NIH Research Matters
September 17, 2012
Study Suggests New Approaches to Burkitt Lymphoma
A new study revealed insights into how Burkitt lymphoma differs from other lymphomas. The researchers identified several cancer-related genes and pathways that could serve as targets for future treatments.
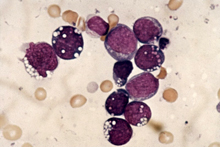
Burkitt lymphoma cells. Image courtesy of Wellcome Photo Library. All rights reserved by Wellcome Images.
Non-Hodgkin lymphomas are cancers that arise from white blood cells. The disease originates in B cells, which are antibody-producing cells that protect the body against bacteria and viruses. Burkitt lymphoma and diffuse large B-cell lymphoma (DLBCL) are 2 different types of aggressive non-Hodgkin lymphoma that require different treatments.
Earlier studies led by Dr. Louis Staudt from NIH's National Cancer Institute (NCI) showed that Burkitt lymphoma can be readily distinguished from DLBCL based on signatures of gene activity. Notably, the oncogene MYC activates many genes that are more highly expressed in Burkitt lymphoma than in DLBCL.
In their new study, Staudt's team set out to identify genes and pathways that cooperate with MYC in Burkitt lymphoma. The researchers sequenced biopsy samples from 28 patients with sporadic Burkitt lymphoma and 13 different Burkitt lymphoma cell lines. They compared the data to published data from 80 DLBCL biopsies. They then confirmed their genetic findings through additional sequencing methods and larger sample sizes. Results appeared online in Nature on August 12, 2012.
The scientists found a number of unique genes that were mutated in each disease. The findings show that these lymphomas use fundamentally different mechanisms to become cancerous. For example, mutations in the genes TCF3 and ID3 were found in 70% of sporadic Burkitt lymphoma patients. TCF3 is needed for B cell function and ID3 is known to inhibit TCF3. Mutations in these genes were rare in DLBCL.
Most of the mutations in TCF3 and ID3 led to increased signaling from the B cell receptor, a protein on the B cell surface. These signals promote survival of Burkitt lymphoma tumor cells by turning on one of the most frequently activated signaling pathways in human cancer, the PI(3) kinase pathway. Development of PI(3) kinase inhibitors for use in cancer patients is well underway, but no inhibitor has yet been tested in patients with Burkitt lymphoma.
The team also found that the CCND3 gene, which is activated by TCF3, was mutated in 38% of sporadic Burkitt lymphoma patients. This gene encodes a protein that interacts with CDK6, which promotes the proliferation of Burkitt lymphoma cells. Unexpectedly, the scientists found that the cells not only stopped dividing but also died when CDK6 was blocked with a drug. This result suggests the protein may be a promising therapeutic target.
“Our research suggests a number of targeted therapies that might be less toxic than the high-dose chemotherapy that is typically given to patients with Burkitt lymphoma in the U.S., even though they have cure rates approaching 90%,” Staudt says. “Such targeted therapies might also help children in Africa with Burkitt lymphoma, who only have cure rates of about 50% because intensive chemotherapy cannot be delivered safely in that setting.”
Related Links:
-
Non-Hodgkin Lymphoma:
http://www.cancer.gov/cancertopics/types/non-hodgkin/ - Gene Expression Profiling Distinguishes Lymphomas:
http://www.nih.gov/researchmatters/june2006/06092006lymphoma.htm - Mutations Contribute to Type of Non-Hodgkin Lymphoma:
http://www.nih.gov/researchmatters/january2010/ 01252010lymphoma.htm - Gene Activity Can Predict Survival Rates of Patients with Lymphoma:
http://www.nih.gov/researchmatters/december2008/ 12082008genelymphoma.htm
Reference: Nature. 2012 Aug 12. doi: 10.1038/nature11378. [Epub ahead of print]. PMID:22885699.
Editor’s Picks
Contact Us
Phone: 301-435-7489
E-mail: nihresearchmatters@od.nih.gov
Mailing Address:
NIH Research Matters
Bldg. 31, Rm. 5B64A, MSC 2094
Bethesda, MD 20892-2094
About NIH Research Matters
Harrison Wein, Ph.D., Editor
Vicki Contie, Assistant Editor
NIH Research Matters is a weekly update of NIH research highlights from the Office of Communications and Public Liaison, Office of the Director, National Institutes of Health.
Social Media Links