General Information About Intraocular (Eye) Melanoma
Key Points for This Section
- Intraocular melanoma is a disease in which malignant (cancer) cells form in the tissues of the eye.
- Age and sun exposure may increase the risk of developing intraocular melanoma.
- Possible signs of intraocular melanoma include a dark spot on the iris or blurred vision.
- Tests that examine the eye are used to help detect (find) and diagnose intraocular melanoma.
- Certain factors affect prognosis (chance of recovery) and treatment options.
Intraocular melanoma is a disease in which malignant (cancer) cells form in the tissues of the eye.
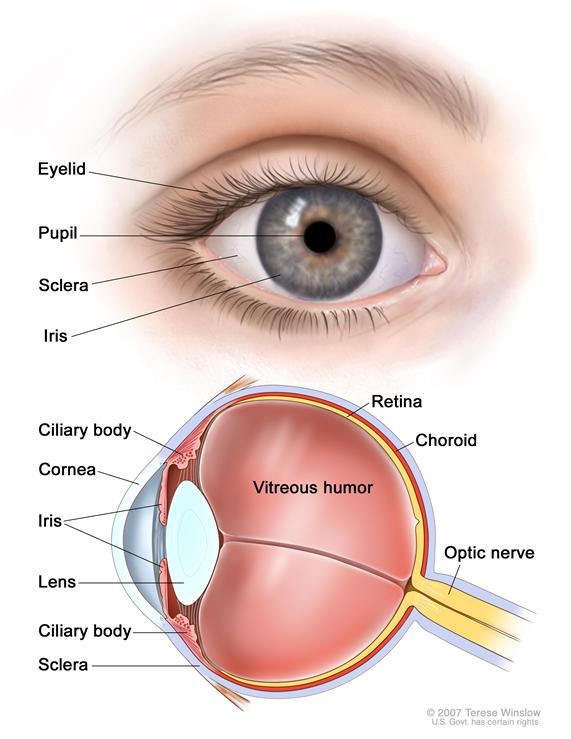
Intraocular melanoma begins in the middle of 3 layers of the wall of the eye. The outer layer includes the white sclera (the "white of the eye") and the clear cornea at the front of the eye. The inner layer has a lining of nerve tissue, called the retina, which senses light and sends images along the optic nerve to the brain.
The middle layer, where intraocular melanoma forms, is called the uvea or uveal tract, and has 3 main parts:
- Iris
The iris is the colored area at the front of the eye (the "eye color"). It can be seen through the clear cornea. The pupil is in the center of the iris and it changes size to let more or less light into the eye.
- Ciliary body
The ciliary body is a ring of tissue with muscle fibers that change the size of the pupil and the shape of the lens. It is found behind the iris. Changes in the shape of the lens help the eye focus. The ciliary body also makes the clear fluid that fills the space between the cornea and the iris.
- Choroid
The choroid is the layer of blood vessels that bring oxygen and nutrients to the eye. Most intraocular melanomas begin in the choroid.
Intraocular melanoma is a rare cancer, but it is the most common eye cancer in adults.
Age and sun exposure may increase the risk of developing intraocular melanoma.
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn’t mean that you will not get cancer. People who think they may be at risk should discuss this with their doctor. Risk factors for intraocular melanoma include the following:
- Being exposed to natural sunlight or artificial sunlight (such as from tanning beds) over long periods of time.
- Having a fair complexion, which includes the following:
- Fair skin that freckles and burns easily, does not tan, or tans poorly.
- Blue or green or other light-colored eyes.
- Older age.
- Being white.
Possible signs of intraocular melanoma include a dark spot on the iris or blurred vision.
Intraocular melanoma may not cause any early symptoms. It is sometimes found during a routine eye exam when the doctor dilates the pupil and looks into the eye. The following symptoms may be caused by intraocular melanoma or by other conditions. A doctor should be consulted if any of these problems occur:
- A dark spot on the iris.
- Blurred vision.
- A change in the shape of the pupil.
- A change in vision.
Glaucoma may develop if the tumor causes the retina to separate from the eye. If this happens, there may be no symptoms, or symptoms may include the following:
- Eye pain.
- Blurred vision.
- Eye redness.
- Nausea.
Tests that examine the eye are used to help detect (find) and diagnose intraocular melanoma.
The following tests and procedures may be used:
- Eye exam with dilated pupil: An examination of the eye in which the pupil is dilated (enlarged) with medicated eyedrops to allow the doctor to look through the lens and pupil to the retina. The inside of the eye, including the retina and the optic nerve, is examined using an instrument that produces a narrow beam of light. This is sometimes called a slit-lamp exam. The doctor may take pictures over time to keep track of changes in the size of the tumor and how fast it is growing.
- Indirect ophthalmoscopy: An examination of the inside of the back of the eye using a small magnifying lens and a light.
- Ultrasound exam of the eye: A procedure in which high-energy sound waves (ultrasound) are bounced off the internal tissues of the eye to make echoes. Eye drops are used to numb the eye and a small probe that sends and receives sound waves is placed gently on the surface of the eye. The echoes make a picture of the inside of the eye. The picture, called a sonogram, shows on the screen of the ultrasound monitor.
- Transillumination of the globe and iris: An examination of the iris, cornea, lens, and ciliary body with a light placed on either the upper or lower lid.
- Fluorescein angiography: A procedure to look at blood vessels and the flow of blood inside the eye. An orange fluorescent dye (fluorescein) is injected into a blood vessel in the arm. As the dye travels through blood vessels of the eye, a special camera takes pictures of the retina and choroid to detect any blockage or leakage.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) and treatment options depend on the following:
- The type of melanoma cells (how they look under a microscope).
- The size of the tumor.
- Which part of the eye the tumor is in (the iris, ciliary body, or choroid).
- Whether the tumor has spread within the eye or to other places in the body.
- The patient's age and general health.
- Whether the tumor has recurred (come back) after treatment.
In patients with small tumors that have not spread, intraocular melanoma can be cured and vision can usually be saved.


 Back to Top
Back to Top