Breast Changes and Conditions: Getting Follow-up Test Results
Test results will tell if you have:
Breast changes that are not cancer
Breast changes that are not cancer, but increase your risk of cancer
Breast changes that may become cancer
Breast cancer
Breast changes that are not cancer
These changes are not cancer and do not increase your risk of breast cancer. They are called benign changes.
Adenosis: Small, round lumps, or a lumpy feeling that are caused by enlarged breast lobules. Sometimes the lumps are too small to be felt. If there is scar-like tissue, the condition may be painful and is called sclerosing adenosis.
Cysts: Lumps filled with fluid. Breast cysts often get bigger and may be painful just before your menstrual period begins. Cysts are most common in premenopausal women and in women who are taking menopausal hormone therapy.
Fat necrosis: Round, firm lumps that usually don't hurt. The lumps most often appear after an injury to the breast, surgery, or radiation therapy.
Fibroadenomas: Hard, round lumps that may feel like a small marble and move around easily. They are usually painless and are most common in young women under 30 years old.
Intraductal papilloma: A wart-like growth in a milk duct of the breast. It's usually found close to the nipple and may cause clear, sticky, or bloody discharge from the nipple. It may also cause pain and a lump. It is most common in women 35-55 years old.
| Ask your doctor when you will get your test results. See the chart in Breast Conditions and Follow-Up Care for follow-up information. |
Breast changes that are not cancer, but increase your risk of cancer
These conditions are not cancer, but having them increases your risk of breast cancer. They are considered risk factors for breast cancer. Other risk factors include, for example, your age and a family history of breast cancer.
- Atypical hyperplasia:
- Atypical lobular hyperplasia (ALH) is a condition in which abnormal cells are found in the breast lobules.
- Atypical ductal hyperplasia (ADH) is a condition in which abnormal cells are found in the breast ducts.
- Lobular carcinoma in situ (LCIS) is a condition in which abnormal cells are found in the breast lobules. There are more abnormal cells in the lobule with LCIS than with ALH. Since these cells have not spread outside the breast lobules, it's called "in situ," which is a Latin term that means "in place."
The abnormal cells found in these conditions are not cancer cells. If you have ALH, ADH, or LCIS, talk with a doctor who specializes in breast health to make a plan that works best for you. Depending on your personal and family medical history, it may include:
- Mammograms every year
- Clinical breast exams every 6 to 12 months
- Tamoxifen (for all women) or raloxifene (for postmenopausal women). These drugs have been shown to lower some women's risk of breast cancer.
- Surgery. A small number of women with LCIS and high risk factors for breast cancer may choose to have surgery.
- Clinical trials. Talk with your health care provider about whether a clinical trial is a good choice for you.
|
Breast changes that may become cancer
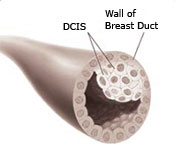
Ductal carcinoma in situ (DCIS): DCIS is a condition in which abnormal cells are found in the lining of a breast duct. These cells have not spread outside the duct to the breast tissue. This is why it is called "in situ," which is a Latin term that means "in place." You may also hear DCIS called Stage 0 breast carcinoma in situ or noninvasive cancer.
Since it's not possible to determine which cases of DCIS will become invasive breast cancer, it's important to get treatment for DCIS. Talk with a doctor who specializes in breast health to learn more. Treatment for DCIS is based on how much of the breast is affected, where DCIS is in the breast, and its grade. Most women with DCIS are cured with proper treatment.
Treatment choices for DCIS include:
- Lumpectomy. This is a type of breast-conserving surgery or breast-sparing surgery. It is usually followed by radiation therapy.
- Mastectomy. This type of surgery is used to remove the breast or as much of the breast tissue as possible.
- Tamoxifen. This drug may also be taken to lower the chance that DCIS will come back, or to prevent invasive breast cancer.
- Clinical trials. Talk with your health care provider about whether a clinical trial is a good choice for you.
Breast cancer
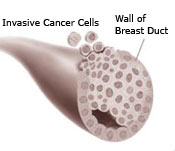
Breast cancer is a disease in which cancer cells form in the tissues of the breast. Breast cancer cells:
- Grow and divide without control
- Invade nearby breast tissue
- May form a mass called a tumor
- May metastasize, or spread, to the lymph nodes or other parts of the body
After breast cancer has been diagnosed, tests are done to find out the extent, or stage, of the cancer. The stage is based on the size of the tumor and whether the cancer has spread. Treatment depends on the stage of the cancer.
For more information about breast cancer and to get answers to any questions you may have, call 1-800-4-CANCER (1-800-422-6237). One free booklet you can ask for is: What You Need To Know About Breast Cancer. You can also visit the National Cancer Institute (NCI) online at www.cancer.gov.
| Get a second opinion |
|---|
You may want to talk with another doctor to get a second opinion on your diagnosis or on your treatment. Many women do. And remember—it's important to talk with a doctor who specializes in breast cancer or in the breast condition that you have. You can talk with your health care provider to find:
Most doctors welcome a second opinion, especially when treatment is involved. Getting a second opinion is often covered, or even required, by your health insurance. Talking with another doctor can give you peace of mind. It can also help you make the best choices about your health. |


