Some Blood Pressure Drugs Might Help Slow Alzheimer's: Study
Fewer telltale brain plaques found in patients on angiotensin receptor blockers
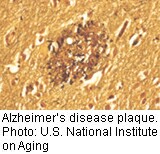 TUESDAY, Sept. 11 (HealthDay News) -- Angiotensin receptor blockers, drugs commonly taken to control high blood pressure, appear to reduce the amount of plaque in the brains of Alzheimer's patients and others, a new study shows.
These results were found when patients with high blood pressure on drugs such as losartan (Cozaar) died and underwent an autopsy. These brain plaques are a hallmark of Alzheimer's disease. Whether, however, these drug also improve mental function isn't known, the researchers added.
"[It] would have to be proven in a clinical trial whether these effects seen in an autopsy study manifest themselves in a clinical setting," said lead researcher Dr. Ihab Hajjar, an assistant professor at the University of Southern California Keck School of Medicine. "But since we don't have any treatment for Alzheimer's, it's worth pursuing."
Candesartan (Atacand), irbesartan (Avapro), olmesartan (Benicar), valsartan (Diovan), telmisartan (Micardis) and eprosartan (Teveten) are other angiotensin receptor blockers approved by the U.S. Food and Drug Administration.
Although this study can't determine whether angiotensin receptor blockers improve mental function in Alzheimer's patients, Hajjar pointed out there is a connection between blood pressure and brain health, and the choice of blood-pressure lowering drugs may make a difference in maintaining brain function.
The report was published online in the Sept. 10 issue of the Archives of Neurology.
For the study, Hajjar's team autopsied the brains of 890 patients with hypertension who had been taking various medications to lower their blood pressure. Some of these patients had Alzheimer's disease while others didn't. Some had been diagnosed with dementia but not Alzheimer's. Most were in their 70s or 80s when they died.
Patients taking angiotensin receptor blockers had fewer brain plaques whether or not they had been diagnosed with Alzheimer's, the researchers found.
Moreover, these results were seen only among those who had been taking angiotensin receptor blockers and not among patients taking any other blood pressure medications.
Patients treated with angiotensin receptor blockers had fewer brain plaques than people not treated with any blood pressure drug, the study also found.
"Uncontrolled hypertension is a recognized risk for Alzheimer's disease and for vascular dementia, so this is unsurprising, but highly welcome, news," said Dr. Sam Gandy, the Mount Sinai chair in Alzheimer's Disease Research and associate director of the Mount Sinai Alzheimer's Disease Research Center, in New York City.
Hajjar's team is looking at the effects of this group of drugs in people who Alzheimer's or other forms of dementia. A pilot study found they did slow or prevent decline in areas of the brain that are susceptible to damage from high blood pressure.
While the new study found an association between these blood pressure medicines and levels of brain plaque, it did not prove a cause-and-effect relationship.
More information
For more about Alzheimer's Disease, visit the Alzheimer's Association  . .

|