Survey of Endoscopic Capacity (SECAP) II
The First SECAP Study (SECAP I)
In 2000, CDC's National Health Interview Survey (NHIS) and Behavioral Risk Factor Surveillance System (BRFSS) showed that only about half of adults aged 50 years or older had been screened for colorectal cancer as recommended. During this time, many national and state programs were being developed to increase colorectal cancer screening rates, and CDC conducted a study to find out if enough screening tests, facilities, and doctors were available for more people to be screened and get follow-up tests for positive results.
CDC conducted the study at the national level and in selected states (Colorado, Georgia, Iowa, Maine, Maryland, Massachusetts, Minnesota, Michigan, New Mexico, New York, North Carolina, South Carolina, Ohio, Texas, and Washington). National results showed that it would take five to 10 years to develop the resources to screen everyone as recommended using only colonoscopy or flexible sigmoidoscopy.colonoscopy or flexible sigmoidoscopy. However, several states had enough resources to screen with these two tests within three years.1 2
National results also showed there was capacity to screen everyone in need of colorectal cancer screening within one year using fecal occult blood tests (FOBTs) followed by colonoscopy for those who tested positive.1 2
Results from this study helped guide planning for national and state colorectal cancer screening programs, including CDC's Colorectal Cancer Screening Demonstration Program, administered from 2005–2009, and the Colorectal Cancer Control Program, which supports colorectal cancer screening efforts in 25 states and four tribes across the United States.
The Follow-Up Study (SECAP II)
Since the first SECAP study ended—
- More people have become aware of the importance of colorectal cancer screening.3
- More people are being screened as recommended.3 4 5 6 7 8
- Colonoscopy is used for screening more often.3 4 5 8 9
- More people are expected to be able to afford screening due to the Affordable Care Act.3 4
CDC is conducting a follow-up study (SECAP II) to determine the colorectal cancer screening capacity in the nation and in newly selected states (Alabama, Alaska, Arkansas, Florida, Hawaii, Kentucky, Nebraska, Nevada, New Jersey, North Dakota, Pennsylvania, Utah, and West Virginia), one tribal organization (Alaska Native Tribal Health Consortium), and one territory (Guam). Like the first study, the second study has three parts: a survey, forecasting model, and capacity assessment.
Survey
A survey [PDF-366KB] will be sent to medical offices that perform colonoscopy and sigmoidoscopy to estimate the number of these tests that can be used for screening or follow-up in a 46-week period.
Forecasting Model
A forecasting model uses public data to estimate the number of people at average risk for colorectal cancer who need to be screened, and the number of tests needed to screen them.
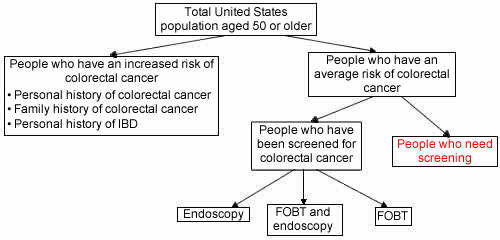
The number of people who are at average risk for colorectal cancer is determined by subtracting the number of people who are at high risk for colorectal cancer from the United States population aged 50 years old or older.
The number of people who have not been screened for colorectal cancer is determined by subtracting the number of people who have already been screened for colorectal cancer from the number of people who are at average risk for colorectal cancer. See the graphic below.
We will use five possible screening scenarios when determining the number of tests needed to screen everyone who has not been screened. The first scenario assumes screening tests are used in the same proportions as they are now. The other four scenarios assume screening options recommended by national guidelines. These scenarios assume that people who have not been screened for colorectal cancer will be screened with—
- A yearly FOBT with follow-up colonoscopy for positive tests, or
- An FOBT plus sigmoidoscopy, or
- Sigmoidoscopy with follow-up colonoscopy for positive tests, or
- Colonoscopy.
More details on the methods used for the forecasting model are available in the article, "Is there endoscopic capacity to provide colorectal cancer screening to the unscreened population of the United States?"
Capacity Assessment
Capacity assessments are determined by comparing the number of tests needed in each of the five screening scenarios to the number of screening tests available.
Differences Between the National and State, Tribal, and Territorial Studies
The national and state, tribal, and territorial studies are nearly the same, but have small differences in the survey and forecasting model methods.
- Survey recipients. The national SECAP II survey will be given to a random group of facilities in the United States that perform colorectal cancer screening tests. The state, tribal, and territorial SECAP II surveys will be given to all facilities in the state, tribe, or territory sample that perform these tests.
- Data source for forecasting model. Data from the 2010 NHIS will be used for the national forecasting model. Data from the 2008 and 2010 BRFSS will be used for the state, tribal, and territorial forecasting models.
National and state, tribe, and territory data is being collected now.
References
1Seeff LC, Manninen DL, Dong FB, Chattopadhyay SK, Nadel MR, Tangka FKL, Molinari N-AM. Is there endoscopic capacity to provide colorectal cancer screening to the unscreened population of the United States? Gastroenterology 2004;127(6):1661–1669.
2Seeff LC, Richards TB, Shapiro JA, Nadel MR, Manninen DL, Given LS. How many endoscopies are performed for colorectal cancer screening? Results for the CDC's survey of endoscopic capacity. Gastroenterology 2004;127(6):1670–1677.
3Shapiro JA, Seeff LC, Thompson TD, Nadel MR, Klabunde CN, Vernon SW. Colorectal cancer test use from the 2005 National Health Interview Survey. Cancer Epidemioliogy, Biomarkers and Prevention 2008;17(7):1623–1630.
4CDC. Vital signs: colorectal cancer screening, incidence, and mortality—United States, 2002–2010. MMWR 2011;60(26):884–889.
5CDC. Vital signs: colorectal cancer screening among adults aged 50–75 years—United States, 2008. MMWR 2010;59(26):808–812.
6CDC. Colorectal cancer screening—United States, 2002, 2004, 2006, and 2008. MMWR 2011;60(1):42–46.
7CDC. Surveillance of screening-detected cancers (colon and rectum, breast, and cervix)—United States, 2004–2006. MMWR 2010;59(SS9):1–25.
8CDC. Use of colorectal cancer tests—United States, 2002, 2004, and 2006. MMWR 2008;57(10):253–258.
9Stock C, Knudsen AB, Lansdorp-Vogelaar I, Haug U, Brenner H. Colorectal cancer mortality prevented by use and attributable to nonuse of colonoscopy. Gastrointestinal Endoscopy 2011;73(3):435–443.e5.
Contact Us:
- Centers for Disease Control and Prevention
Division of Cancer Prevention and Control
4770 Buford Hwy NE
MS K-64
Atlanta, GA 30341 - 800-CDC-INFO
(800-232-4636)
TTY: (888) 232-6348
8am–8pm ET
Monday–Friday
Closed on Holidays - cdcinfo@cdc.gov


