Managing Elevated Blood Lead Levels Among Young Children: Recommendations from the Advisory Committee on Childhood Lead Poisoning Prevention
Chapter 2 - Assessment and Remediation of Residential Lead Exposure
- Table 2.1. Summary of Recommendations for Assessment and Remediation of Residential Lead Exposure
- Introduction
- Sources and pathways of residential lead exposure
- Effectiveness and Safety of Lead Hazard Control Measures
- Recommendations for Assessment and Remediation
- Enforcement of Laws and Regulations
- Financial Resources for Lead Hazard Control
- Recommendations for Future Research
- References
- Diagrams of Lead Exposure in the Residential Environment
- Fig 2.1
- Fig 2.2
- Fig 2.3 - Table 2.2. Time Frames for Environmental Investigation and Other Case Management Activities According to a Child’s Blood Lead Levela
- Table 2.3. Common Sources of Lead Exposure to Consider in an Environmental Investigation
Table 2.1. Summary of Recommendations for Assessment and Remediation of Residential Lead Exposure
|
Make
prompt and effective environmental management for children with
EBLLs the highest priority of all childhood lead poisoning
prevention programs. 1. Conduct an environmental investigation for all children with blood lead levels >=20 µg/dL, or persistently $15 µg/dL. This investigation should include: |
||
| a. | An inspection of the child’s home and other sites where the child spends significant amounts of time. | |
| b. | A history of the child’s exposure | |
| c. | Measurements of environmental lead levels, including at a minimum | |
| i. | House dust; | |
| ii. | Paint that is not intact or is subject to friction; | |
| iii. | Exposed soil, especially in play areas; | |
| iv. | Other media as appropriate; | |
|
2. Ensure that interventions to reduce ongoing exposure: |
||
| a. | Focus on control of current lead hazards. | |
| b. | Include prompt interim measures (e.g., house dust control by professional cleaners) where appropriate, to rapidly reduce lead exposure. | |
| c. | Be performed in accordance with safe practices by trained workers to avoid increasing lead exposure to occupants and workers. | |
| d. | Keep to a minimum on-site removal of intact leaded paint. | |
| e. | Replace or enclose building components when elimination of intact leaded paint is performed. | |
| f. | Include
clearance testing following lead hazard reduction work to ensure that lead levels are safe prior to a structure being re-occupied. |
|
| g. | Include temporary occupant relocation or other measures to protect occupants from exposure to leaded dust produced by lead hazard control activities. | |
| h. | Relocate children permanently to lead-safe housing if necessary to reduce their lead exposure in a timely manner. | |
|
3. Encourage state and local governments to assess the effectiveness of their laws, ordinances, housing codes, and enforcement structures in dealing with identified lead hazards and to identify changes required to ensure that children are protected. |
||
| 4. Promote the expansion of existing federal, state, and local subsidies to help finance lead hazard control in economically distressed communities, and the creation of new subsidies, if necessary. | ||
Introduction
Recent research concerning lead exposure from leaded paint in the residential environment has shown that some of the recommendations on managing lead hazards in the child’s environment made in the 1991 Centers for Disease Control and Prevention (CDC) guidance, Preventing Lead Poisoning in Young Children, need updating (1). In addition, a regulation to control lead exposure from public drinking water (2), implemented during the 1990s, makes possible a more focused approach to assessing that source than was previously recommended. This chapter summarizes current knowledge concerning children’s lead exposure in the residential environment, recommends interventions directed at reducing or eliminating lead exposure, and provides information to guide state and local officials in developing and updating policies and procedures for identifying and managing lead hazards in the residential environment of children with elevated blood lead levels (EBLLs).
Detailed technical protocols for assessing and correcting lead hazards in a variety of situations can be found in guidance developed by the Department of Housing and Urban Development (HUD) for property owners, private contractors, and government housing agencies (3). These are cited where appropriate.
Sources and pathways of residential lead exposure
Lead can be found in high concentrations in three media to which children may be directly or indirectly exposed: paint, interior dust, and exterior soil or dust. This section discusses the distribution of lead in these media and their relationships to one another and to blood lead levels (BLLs) in children (Figure 2.1). Lead in tap water, generally a lower dose source of exposure, is also addressed.
Paint
Although the addition of lead to residential paint and similar surface-coating materials, such as varnishes and stains, was banned in 1978 (4), 74% of dwellings constructed prior to 1980 contain some leaded paint.* The amount of lead in paint is much greater in homes built before 1950 than in homes built later but prior to the ban on leaded house paint. For example, 90% of dwellings built before 1940 have paint
---------------------------------------
*Throughout this document, the term "paint" will be used to refer to paint and,
where appropriate, similar surface-coating materials such as varnishes and
stains. Paints and coatings manufactured since 1978 must contain < 0.06%
lead by weight. For testing of lead content in existing structures, the
regulatory threshold for defining "lead-based paint" is
$
1 milligram of lead per square centimeter of paint film or
$
0.5 % lead by weight. These standards, however, were based on the limitations of
measurement techniques available when they were formulated rather than on
health considerations.
----------------------------------------
containing more than 1 mg/cm2 of lead, compared with 62% of dwellings built from 1960 through 1979. The relative contrast is much greater for paint containing more than 2 mg/cm2: 75% versus 18%, respectively (5). Direct and indirect exposure of children to leaded paint that has deteriorated because of deferred maintenance is likely the major factor in the increased risk for EBLL associated with poverty and living in older housing. Data from the Third National Health and Nutrition Examination Survey (NHANES III) indicate that the prevalence of EBLLs among children living in homes built before 1946 is five times higher than that among children living in homes built after 1973 (most of which do not have leaded paint) (6). Furthermore, for low-income children living in pre-1946 dwellings, the prevalence of EBLLs is 16%, compared with 4% for middle-income children living in such dwellings (6).
Although children may be exposed to lead from paint directly by ingesting paint chips (7), they are more commonly exposed by ingesting house dust or soil contaminated by leaded paint (8, 9). Federal law defines a leaded paint hazard as a condition in which exposure to lead from lead-contaminated dust, lead-contaminated soil, or deteriorated leaded paint would have an adverse effect on human health (10).
Lead contamination of dust or soil occurs when leaded paint deteriorates or is subject to friction or abrasion (as on window sashes). In addition, lead can be dispersed when paint is disturbed during demolition, remodeling, paint removal, or preparation of painted surfaces for repainting. In a population-based study in Wisconsin, about two-thirds of children who had a blood lead test lived in a home that had undergone some type of renovation, repair, or remodeling work in the prior year. These children were at 1.3 times greater risk of having an EBLL than were children not exposed to such activities (11). The risk was even higher among children living in homes where certain practices, such as the removal of paint with heat guns, had been used.
Interior dust
Interior house dust can become contaminated with lead as the result of the deterioration or disturbance of leaded paint, the tracking or blowing in of contaminated soil, and the fallout of airborne lead particulate from industrial or vehicular sources. A simple visual inspection of older homes can identify those in poor condition. The condition of leaded paint more accurately predicts lead exposure than the lead content of paint by itself (12, 13). Older homes in poor condition have much higher dust lead levels than older homes in good condition (Figure 2.2) (14). The amount of lead in house dust, in turn, has a strong correlation with the BLLs of young children (12, 13, 15, 16) and is more predictive of BLLs in children than is the amount of lead in house paint (13). Lead levels in house dust can be measured either as a mass concentration (mass of lead/mass of dust) or as surface loading (mass of lead per surface area sampled). The most widely used sampling technique, in which a wipe sample is collected with commercially available baby wipes (3), can determine only lead surface loading. However, this measure predicts BLLs as well as or better than mass concentration (17). Lead loadings vary considerably among the types of surfaces commonly tested, with levels on interior window sills and window "wells" (the part of the window that receives the lower sash when closed) often being, respectively, 1 and 2 orders of magnitude higher than those found on floors. Higher levels on window components may reflect a combination of lead dust derived from friction and the deterioration of leaded paint on the windows themselves and from the settling of airborne dust from outside of the dwelling. Dust lead loading on all three surfaces (floors, windowsills, and window wells) correlates with BLLs in children (12).
A recent statistical analysis of data from 12 studies relating lead in dust to BLLs in children between 6 and 36 months of age found a strong direct association between dust lead loading and the risk of having an EBLL (13). The association extended well below the 40 µg/ft2 threshold for a lead hazard in dust samples collected from floors as defined by HUD (18) and the Environmental Protection Agency (EPA) (19). For example, the estimated probability of a child having an EBLL increases from 7% to 18% with an increase in floor dust lead loading from 10 to 40 µg/ft2 (Figure 2.3) (13). For dust samples collected from window sills, lead levels >=250 µg/ft2 are defined as hazardous (18, 19).
Soil and Exterior Dust
Contamination of soil and exterior dust has been linked to point source emissions, such as lead smelters, fall-out from past use of leaded gasoline, and weathering of exterior leaded paint (20). Soil located next to dwellings typically has higher lead content than that sampled from other locations in a yard.
Potentially hazardous levels of lead in soil are not uncommon. Results of a national survey in which soil samples were collected from both bare and covered soil showed that residences with intact exterior leaded paint are more than three times as likely to have soil lead levels exceeding 500 ppm than are dwellings without lead in exterior paint (21% vs. 6%). Results also showed that soil contamination is eight times more common at residences with non-intact leaded exterior paint than at residences without exterior leaded paint (48% vs. 6%) (5). In urban neighborhoods, high levels of lead have also been found in exterior dust collected from paved surfaces, such as sidewalks (21).
Soil lead content is an important predictor of children’s risk for an EBLL, though less important than the lead content of interior floor dust (13). Soil samples taken from play areas in a yard have a stronger relationship to children’s BLLs than samples from other locations. The EPA defines a soil lead hazard as bare soil that contains 400 ppm of lead in a play area or 1200 ppm in other parts of a yard (19).
Tap water
Lead found in tap water usually is from the corrosion of lead-containing materials found in water distribution systems and household plumbing (22). Exposure to lead in tap water has been reduced by measures taken during the last two decades under the requirements of the 1986 and 1996 amendments to the Safe Drinking Water Act and a subsequent EPA regulation (the Lead and Copper Rule) (2). The latter regulation, which only applies to public water systems, requires those systems to monitor tap water for lead and to implement public education and other measures to reduce lead levels in drinking water if they exceed 15 µg/L in more than 10% of household samples (2). Lead levels are reduced by treating the supplied water to make it less corrosive and, in some cases, by replacing lead water-service lines. These regulations do not apply to the more than 40 million households supplied by private well water that can have elevated levels of lead if the water is corrosive and lead is present in the well pump or household plumbing system (23). In most jurisdictions, there is no monitoring for lead in the drinking water supplied by private wells.
A number of studies, mostly of adults, have attempted to characterize the relationship between lead levels in drinking water and BLLs (24-26). Data from these studies indicate that exposure to water with a lead content close to the EPA action level would not, by itself, be expected to produce an EBLL. However, the individual risk will vary depending upon the circumstances and amount of water consumed. For example, infants consuming formula prepared with lead-contaminated water may be at particular risk because of the large amount of water they consume relative to their body size (27).
Effectiveness and Safety of Lead Hazard Control Measures
Interventions to reduce exposure to lead in the residential environment include measures focused on immediate hazards to current occupants, such as removing or covering nonintact leaded paint, repairing or replacing windows to prevent abrasion of leaded paint on moving surfaces, sealing floors to create smooth and cleanable surfaces, using professional cleaners to control household dust, and covering bare, contaminated soil. Additional interventions may be carried out to prevent lead hazards from developing in the future, such as replacing building components that have leaded paint (whether intact or not) and removing (stripping) leaded paint from components left in the dwelling.
Most studies evaluating the effectiveness of lead hazard control measures for reducing EBLLs have lacked controls. In addition, many studies evaluated interventions prior to the institution of stringent procedures for limiting the contamination of residences with leaded dust. In general, these earlier studies showed that among children with baseline BLLs greater than about 25 µg/dL, measures to remove or repair nonintact leaded paint were followed by declines in BLLs of 20% to 30% over the following year (28). In one controlled study, the decline in BLLs for children in treated dwellings was about twice that of children in untreated dwellings (29).
In homes of children with EBLLs, extensive removal of leaded paint without measures to prevent the children’s exposure to abatement dust and debris has also been associated with increases in the children’s BLLs (30-32). These increases were apparently the result of corresponding increases in house dust lead levels. Consequently, regulations in many jurisdictions now prohibit certain hazardous paint removal methods, such as uncontained power sanding, and require safe work practices, cleaning, and dust lead testing to protect occupants from lead exposure associated with the disturbance of leaded paint. Most jurisdictions require that post-intervention dust lead levels be below clearance standards—the maximum allowable levels of lead. If the dust lead levels in a particular dwelling exceed the clearance standard, that dwelling cannot be reoccupied until additional cleaning or other measures reduce dust lead contamination to less than the clearance threshold. Clearance standards for public and federally assisted housing are 40 µg/ft2 for floors, 250 µg/ft2 for windowsills, and 400 µg/ft2 for window wells. Some state and local jurisdictions have established other clearance standards (19).
Recent longitudinal studies have evaluated leaded paint abatement programs that combined multiple lead hazard control methods (33-35). Interventions used in these programs included measures to prevent the generation of leaded paint chips and dust (treatments to eliminate nonintact leaded paint and windows containing leaded paint subject to friction), leaded dust removal (specialized cleaning), and measures to make floors smooth and cleanable (by sealing or using durable floor coverings). The elimination of leaded paint hazards in the programs relied primarily on component replacement, enclosure, and paint stabilization, with limited on-site paint removal. Although these studies did not include randomly assigned control homes that received no treatment, their results strongly suggest that these treatments resulted in substantial, sustained reductions in interior dust lead loading and little if any risk of children having substantial short-term increases in BLLs. While average BLLs in children occupying treated dwellings fell by approximately 20% to 25% over the following year (from baseline averages in the 5-15 µg/dL range) (35), no data on children in untreated dwellings are available to directly estimate the proportion of decline attributable to the hazard-reduction treatments. In one of these studies, greater initial and sustained reductions in interior dust lead loadings were achieved with more intensive treatments, including window replacement (rather than repair) and the use of durable floor coverings (rather than paints and sealants) (34). However, among children living in the more intensively treated dwellings, average BLL declines following the intervention were not significantly greater than those among children whose dwellings had more limited interventions.
These studies generally involved interventions that left some intact leaded paint in place. The only certain way to prevent future exposure to lead from paint in a dwelling is to remove all leaded paint from the dwelling. However, no studies are available that compare changes in children’s BLLs following the total "deleading" of their dwelling with changes following interventions that leave some leaded paint intact. If many components in a dwelling contain leaded paint, complete deleading may be impractical unless performed as part of a substantial or "gut" renovation.
One study of children with baseline BLLs of 10 to 24 µg/dL found that leaded paint hazard-control measures, including extensive on-site paint removal, resulted in increases in children’s BLLs after abatement (36). These increases occurred despite a protocol for safe work practices, cleaning, and clearance testing. However, the clearance standard used for floors was 200 µg/ft2, which may have been too high to prevent continued or increased exposure to leaded dust when compared with pre-intervention levels. The previously cited impact of relatively "low" levels of lead in house dust on children’s BLLs could explain the increases.
Interventions focused on reducing exposure to leaded dust have been evaluated in several studies (37-39). Household dust control performed repeatedly by professional cleaners was associated with decreases in children’s mean BLL with the greatest benefits seen among children whose dwellings were cleaned at least 20 times during a 1-year follow-up period (38). To be effective, dust control should be conducted every 2-3 weeks. However, simply educating parents about the need to perform dust control as a preventive measure has not proven effective in preventing increases in children’s mean BLLs (39). See Chapter 6, "Educational Interventions for Caregivers," for a detailed discussion of the effects of such education.
In a controlled study, soil removal and replacement with uncontaminated soil was associated with a 15% reduction in BLLs among children whose average baseline BLL was from 10 to 24 µg/dL and who were exposed to high levels of lead in soil (40). Two other studies of the lead abatement of soil with lower baseline contamination showed no reduction in children’s BLLs following such abatement (21, 41).
In the studies noted above and reviewed in detail in Chapter 6, the benefits of environmental interventions have generally been modest—BLL reductions in the range of 10% to 30%. A number of factors might explain the limited effectiveness of these interventions. One such factor is that the interventions were limited in scope: lead hazard control often involved the interior but not the exterior of homes. Another factor is that most interventions were performed in scattered rather than contiguous blocks of homes. Thus, children’s continued exposure to lead from sources in the neighborhood might limit the effectiveness of the interventions. In the Baltimore repair and maintenance study, for example, one comparison group consisted of modern urban homes located in contiguous blocks of such dwellings that were built where older row homes with leaded paint once stood. The geometric mean level of lead contamination in the floor dust of the modern urban homes was less than one-tenth that of older homes that had previously undergone complete lead paint abatement but which were still surrounded by other homes with leaded paint. The geometric mean BLL for children living in the modern homes was one-fourth that of the children living in the older homes (34). A final factor is that the release of lead from bone might also reduce the impact of environmental interventions. By one estimate, an intervention reducing total lead exposure by half for a 5-year-old child would, because of mobilized bone lead stores, cause the child’s BLL to decline by only 25% after 1 year (42).
Recommendations forAssessment and Remediation
General Recommendations
Conduct prompt and effective environmental management. The identification and control of ongoing sources of lead exposure for children with EBLLs should be the highest priority. In addition, identifying children with EBLLs may help officials identify and control potential sources of lead exposure for other children. Because the main objective of environmental management is to reduce lead exposure quickly, investigations should be initiated as soon as possible after a case is identified.
Priority should be placed on responding to children with the highest BLLs and to infants and children less than 2 years of age with any EBLL, because their BLLs are more likely to increase and they are more sensitive to lead’s neurotoxic effects. Table 2.2 shows the recommended maximum time frames for initiating environmental investigations and interventions according to a child’s BLL.
Obtain an exposure history. Investigations to identify sources of a child’s lead exposure should begin with an interview with the child’s caregiver. Whenever possible, the interview should take place at the child’s residence. The interviewer should question the caregiver concerning a range of possible exposure sources. (See Table 2.3 and Appendix I.) It is also important to collect information concerning locations outside the home, such as childcare sites, where the child spends significant amounts of time. The interview should be guided by a checklist tailored to sources of lead exposure found in a given jurisdiction. Checklists facilitate data collection and ensure that potential sources are not overlooked. A sample checklist is provided in Chapter 3, "Medical Assessment and Interventions," and in the 1995 HUD guidelines (3).
Visually inspect the residentialenvironment. A visual inspection can quickly identify areas where deteriorating paint may be contributing to lead exposure and should include windows, porches, bare soil, and common areas in multifamily dwellings, as well as any other locations where the child spends time.
Measure lead in environmental media. Selection of the media to be tested should be guided by the visual inspection and the child’s exposure history. Depending on the inspector’s training, the equipment available, and the media to be tested, environmental analysis may be done either on-site with portable instruments or at an environmental laboratory. Personnel performing environmental sampling and on-site testing should be appropriately trained and be certified as risk assessors (43) or have equivalent qualifications.
Communicate results. Results of investigations, including recommended actions to protect the child from further exposure, should be communicated promptly to caregivers, to primary care providers (PCPs), and, where relevant, to property owners and housing code enforcement authorities. Environmental management activities should be coordinated with other health professionals, including those providing clinical care, case management, and social services.
Specific Recommendations
Since leaded paint and associated lead in house dust and soil are the most common sources of exposure, they should be the focus of environmental investigations and control efforts. State and local health officials should review current policies concerning childhood lead poisoning prevention and revise them as needed to be consistent with the following recommendations.
Measure lead levels in house dust, paint, and bare soil. Investigations of the residential environment of children with EBLLs should focus on immediate lead hazards. At a minimum, testing should include house dust, paints, and similar surface coatings that are not intact or that are located on surfaces subject to friction, and bare soil, especially in play areas. Detailed protocols for sampling and measuring lead in these media can be found in the 1995 HUD guidelines (3).
There is no evidence that complete testing of all building components for leaded paint, regardless of the condition or location of the paint, is helpful in identifying ongoing exposure. Such testing may serve other purposes, however, such as educating occupants about the health hazards of leaded paints, planning the abatement of potential future leaded paint hazards, planning renovation work that may involve disturbance of intact paint, or complying with state and local regulations.
Test for lead in tap water. For homes
served by public water systems, data on lead in drinking water should be
obtained from the water supplier. Many public water systems post data on
the Internet on the quality of drinking water, including results of lead
testing. Links to such data can be found at the following EPA Web site:
http://yosemite.epa.gov/ogwdw/ccr.nsf/America?OpenView.
If prior testing of a public water system shows that lead contamination is
not a problem in homes served by that system, no additional testing is
necessary, unless no other source of a child’s EBLL can be found. For
all other children with EBLLs, including children living in homes served
by private wells, water that the child may consume should be tested. If
necessary, measures should be implemented to prevent the child’s further
exposure to lead (e.g., the use of bottled water or appropriate water
filters). If bottled water is used, fluoride supplementation should be
discussed with the PCP and the caregiver. More information on lead in
drinking water can be found at http://www.epa.gov/ogwdw/dwh/o-ioc/lead.html
or by contacting the Safe Drinking Water hotline at (800) 426-4791 or
hotline-sdwa@epamail.epa.gov. Additional sources of information about lead
in drinking water can be found in Chapter 6, "Educational
Interventions for Caregivers."
Control immediate hazards. Interventions to reduce ongoing exposure should include:
- Replacing or stabilizing the paint in building components containing nonintact leaded paint.
- Replacing or repairing windows and other building systems to eliminate the abrasion of leaded paint.
- Covering or replacing bare lead-contaminated soil.
- Conducting specialized cleaning to reduce lead loading in house dust.
- Sealing or covering floors to make them smooth and cleanable.
Lead hazard control work must be performed in accordance with safe practices by trained workers to avoid exposing workers to unsafe lead levels or increasing the level of lead exposure to occupants. Detailed guidelines for residential lead hazard control work have been published by HUD (3).
On-site removal of intact leaded paint should be kept to a minimum, and safer alternatives, such as component replacement, enclosure, encapsulation, off-site paint removal, and paint-film stabilization should be used when possible. Replacing building components that have intact leaded paint reduces the potential for future lead exposure as the leaded paint deteriorates or is disturbed during renovation. However, such work can generate leaded dust, and workers should follow the precautions described in HUD guidelines.
As discussed previously, there is no evidence that environmental interventions that include complete removal of all leaded paint are more effective at reducing residents’ BLLs than interventions focused on current lead hazards. Furthermore, some evidence suggests that extensive on-site paint removal increases the potential for lead exposure, at least in the short run. The amount of lead in 1 ft2 of paint containing 1 mg/cm2 of lead (approximately 1 g or 1 million Fg) is very large relative to the amount of lead in dust associated with an increased risk for EBLLs (approximately 10 µg/ft2). Thus, performing extensive on-site removal of leaded paint in a dwelling without increasing the occupants’ lead exposure requires a degree of caution that may be difficult to achieve and monitor in the routine, large-scale implementation of health codes.
Long-term control of residential hazards from leaded paint may involve considerable time and expense. Obtaining the compliance of property owners may cause additional delays in reducing residents’ lead exposure. Therefore, interim measures to rapidly reduce lead exposure, including specialized cleaning to reduce exposure to leaded dust, are often required.
Perform clearance testing. Following lead hazard reduction work, repeat testing for lead in house dust is essential to see whether the work has resulted in levels of lead low enough for safe re-occupancy. Post-intervention tests showing increased or persistently high dust lead levels indicate the need for further cleaning or other additional work. Available evidence indicates that current and proposed guidelines for levels of lead in dust on floors may not adequately protect young children and that levels well below these guidelines are achievable and are often present even before intervention. Therefore, the goal should be to attain post-intervention dust lead levels that are as low as is feasible, which is generally less than 10 µg/ft2 on floors (44), and that are at or below baseline levels. Where leaded paint is left in place, periodic monitoring with visual inspection and dust testing should be performed.
Relocate occupants. Temporary occupant relocation is generally required to safely conduct lead hazard control activities that may increase dust lead levels. In some cases, it may be feasible to protect occupants during lead control activities by creating barriers, monitoring the work site daily, and, where appropriate, obtaining serial dust lead measurements. In other cases, permanently relocating occupants to lead-safe housing may be the best way of quickly reducing their lead exposure. Examples of situations that might require relocation include a child living in a dwelling that is structurally unsound or a child living in a dwelling where temporary measures to reduce exposure cannot be taken or are ineffective. Case managers and social workers with experience in assisting families with housing difficulties can play a vital role in assessing the needs and desires of the family and arranging such relocation. A registry of lead-safe housing units in a community can also be helpful. When families permanently relocate from a dwelling where lead hazards are identified, measures should be taken to ensure that the hazards are corrected before any other families with young children occupy the dwelling.
Enforcement of Laws and Regulations
Although enforcing laws and regulations pertaining to lead hazards is not part of case management per se, it is essential to realizing the long-range goal of reducing those hazards. Individual states should provide health and housing officials with the necessary legal authority to require that timely and effective actions are taken to eliminate lead hazards at properties where children with EBLLs have been identified. Health and housing officials should take all steps necessary to prevent additional or repeated cases of children with EBLLs at one property. In a recent national survey, only 18 states indicated that they have legal authority to order remediation at properties where children with EBLLs reside, with only 14 states reporting that their authority was based on lead-specific state laws or regulations (45). State and local governments should examine their laws, ordinances, and housing codes and their enforcement structure to determine whether they are effective in dealing with identified lead hazards and make changes to ensure that children are protected. At a minimum, legislation or ordinances should include the action level at which the law applies, procedures for investigation and re-inspection, standards for lead-safe housing, requirements for completing lead hazard control work (including permits, time frames, permissible methods, waste disposal methods, and clearance standards) and enforcement provisions for noncompliance. In addition, states and localities should be encouraged to develop lead-safe housing standards to protect children from exposure and to ensure that older rental housing is safe for children with EBLLs. Finally, state and local governments should also ensure that they have the ability and necessary resources to take emergency actions (including cleaning the rental units, stabilizing the paint in them, and relocating the occupants) to protect children from identified lead hazards.
Financial Resources for Lead Hazard Control
Many of the homes in which children with EBLLs live are poorly maintained, deteriorated, low-income rental properties. For some economically distressed housing, subsidies and other financial assistance for lead hazard control are required to enable owners to make timely corrections of residential lead hazards. Because resources for addressing lead hazards, particularly in low-income housing, are inadequate in most areas of the country, an increase in resources at the federal, state, and local level should be strongly supported.
In addition, state and local health agencies should develop strong partnerships with local housing and community development organizations, investigate currently available resources for improving low-income housing, and establish mechanisms to apply such resources to lead hazard control in homes of children with EBLLs. A detailed discussion and recommendations concerning financing of lead hazard control work can be found in a HUD publication (46). Some examples of current programs providing resources for this purpose are provided in the following paragraphs.
HUD’s Lead Hazard Control Grant Program (47) enables state or local agencies to provide grants or loans to property owners for conducting lead hazard control measures in low-income housing. Federal regulations require the timely identification and remediation of lead hazards in federally assisted housing, including rental property, whose owners receive tenant-based assistance (Section 8 housing) (19). This program should create a growing pool of lead-safe housing in the future. Decisions on specific priorities for tenant selection under Section 8 and for public housing have been devolved to state and local public-housing agencies. This local flexibility gives health departments in jurisdictions where lead exposure is a major problem an opportunity to urge that priority for assistance be given to families of children with the highest BLLs who are unable to find or afford lead-safe housing.
State and local governments can use HUD’s Community Development Block Grant (CDBG) and HOME Investment Partnership block grant funds to make housing lead-safe. The resources available for state and local block grants under these programs ($6.4 billion in FY 2000) dwarf the $60 million available under the Lead Hazard Control Grant Program. Both the CDBG and HOME programs provide a high degree of flexibility in the use of funds. Indeed, CDBG funds are used by some jurisdictions to support emergency programs dealing with problems such as the breakdown of plumbing or heating systems. A similar approach would be desirable for controlling lead hazards.
State and local governments receiving these block grants must submit a consolidated plan (ConPlan) containing a 5-year strategic plan and a 1-year action plan for their use of these and other available funds. The strategic plan must include actions to evaluate and reduce leaded paint hazards and describe how hazard reduction will be integrated into other housing activities. Evaluating and reducing leaded paint hazards is also a required component of the annual action plan. HUD regulations require that eligible jurisdictions consult with state or local health and child welfare agencies as well as health and social service providers as part of the planning process. State and local health departments with identified lead problems should involve themselves in this planning process to ensure that lead hazard control is a priority for federal CDBG and HOME funding.
Recommendations for Future Research
Technical knowledge concerning the identification and control of lead hazards in homes has advanced greatly over the past several years, resulting in more efficient, safe, and effective environmental management for children with EBLLs. Still, prevention efforts could be improved with further work in several areas.
Additional studies are needed to assess the long-term impact of current lead hazard control methods on children’s EBLLs, especially on levels from 10 to 20 µg/dL. Available data indicate that these methods are safe and effective (i.e., they do not increase children’s BLLs in the short run and they decrease children’s exposure to leaded dust). Because BLL changes over time may be influenced by a child’s age, the season, and secular trends, as well as by regression to the mean, controlled studies are needed to determine how much of the observed decline in BLLs among children living in these dwellings can be attributed to the interventions. Future research should also evaluate the cost effectiveness of interventions.
Until recently, most residential lead hazard control work and studies have involved children who already had EBLLs and presumably relatively high body stores of lead from chronic exposure. The effectiveness of residential lead hazard control in preventing future increases in BLLs among infants and toddlers needs further study.
The level of neighborhood lead exposures appears to make an important contribution to the risk for EBLLs among children. Research is needed to examine how community-level lead sources, such as lead from building demolitions, contribute to children’s exposure. Finally, the effectiveness of community-level interventions to reduce children’s exposure to lead in dwellings and in exterior dust and soil should be further studied.
References
- CDC. Preventing lead poisoning in young children. Atlanta, Georgia: US Department of Health and Human Services, CDC; 1991.
- 2. U.S. Environmental Protection Agency. 40 CFR Ch.1 (7-1-00 Edition). Subpart I—Control of lead and copper. Available at http://www.epa.gov/safewater/regs/cfr141.pdf. Pages 438-70. Accessed 12/19/01.
- Department of Housing and Urban Development (HUD). Guidelines for the evaluation and control of lead-based paint hazards in housing. Washington, DC: HUD; 1995. Available at http://www.hud.gov/lea/learules.html. Accessed 12/19/01.
- Consumer Product Safety Commission. Ban of lead-containing paint and certain consumer products bearing lead-containing paint. 42 CFR § 1303.1-5, 1977.
- Clickner RP, Albright VA, Weitz S. The prevalence of lead-based paint in housing: findings from a national survey. In: Breen JJ, Stroup CR (eds). Lead Poisoning: Exposure, Abatement, Regulation. Boca Raton, FL: CRC Press; 1995:3-12.
- Pirkle JL, Kaufmann RB, Brody DJ, et al. Exposure of the U.S. population to lead, 1991-1994. Environ Health Perspect 1998;106:745-50.
- McElvaine MD, DeUngria EG, Matte TD, et al. Prevalence of radiographic evidence of paint chip ingestion among children with moderate to severe lead poisoning, St. Louis, Missouri, 1989 through 1990. Pediatrics 1992;89:740-2.
- Bornschein RL, Succop P, Kraft KM, et al. Exterior surface dust lead, interior house dust lead and childhood lead exposure in an urban environment. In: Hemphill DD (ed). Trace substances in environmental health, XX. Proceedings of University of Missouri’s 20th Annual Conference, June 1986. Columbia, MO: University of Missouri; 1987.
- Lanphear BP, Roghmann KJ. Pathways of lead exposure in urban children. Environ Res 1997;74:67-73.
- Public Law 102-550. Residential Lead-Based Paint Hazard Reduction Act of 1992.
- U.S. Environmental Protection Agency (EPA). Lead exposure associated with renovation and remodeling activities: Phase III. Wisconsin Childhood Blood Lead Study. Washington, DC: EPA; 1999. EPA 747-R-99-002.
- Lanphear BP, Weitzman M, Winter NL, et al. Lead-contaminated house dust and urban children’s blood lead levels. Am J Public Health 1996;86:1416-21.
- Lanphear BP, Matte TD, Rogers J, et al. The contribution of lead-contaminated house dust and residential soil to children’s blood lead levels. Environ Res 1998;79:51-68.
- Clark CS, Bornschein RL, Succop P, et al. Condition and type of housing as an indicator of potential environmental lead exposure and pediatric blood lead levels. Environ Res 1985;38:46-53.
- Charney E. Sayre J, Coulter M. Increased lead absorption in inner city children: where does the lead come from? Pediatrics 1980;65:226-31.
- Charney E. Lead poisoning in children: the case against household lead dust. In: Chisolm JJ, O’Hara DM (eds). Lead absorption in children—management, clinical, and environmental aspects. Baltimore, MD: Urban & Schwarzenberg; 1982.
- Lanphear BP, Emond M, Jacobs DE, et al. A side-by-side comparison of dust collection methods for sampling lead-contaminated house dust. Environ Res 1995;68:114-23.
- Department of Housing and Urban Development. Requirements for notification, evaluation and reduction of lead-based paint hazards in federally owned residential property and housing receiving federal assistance; final rule. 24 CFR Part 35. Federal Register 1999;64, Number 178: 50139-231.
- U.S. Environmental Protection Agency. Lead: identification of dangerous levels of lead; final rule. 40 CFR Part 745. Federal Register 2001;66(4). Available at http://www.epa.gov/fedrgstr/EPA-TOX/2001/January/Day-05/t84.htm. Accessed 12/19/01.
- U.S. Environmental Protection Agency. Sources of lead in soil: a literature review. Washington, DC: EPA; 1998. EPA 747-R-98-001a.
- U.S. Environmental Protection Agency. Urban soil lead abatement demonstration project. Volume IV: Cincinnati Report. Washington, DC: US EPA;1993. EPA 600/AP93/001d.
- U.S. Environmental Protection Agency. National Primary Drinking Water Regulations: Technical Factsheet on Lead. Available at http://www.epa.gov/safewater/dwh/t-ioc/lead.html. Accessed 3/28/02.
- Estimated use of water in the United States in 1995. U.S. Geological Survey. Available at http://water.usgs.gov/watuse/pdf1995/html/. Accessed 12/19/01.
- U.S. Environmental Protection Agency. Air quality criteria document for lead. Research Triangle Park, NC: EPA; 1986. EPA-600/8-83/028aF-dF.
- Watt GCM, Gilmour WH, Moore MR, et al. Is lead in tap water still a public health problem? An observational study in Glasgow. BMJ 1996; 313:979-81.
- Gulson BL, Giblin AM, Sheehan A, et al. Maintenance of elevated lead levels in drinking water from occasional use and potential impact on blood leads in children. Sci Total Environ 1997;205:271-5.
- Shannon MW, Graef JW. Lead intoxication in infancy. Pediatrics 1992;89:87-90.
- U.S. Environmental Protection Agency (EPA). Review of Studies Addressing Lead Abatement Effectiveness: Updated Edition. Washington DC: EPA; 1998. EPA 747-B-98-001.
- Staes C, Matte T, Copley CG, et al. Retrospective study of the impact of lead-based paint hazard remediation on children’s blood lead levels, St. Louis. Am J Epidemiol 1994;139:1016-26.
- Farfel MR, Chisolm JJ. Health and environmental outcomes of traditional and modified practices for abatement of residential lead-based paint. Am J Public Health 1990;80:1240-5.
- Amitai Y, Graef JW, Brown MJ, et al. Hazards of ‘deleading’ homes of children with lead poisoning. Am J Dis Child 1987;141:758-60.
- Swindell SL, Charney E, Brown MJ, et al. Home abatement and blood lead changes in children with class III lead poisoning. Clin Pediatr 1994;33:536-41.
- Farfel MR, Chisholm JJ, Rohde CA. The longer-term effectiveness of residential lead paint abatement. Environ Res 1994;66:217-21.
- U.S. Environmental Protection Agency (EPA). Lead-based paint abatement and repair and maintenance study in Baltimore: Findings based on two years of follow-up. Washington, DC: EPA; 1997. EPA 747-R-97-005.
- National Center for Lead-Safe Housing. Evaluation of the HUD Lead-Based Paint Hazard Control Grant Program. Fifth interim report. Columbia, MD: National Center for Lead-Safe Housing; 1998.
- Ashengrau A, Beiser A, Bellinger D, et al. Residential lead-based-paint hazard remediation and soil lead abatement: their impact among children with mildly elevated blood lead levels. Am J Public Health 1997;87:1698-702.
- Rhoads GG, Ettinger AS, Weisel CP, et al. The effect of dust lead control on blood lead in toddlers: a randomized trial. Pediatrics 1999;103(3):551-5.
- Ashengrau A, Hardy S, Mackey P, et al. The impact of low technology lead hazard reduction activities among children with mildly elevated blood lead levels. Environ Res 1998;79:41-50.
- Lanphear BP, Howard C, Eberly S, et al. Primary prevention of childhood lead exposure: a randomized trial of dust control. Pediatrics 1999;103:772-7.
- Weitzman M, Ashengrau A, Bellinger D, et al. Lead-contaminated soil abatement and urban children’s blood lead. JAMA 1993;269:1647-54.
- Farrell KP, Brophy MC, Chisholm JJ Jr, et al. Soil lead abatement and children’s blood lead levels in an urban setting. Am J Public Health 1998;88:1837-9.
- Rust SW, Kumar P, Burgoon DA, et al. Influence of bone-lead stores on the observed effectiveness of lead hazard intervention. Environ Res 1999;81:175-84.
- U.S. Environmental Protection Agency. Lead; requirements for lead-based paint activities in target housing and child-occupied facilities; final rule. 40 CFR Part 745. Federal Register 1996;61:45777-830.
- Galke W, Clark S, Wilson J, Jacobs D, Succop P, Dixon S, Bornschein B, McLaine P, Chem M. Evaluation of the HUD Lead Hazard Control Grant Program: Early Overall Findings. Environ Res. 2001; 86:149-156.
- Alliance To End Childhood Lead Poisoning, National Center for Lead-Safe Housing. Another Link in the Chain: state policies and practices for case management and environmental investigation for lead-poisoned children. Available for purchase at <http://www.aeclp.org>. Accessed 12/27/00.
- Lead-Based Paint Hazard Reduction and Financing Task Force. Putting the pieces together: controlling lead hazards in the nation’s housing. Washington DC: US Department of Housing and Urban Development; July 1995. HUD-1547-LBP.
- U.S. Department of Housing and Urban Development. Lead-Based Paint Hazard Control Grant Program. Available at http://www.hud.gov/offices/lead/leagrant.cfm. Accessed 12/19/01.
- Roscoe RJ, Gittleman JL, Deddams JA, et al. Blood lead levels among children of lead-exposed workers: a meta-analysis. Am J Ind Med 1999;36:475-81.
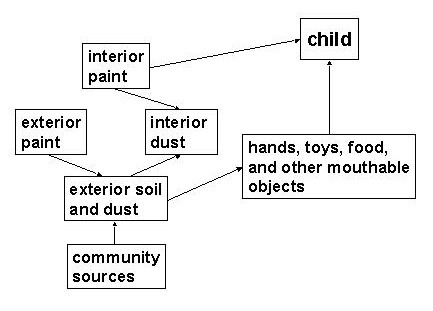 Figure 2.1. Pathways of
Lead Exposure in the Residential Environment
Figure 2.1. Pathways of
Lead Exposure in the Residential Environment
Sources: Bornschein et al., 1987 (reference 8). Lanphear et al., 1997 (reference 9)
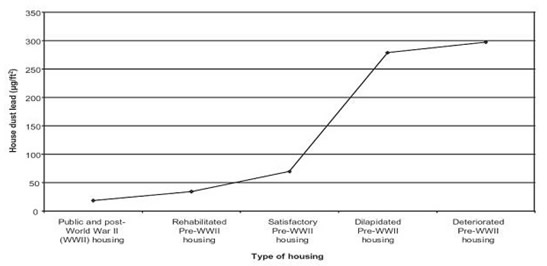
Figure. 2.2. Relationship
of Housing Age and Condition to Dust Lead Levels
Source: Clark et al., 1985 (reference 14)
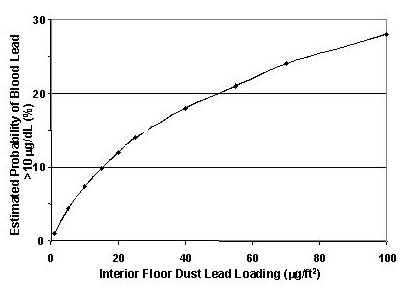
Figure 2.3. Relationship of Dust Lead Levels to Blood Lead Levels in Children Source: Lanphear et al., 1998 (reference 12). Assumes children are exposed to a soil lead concentration equal to the national average level (72 ppm).
Table 2.2. Time Frames for Environmental Investigation and Other Case Management Activities According to a Child’s Blood Lead Levela
| Blood lead level µg/dL)b | Actions | Time frame for beginning intervention |
| Provide caregiver lead education. Provide follow-up testing. Refer the child for social services if necessary. | ||
| Above
actions, plus: If BLLs persist (i.e., 2 venous BLLs in this range at least 3 months apart) or increase, proceed according to actions for BLLs 20-44. |
||
| Above
actions, plus: Provide coordination of care (case management). Provide clinical evaluation and care.c Provide environmental investigation and control current lead hazards. |
||
| Above actions. | ||
| Above actions, plus hospitalize child for chelation therapy immediately. |
|
aThe ACCLPP encourages programs to develop methods to deliver environmental assessment services to caregivers for children living in high-risk dwellings regardless of the children’s blood lead levels. bMicrograms per deciliter of whole blood measured in a venous sample collected following an elevated screening measurement. cThe recommended clinical evaluation is described in Chapter 3, “Medical Assessment and Interventions.” |
Table 2.3. Common Sources of Lead Exposure to Consider in an Environmental
Investigation
(less common sources should be considered where appropriate—see
Appendix I)
| Source | Standardsa/Comments | References |
| New paint: 600 ppm in dried paint film.Existing paint in structures built prior to 1978: 1 mg/cm2 or 0.5% Hazard is increased if leaded paint is deteriorated; present on surfaces subject to friction (e.g., window sashes); or disturbed during maintenance, repair, and renovation, especially during surface preparation for repainting. | ||
| Floors:
40 micrograms per square foot µg/ft2)b Interior window sills: 250 µg/ft2 Window troughs: 400 µg/ft2 Research shows children to be at increased risk for EBLLs at floor lead loading substantially below standard. |
18, 19 | |
| Bare
play area soil: 400 ppm All other soil: 1200 ppm Dust on paved surfaces in urban areas often contains elevated lead concentrations. |
||
| First draw from tap (stagnant sample): 15 ppb Probability of contamination depends on the chemistry of the water. For communities served by public water systems, available data may indicate whether testing is likely to be helpful. | ||
| House dust may be contaminated with lead (see above) indirectly via contaminated work clothes, shoes, or hair. Direct contamination can occur from hobbies that generate lead fumes (from heating) or dust. |
aNote: Most standards for lead in environmental media are established on the basis of measurement feasibility or for primary prevention purposes. These standards cannot be used to determine the cause of an EBLL, which requires that environmental measurements be interpreted in the context of a careful exposure history.
bEPA has established standards of 40 and 250 µg/ft2for hazardous levels of lead in dust on floors and sills, respectively. HUD has established interim standards, 25 and 125 µg/ft2, that apply if a more limited assessment known as a "lead hazard screen" is performed. The EPA standard for window troughs is intended only for clearance testing after lead hazard reduction activities.
Contact Us:
- Centers for Disease Control and Prevention
1600 Clifton Rd
Atlanta, GA 30333 - 800-CDC-INFO
(800-232-4636)
TTY: (888) 232-6348 - cdcinfo@cdc.gov

