- You see little or no areola, depending on the size of your areola and the size of your baby’s mouth. If areola is showing, you will see more above your baby’s lip and less below.
- When your baby is positioned well, his or her mouth will be filled with breast.
- The tongue is cupped under the breast, although you might not see it.
- You hear or see your baby swallow. Some babies swallow so quietly, a pause in their breathing may be the only sign of swallowing.
- You see the baby’s ears “wiggle” slightly.
- Your baby’s lips turn out like fish lips, not in. You may not even be able to see the bottom lip.
- Your baby’s chin touches your breast.
Help with latch problems
Are you in pain? Many moms report that their breasts can be tender at first until both they and their baby find comfortable breastfeeding positions and a good latch. Once you have done this, breastfeeding should be comfortable. If it hurts, your baby may be sucking on only the nipple. Gently break your baby’s suction to your breast by placing a clean finger in the corner of your baby’s mouth and try again. Also, your nipple should not look flat or compressed when it comes out of your baby’s mouth. It should look round and long, or the same shape as it was before the feeding.
Are you or your baby frustrated? Take a short break and hold your baby in an upright position. Try holding him or her between your breasts skin-to-skin. Talk, sing, or provide your finger for sucking for comfort. Try to breastfeed again in a little while. Or, the baby may start moving to the breast on his or her own from this position.
Does your baby have a weak suck, or make only tiny suckling movements? Break your baby’s suction and try again. He or she may not have a deep enough latch to remove the milk from your breast. Talk with a lactation consultant or pediatrician if your baby’s suck feels weak or if you are not sure he or she is getting enough milk. Rarely, a health problem causes the weak suck.
How often should I breastfeed? How long should feedings be?
Early and often! Breastfeed as soon as possible after birth, then breastfeed at least 8 to 12 times every 24 hours to make plenty of milk for your baby. This means that in the first few days after birth, your baby will likely need to breastfeed about every hour or two in the daytime and a couple of times at night. Healthy babies develop their own feeding schedules. Follow your baby’s cues for when he or she is ready to eat.
Feedings may be 15 to 20 minutes or longer per breast. But there is no set time. Your baby will let you know when he or she is finished. If you are worried that your baby is not eating enough, talk to your baby’s doctor. Use our Feeding Chart (PDF, 110 KB) to write down when your baby wants to eat.
Breastfeeding holds
Some moms find that the following positions are helpful ways to get comfortable and support their babies in finding a good latch. You also can use pillows under your arms, elbows, neck, or back to give you added comfort and support. Keep in mind that what works well for one feeding may not work well for the next. Keep trying different positions until you are comfortable.
 |
Cradle hold – An easy, common hold that is comfortable for most mothers and babies. Hold your baby with his or her head on your forearm and his or her whole body facing yours. |
 |
Cross cradle or transitional hold – Useful for premature babies or babies with a weak suck because it gives extra head support and may help babies stay latched. Hold your baby along the opposite arm from the breast you are using. Support your baby’s head with the palm of your hand at the base of his or her neck. |
 |
Clutch or “football” hold – Useful for mothers who had a c-section and mothers with large breasts, flat or inverted nipples, or a strong letdown reflex. It is also helpful for babies who prefer to be more upright. This hold allows you to better see and control your baby’s head, and keep the baby away from a c-section incision. Hold your baby at your side, lying on his or her back, with his or her head at the level of your nipple. Support baby’s head with the palm of your hand at the base of the head. (The baby is placed almost under the arm.) |
 |
Side-lying position – Useful for mothers who had a c-section or to help any mother get extra rest while the baby breastfeeds. Lie on your side with your baby facing you. Pull your baby close so your baby faces your body. |
Tips for making it work
- Learn your baby’s hunger signs – When babies are hungry, they become more alert and active. They may put their hands or fists to their mouths, make sucking motions with their mouth, or turn their heads looking for the breast. If anything touches the baby’s cheek — such as a hand — the baby may turn towards this hand, ready to eat. This sign of hunger is called rooting. Offer your breast when your baby shows rooting signs. Crying can be a late sign of hunger and it may be harder to latch once the baby is upset. Over time, you will be able to learn your baby’s cues for when to start feeding.
- Follow your baby’s lead – Make sure you are both comfortable and follow your baby’s lead after he or she is latched on well. Some babies take both breasts at each feeding. Other babies only take one breast at a feeding. Help your baby finish the first breast, as long as he or she is still sucking and swallowing. This will ensure the baby gets the “hind” milk — the fattier milk at the end of a feeding. Your baby will let go of the breast when he or she is finished, and often falls asleep. Offer the other breast if he or she seems to want more.
- Keep your baby close to you – Remember that your baby is not used to this new world and needs to be held very close to his or her mother. Being skin-to-skin helps babies cry less and stabilizes the baby’s heart and breathing rates.
- Avoid nipple confusion – Avoid using pacifiers, bottles, and supplements of infant formula in the first few weeks unless there is a medical reason to do so. If supplementation is needed, try to give expressed breast milk first. But it’s best just to feed at the breast. This will help you make milk and keep your baby from getting confused while learning to breastfeed.
- Sleep safely and close by – Have your baby sleep in a crib or bassinet in your room, so that you can breastfeed more easily at night. Sharing a room with parents is linked to a lower risk of SIDS (sudden infant death syndrome).
- Know when to wake the baby – In the early
weeks after birth, you should wake your baby
to feed if 4 hours have passed since the beginning
of the last feeding. Some tips for waking
the baby include:
- Changing your baby’s diaper
- Placing your baby skin-to-skin
- Massaging your baby’s back, abdomen, and legs
Making plenty of milk
Your breasts will easily make and supply milk directly in response to your baby’s needs. The more often and effectively a baby breastfeeds, the more milk will be made. Babies are trying to double their weight in a few short months, and their tummies are small, so they need many feedings to grow and to be healthy.
Most mothers can make plenty of milk for their baby. If you think you have a low milk supply, talk to a lactation consultant. Visit the Finding support and information section for other types of health professionals who can help you.
| Time | Milk | The baby | You (Mom) |
|---|---|---|---|
| Birth | Your body makes colostrum (a rich, thick, yellowish milk) in small amounts. It gives your baby a healthy dose of early protection against diseases. | Will probably be awake in the first hour after birth. This is a good time to breastfeed your baby. | You will be tired and excited. |
| First 12-24 hours | Your baby will drink about 1 teaspoon of colostrum at each feeding. You may or may not see the colostrum, but it has what the baby needs and in the right amount. | It is normal for the baby to sleep heavily. Labor and delivery are hard work! Some babies like to nuzzle and may be too sleepy to latch well at first. Feedings may be short and disorganized. As your baby wakes up, take advantage of your baby’s strong instinct to suck and feed every 1-2 hours. Many babies like to eat or lick, pause, savor, doze, then eat again. | You will be tired, too. Be sure to rest. |
| Next 3-5 days | Your white milk comes in. It is normal for it to have a yellow or golden tint first. Talk to a doctor and lactation consultant if your milk is not yet in. | Your baby will feed a lot (this helps your breasts make plenty of milk), at least 8-12 times or more in 24 hours. Very young breastfed babies don’t eat on a schedule. Because breast milk is more easily digested than formula, breastfed babies eat more often than formula-fed babies. It is okay if your baby eats every 2-3 hours for several hours, then sleeps for 3-4 hours. Feedings may take about 15-20 minutes on each side. The baby’s sucking rhythm will be slow and long. You might hear gulping. | Your breasts may feel full and leak. (You can use disposable or cloth pads in your bra to help with leaking.) |
| The first 4-6 weeks | White breast milk continues. | Your baby will likely be better at breastfeeding and have a larger stomach to hold more milk. Feedings may take less time and will be farther apart. | Your body gets used to breastfeeding so your breasts will be softer and the leaking may slow down. |
How to know your baby is getting enough milk
Many babies, but not all, lose a small amount of weight in the first days after birth. Your baby’s doctor will check his or her weight at your first visit after you leave the hospital. Make sure to visit your baby’s doctor within three to five days after birth and then again at two to three weeks of age for check-ups.
You can tell if your baby is getting plenty of milk if he or she is mostly content and gaining weight steadily after the first week of age. From birth to three months, typical weight gain is two-thirds to one ounce each day.
Other signs that your baby is getting plenty of milk:
- He or she is passing enough clear or pale yellow urine, and it’s not deep yellow or orange (see the chart below).
- He or she has enough bowel movements (see the chart below).
- He or she switches between short sleeping periods and wakeful, alert periods.
- He or she is satisfied and content after feedings.
- Your breasts feel softer after you feed your baby.
Talk to your baby’s doctor if you are worried that your baby is not eating enough.
A newborn’s tummy is very small, especially in the early days. Once breastfeeding is established, exclusively breastfed babies from 1 to 6 months of age take in between 19 and 30 ounces per day. If you breastfeed 8 times per day, the baby would eat around 3 ounces per feeding. Older babies will take less breastmilk as other food is introduced. Every baby is different, though.
 |
 |
| Hazelnut | Walnut |
At birth, the baby’s stomach can comfortably digest what would fit in a hazelnut (about 1-2 teaspoons). In the first week, the baby’s stomach grows to hold about 2 ounces or what would fit in a walnut.
| Baby's age | Number of wet diapers | Number of bowel movements | Color and texture of bowel movements |
|---|---|---|---|
| Day 1 (first 24 hours after birth) | 1 | The first one usually occurs within 8 hours after birth | Thick, tarry, and black |
| Day 2 | 2 | 3 | Thick, tarry, and black |
| Day 3 | 5-6 | 3 | Looser greenish to yellow (color may vary) |
| Day 4 | 6 | 3 | Yellow, soft, and watery |
| Day 5 | 6 | 3 | Loose and seedy, yellow color |
| Day 6 | 6 | 3 | Loose and seedy, yellow color |
| Day 7 | 6 | 3 | Larger amounts of loose and seedy, yellow color |
How long should I breastfeed?
Many leading health organizations recommend that most infants breastfeed for at least 12 months, with exclusive breastfeeding for the first six months. This means that babies are not given any foods or liquids other than breast milk for the first six months. These recommendations are supported by organizations including the American Academy of Pediatrics, American Academy of Family Physicians, American Congress of Obstetricians and Gynecologists, American College of Nurse-Midwives, American Dietetic Association, and American Public Health Association.
More information on learning to breastfeed
Read more from womenshealth.gov
-
Your Guide to Breastfeeding — This easy-to-read publication provides women the how-to information and support needed to breastfeed successfully. It explains why breastfeeding is best for baby, mom, and society and how loved ones can support a mother's decision to breastfeed. Expert tips and illustrations help new moms learn how to breastfeed comfortably and how to overcome common challenges.
http://www.womenshealth.gov/publications/our-publications/breastfeeding-guide/
Explore other publications and websites
-
Breastfeeding 101 (Copyright © American College of Nurse-Midwives) — This publication outlines the basic steps moms need to take when preparing to breastfeed, issues they may face regarding siblings of the new baby, and how to develop family support.
http://www.mymidwife.org/Breastfeeding-101
-
Breastfeeding vs. Formula Feeding (Copyright © Nemours Foundation) — This publication discusses the benefits of breastfeeding and the pros and cons of bottle-feeding, as well as answering common breastfeeding questions.
http://www.kidshealth.org/parent/food/infants/breast_bottle_feeding.html
-
Breastfeeding Your Baby (Copyright © American College of Obstetricians and Gynecologists) — This online resource about breastfeeding provides information on getting started with breastfeeding, diet, sex and birth control, work, and breast health. It also includes a glossary of terms.
http://www.acog.org/publications/patient_education/bp029.cfm
-
Breastfeeding: Hints to Help You Get Off to a Good Start (Copyright © American Academy of Family Physicians) — This fact sheet offers helpful hints on successful breastfeeding, including how to hold your baby, what you need to know about the let-down reflex, how to prevent and heal sore nipples, what to avoid eating, and where to get more information on breastfeeding.
http://familydoctor.org/online/famdocen/home/women/pregnancy/birth/019.html
-
FAQ on Breastfeeding Twins (Copyright © La Leche League International) — This publication provides information on breastfeeding twins. It includes positioning techniques, feeding plans, and ways to care for oneself.
http://www.llli.org/FAQ/twins.html
-
Got Mom (Copyright © American College of Nurse Midwives) — GotMom.org was created by the American College of Nurse-Midwives to provide breastfeeding information and resources for mothers and families. It has information on why breast milk is best, dispels common misunderstandings about breastfeeding, and provides a list of resources that can help women and families with breastfeeding.
http://www.gotmom.org/
-
How Can I Increase My Milk Supply? (Copyright © La Leche League International) — This publication explains how to know if you're not producing enough breast milk for your baby and gives tips on increasing your milk supply.
http://www.llli.org/FAQ/increase.html
-
How Can I Tell if My Baby is Getting Enough Milk? (Copyright © La Leche League International) — This publication explains how to look for signs that your baby is getting enough breast milk. It also provides additional resources on milk supply and breastfeeding for more information.
http://www.llli.org/FAQ/enough.html
-
How Do I Wean My Baby? (Copyright © La Leche League International) — This publication explains why it is important to wean your baby slowly off of the breast. It also gives tips for when and how to reduce feedings to make the weaning process easier.
http://www.lalecheleague.org/FAQ/weanhowto.html
-
How Often Should I Nurse My Baby? (Copyright © La Leche League International) — This publication gives guidelines for how often babies should breastfeed. It also explains why a baby may feed frequently or infrequently and what behaviors are considered normal during the period of breastfeeding.
http://www.llli.org/FAQ/frequency.html
-
Increasing Breastfeeding Success: Why it Matters and What the Research Shows (Copyright © Breastfeeding Coalition of Washington) — This publication is a set of ten lactation presentations designed to educate physicians and their staff in the in-patient or out-patient setting.
http://www.breastfeedingwa.org/node/116
-
Weaning Your Child (Copyright © The Nemours Foundation) — This publication discusses when to wean and also gives tips on how to start weaning to make the transition easier.
http://www.kidshealth.org/parent/pregnancy_newborn/feeding/weaning.html
Connect with other organizations
-
American Academy of Family Physicians
http://familydoctor.org/online/famdocen/home.html
-
American Academy of Pediatrics
http://www.aap.org/
-
American College of Nurse-Midwives
http://www.midwife.org/index.cfm
-
International Lactation Consultant Association (ILCA)
http://www.ilca.org
-
KellyMom
http://kellymom.com/
-
La Leche League International
http://www.llli.org/
-
Maternal and Child Health Bureau, HRSA, HHS
http://www.mchb.hrsa.gov/
-
National Center for Education in Maternal and Child Health
http://www.ncemch.org/
-
National Healthy Mothers, Healthy Babies Coalition
http://www.hmhb.org/
-
Wellstart International
http://www.wellstart.org/
-
Womenshealth.gov, OWH, HHS
http://www.womenshealth.gov/
-
World Alliance For Breastfeeding Action
http://www.waba.org.my/
Content last updated August 1, 2010.
Resources last updated August 1, 2010.
womenshealth.gov
A federal government website managed by the Office on Women's Health in the Office of the Assistant Secretary for Health at the U.S. Department of Health and Human Services.
200 Independence Avenue, S.W. • Washington, DC 20201


 Text size
Text size Email
Email