State of CDC Archive
Reform Health Policies
2009
Achieving better health for all requires more than a public health approach. It requires prevention of chronic conditions through more effective health care policies. Community prevention programs, public health infrastructure support, and prevention research are part of this work. Having public health play a role in health reform is critical to address health care cost containment and improve access and quality of services. As the focus moves to primary prevention, state and local health departments will have an increased role in ensuring the health of communities across the country.
We know that we need health reform to ensure Americans get the high-quality, affordable care they need and deserve. Under the status quo, too many Americans can’t get the affordable care they need when they fall ill. Health reform must make health care more than just sick care, it must also improve the health of our nation by investing in critical prevention and wellness initiatives that help keep Americans healthy and out of the hospital in the first place.
Today, we spend more on health care than any other country in the world, yet we don’t live longer. Scientists say this generation of children may not live as long as their parents did. If we do nothing, many of them will grow up to develop a chronic disease that could have been prevented if we encouraged wellness rather than just focus on treatment.
The American people remember the old adage and they know that an ounce of prevention truly is worth a pound of cure. That is just one of the reasons why helping to prevent disease and illness also has strong public support. Preventing illness and disease is an essential component of health reform. We know that it isn’t enough to provide coverage and keep doing the same thing. Health reform can help stop diseases before they happen. It can make our homes, our communities and our families healthier, safer and stronger. It’s time to make preventing illness and disease the foundation of our health care system.
We face many challenges and have many opportunities, especially with the President’s signature issue of health reform. Improving our health care system to increase access, affordability, and quality will require creative and strategic thinking. President Obama is committed to prevention as a key component of reform, as evidenced by the Recovery Act, and has highlighted the need for our society to do more to prevent, manage, and treat chronic diseases.
2008
Pandemic Influenza: New Test, New Vaccines
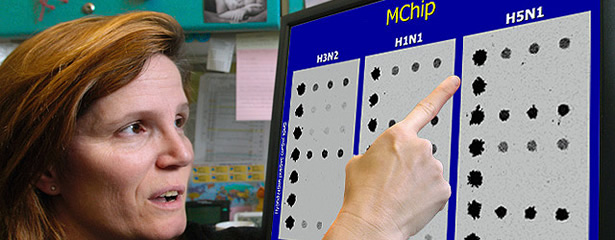
On September 30, 2008, the US Food and Drug Administration cleared an important new test that can rapidly detect and identify human influenza viruses, including those that may pose a pandemic risk. The human influenza virus real-time polymerase chain reaction detection and characterization panel (RT-PCR) was developed by CDC in collaboration with Applied Biosystems of Foster City, California and the Association of Public Health Laboratories. Using a molecular biology technique, the RT-PCR can test multiple samples at once and renders results within just four hours.
CDC developed six H5N1 pandemic influenza vaccine candidates derived from viruses from Indonesia and China for use in manufacturing prepandemic vaccines including H5N1 vaccine candidate Clade 2.1 and H5N1 vaccine candidate Clade 2.2. H5N1 viruses are the avian influenza viruses currently causing human cases in Asia and Africa (more than 300 cases so far). They are a concern because of the potential to become a new pandemic strain. They have caused outbreaks in birds (usually chickens) in Asia, Africa, the Middle East, and Europe.
CDC also developed a five-target polymerase chain reaction panel for influenza (A, B, H1, H3, and H5); approval is pending from the US Food and Drug Administration. This new area of diagnostics for CDC will greatly enhance disease detection, prepare people for emerging health threats, and provide a path for future development.
First Pandemic Influenza Ethics Workshop Held in Africa
CDC collaborated with the African Field Epidemiology Network to convene a symposium on public health codes of ethics for pandemic influenza detection and control in Africa. Representatives from 15 African countries discussed how to make ethical decisions using current scientific knowledge while evaluating the effectiveness of interventions.
Conference participants identified and discussed African-specific ethical challenges likely to arise during a pandemic:
- Enforcement of culling sick poultry when poultry is the primary protein in African diets.
- Compensation for owners who are required to cull their smaller flocks.
- Politicians who try to reserve available vaccines for their own use.
- Opposition to preparing for a pandemic when most people die from AIDS, malaria, and tuberculosis.
Hearing Initiative Triples Screening for Infants
Strong partnerships and collaborations with other federal agencies, states and territories, as well as several professional organizations are responsible for the remarkable success of CDC’s Early Hearing Detection and Intervention program. At the program’s inception, fewer than 30% of infants in the United States were being screened for hearing loss, compared to more than 92% today.
This program is a national initiative that supports the early identification of infant hearing loss through screening, audiological diagnosis, medical evaluation, and enrollment in early intervention services. More than 12,000 babies are born in the United States with hearing loss every year. Prior to this program, the average age of diagnosis of hearing loss in infants and young children ranged from 14 months to around three years of age. Now, many infants are diagnosed before three months of age. With screening and early intervention, estimates show a reduction of $44,220 per child in lifetime educational costs for children with permanent bilateral hearing loss—a potential savings of approximately $200 million annually.
Increasing Vaccine Access to Children Worldwide

In low-income countries around the world, CDC has made significant contributions in introducing and administering Haemophilus influenzae type b (Hib) vaccine. The vaccine protects susceptible populations from Hib disease, one of the leading causes of severe childhood pneumonia and meningitis.
Hib disease is the estimated cause of three million cases of meningitis and severe pneumonia and is responsible for approximately 400,000 deaths worldwide per year in children five years of age and younger. Safe and effective Hib vaccines have been widely used in industrialized countries for nearly 20 years, but they have been relatively unavailable in the world’s poorest countries.
In 2000, the Global Alliance for Vaccines and Immunization (GAVI) initiated a project that provided financial support for purchasing and providing the Hib vaccine in 72 of the world’s poorest countries. From 2004–2008, the proportion of these countries using or approved to use Hib vaccine increased from 17% to 56% thanks to a focused, collaborative effort by the GAVI, the World Health Organization, and CDC. This number is projected to increase to 81% in 2009, supporting and sustaining CDC’s efforts to promote Healthy People in Every Stage of Life.
In 2004, 6.8 million children born in one of the 72 GAVI-eligible countries had access to the Hib vaccine. In 2007, 14 million of the 79 million children had vaccine access, and by the end of 2008, 43 million children are expected to have access. Several factors fostered increased interest and use of the Hib vaccine in the GAVI-eligible countries:
- Greater awareness of the amount and severity of disease caused by Hib.
- Greater encouragement by the World Health Organization that the Hib vaccine be included in routine immunization programs in all countries.
- Greater effort by GAVI to make the vaccine more affordable and accessible to the world’s most susceptible populations.
Reductions in Healthcare-associated Infections

CDC and its public health partners have significantly influenced hospital infection control practices nationwide. Bloodstream infections associated with a central line (a type of venous catheter) are among the most common type of healthcare-associated infections (HAIs), with an estimated 250,000 cases reported in US hospitals each year. However, in several states around the country, these HAIs have been reduced by as much as 66%–70%. Seeing a national reduction of two-thirds of bloodstream infections could translate into as many as 180,000 fewer HAIs and $4–$6 billion in health care cost savings.
In recent years, CDC and its partners have worked to ensure that more health care facilities have been following CDC’s guidelines and recommendations in support of CDC’s Health Protection Goal of Healthy People in Healthy Places:
- Among hospitals participating in the CDC’s National Healthcare Safety Network, the rate of central line-associated bloodstream infections decreased by 40%–50% among patients in intensive care units (ICUs) during the last decade. Rates also decreased by 50% in most major ICUs for the subset of central line-associated bloodstream infections associated with methicillin-resistant Staphylococcus aureus.
- CDC collaborated with the Pittsburgh Regional Health Initiative to target a common type of HAI—catheter-associated bloodstream infections—that occur in ICUs. The Catheter-Associated Bloodstream Infections Prevention Strategy included educational models and standardized tools for hospital staff and comparison data for participating hospitals. The intervention was implemented in 32 hospitals and 66 ICUs in southwestern Pennsylvania. After four years, the 32 participating hospitals were able to collectively reduce their blood stream infection rates among patients in their ICUs by 68%. This intervention has been replicated elsewhere with similar reductions in HAIs.
- In Michigan, the Agency for Healthcare Research and Quality funded the Keystone Initiative that resulted in a 70% decline of central-line associated bloodstream infections when CDC guidelines were fully implemented. The dramatic reductions in serious ICU infections prompted replication of these efforts in hospitals across the country.
- Several states using the National Healthcare Safety Network for mandated reporting of healthcare-associated infections have identified prevention of bloodstream infections as a priority. For example, by adopting safety and prevention practices, infection rates in New York have declined more than 70% in ICUs participating in the Greater New York Hospital Association Prevention Collaborative.
CDC plans to build on these successes in reducing bloodstream infections by developing and implementing similar strategies for reducing other healthcare-associated infections.
One Millionth Call to 1-800-QUIT-NOW

Tobacco use is the leading cause of preventable death and disease in the United States. So when one million calls were placed to 1-800-QUIT-NOW there was reason to celebrate. The national, toll-free number for free help to quit tobacco use was developed by the National Network of Tobacco Cessation Quitlines, a dynamic collaboration among states, CDC, the National Cancer Institute, and the North American Quitline Consortium.
An estimated 43 million American adults currently smoke cigarettes, and cigarette smoking and exposure to secondhand smoke causes approximately 443,000 deaths annually. For every person who dies from tobacco use, another 20 suffer with at least one serious tobacco-related illness. This addiction costs the nation more than $96 billion per year in direct medical expenses as well as more than $97 billion in lost productivity annually.
CDC’s Best Practices for Comprehensive Tobacco Control Programs, 2007 describes an integrated programmatic structure for implementing interventions that are proven to be effective. The report also provides guidance to states regarding the recommended levels of investment in tobacco control to reduce the burden of tobacco use on the nation. Comprehensive tobacco control programs have been shown to reduce smoking rates, tobacco-related deaths, and disease when they are sustained and accountable. By collaborating with our many partners, CDC is expanding its vision of promoting Healthy People in a Healthy World.
For more information on comprehensive tobacco control programs visit
Best Practices for Comprehensive Tobacco Control Programs ![]() (95 pages).
(95 pages).
Birth Defects Prevention Study
In 2008, CDC’s National Birth Defects Prevention Study provided further evidence that smoking and diabetes in women are harmful to unborn babies by contributing to major, structural birth defects.
Women who have diabetes before they become pregnant are three to four times more likely to have a child with one or even multiple birth defects than a mother who is not diabetic. Also, women who smoke early in their pregnancy are more likely to give birth to infants with congenital heart defects and orofacial clefts. These findings have significant public health implications because nearly three percent of all infants born in the United States have a major birth defect, and nearly one percent have a congenital heart defect.
CDC’s National Birth Defects Prevention Study is the largest population-based study on the causes of birth defects ever undertaken in the United States.
2007
President’s Malaria Initiative
The global toll of malaria is high: an estimated one million people die each year, most of them young children in Africa. The economic costs alone for malaria-related illness and mortality are estimated to cost Africa’s economy $12 billion per year. Since President Bush announced the $1.2-billion President’s Malaria Initiative (PMI) in 2005, CDC has been at the forefront of efforts to cut malaria deaths in half in targeted African countries. CDC worked closely with USAID not only to design the initiative, but to conceive and implement evaluation of PMI’s impact in achieving its goal. To date, PMI has provided life-saving interventions to more than six million people, and estimate that approximately 11 million people were reached with life-saving interventions by the end of 2007. An additional eight countries also will be added to initiative in FY2008.
Health Protection Goals Transform CDC
Over the last year, CDC centers, institute, and offices worked collaboratively and with CDC’s partners to develop the full vision of CDC’s four Health Protection Goals to promote and protect health in every stage of life, in every place, for emerging health threats, and around the world.
CDC’s goals guide our work and have resulted in many new proposals that incorporate collaborative and holistic approaches to addressing health protection.
An example of the projects coming specifically from the goal objectives and coordinated across CDC centers is a one-year Healthy Parenting Fellowship supported by the Healthy Children Goal. This fellowship will bring a visiting scientist to CDC to help increase the agency’s knowledge base on the role healthy parenting plays in improving health from birth through adolescence and will focus on the middle childhood population (ages 4–11 years). This enhanced knowledge will, in turn, enable CDC to develop more effective parent-targeted programs and initiatives.
The development of other goals and objectives are resulting in similar cross-cutting recommendations to unite CDC internally and externally with its partners to improve health impact. A Green Healthcare proposal backed by the Healthy Healthcare Goal proposes the investigation of how a hospital’s design, function, and indoor environment affect patient recovery and outcomes and healthcare worker safety, health, and productivity. The project involves wide collaboration that brings together multiple centers and offices at CDC as well as other government partners, including the Environmental Protection Agency and the Agency for Healthcare Research and Quality, as well as private partner, Kaiser Permanente.
Developing the home-focused messages draws from the current work in CDC programs, such as lead poisoning; injury; indoor air, including secondhand smoke; food safety; nutrition and physical activity; emergency preparedness; pest control; and infectious disease. This project also coordinates with other federal agencies and professional and nongovernmental organizations.
CDC’s four overarching health protection goals and the goal plans continue to transform the way CDC does the business of health protection by ensuring that our work is even more targeted and result/outcome oriented; our approach, action, and method are strategic and evidence based; that our course of action is specific and advances underlying strategies; and that we can measure our progress and promote accountability for the work we do.
Leading Health Homeward Bound

Environmental Health Initiatives Focus Inside—and Outside—the Home
is synonymous with security and comfort, yet also dwelling within millions of houses is a host of potential health hazards. Childhood lead poisoning, injuries, and respiratory diseases such as asthma have been linked to the more than 6 million substandard housing units nationwide. Residents of these units are also at increased risk for fire, electrical injuries, falls, rodent bites, and other illnesses and injuries.
With most Americans spending an average of 90% of their time indoors, taking a good look inside makes good public health sense. CDC’s Healthy Homes Initiative is a coordinated, comprehensive, and holistic approach to preventing diseases and injuries that result from housing-related hazards. The initiative’s goal is to identify health, safety, and quality-of-life issues in the home environment and to systematically eliminate or mitigate problems.
New products from the initiative include the Healthy Housing Reference Manual, written by staff from CDC and the Department of Housing and Urban Development. The manual helps public health and housing professionals ensure that housing stock is safe, decent, affordable, and healthy for our citizens, particularly children and the elderly, who are often most vulnerable and spend more time in the home. The initiative also includes the development of the Healthy Homes Clearinghouse, which will include six regional academic centers. (See www.healthyhouses.org.)
The environment outside our homes also has a large influence on our health. The air we breathe. The water we drink. The roads we share. From home to workplace to community, CDC is looking at an increasing range of ways in which the built environment impacts health. Recent contributions include a national satellite broadcast at the University of North Carolina looking at “place-specific” health issues and grants funding research on obesity and the built environment. Studies of mixed use neighborhoods that have homes, businesses, schools in one location will assess physical activity and travel behaviors before and after individuals move in.
CDC continues to provide leadership in its own community through sustainable building, water conservation, and workplace wellness. In 2006, HHS selected CDC’s Arlen Specter Headquarters and Emergency Operations Center on the Roybal campus and Building 110 on the Chamblee campus to be featured in its Energy Leadership poster as a model for other federal agencies to adopt similar building practices.
Recognizing that drought is a worldwide issue with major health consequences, CDC also exerts leadership in water conservation. During Georgia’s current drought, CDC facilities benefited from having been engineered to collect and recycle water through green designs – steps that lead to significantly reduced water consumption.
At the same time, CDC’s Healthier Worksite Initiative is developing projects and implementing plans for green activities and health promotion activities, including recycling, campus garden markets, employee van pools, new E-health tools, and green teams to address various environmental issues.
Contact Us:
- Centers for Disease Control and Prevention
1600 Clifton Rd
Atlanta, GA 30333 - 800-CDC-INFO
(800-232-4636)
TTY: (888) 232-6348 - cdcinfo@cdc.gov