Other Rare Unusual Cancers of Childhood
Multiple Endocrine Neoplasia Syndromes
Pheochromocytoma and Paraganglioma
Skin Cancer (Melanoma, Squamous Cell Cancer, Basal Cell Cancer)
Chordoma
Cancer of Unknown Primary Site
Multiple Endocrine Neoplasia Syndromes
Multiple endocrine neoplasia (MEN) syndromes
Multiple endocrine neoplasia (MEN) syndromes are inherited disorders that affect the endocrine system. The endocrine system is made up of glands and cells that make hormones and release them into the blood. MEN syndromes may cause hyperplasia (the growth of too many normal cells) or tumors that may be benign (not cancer) or malignant (cancer).
There are several types of MEN syndrome and each type may cause different conditions or cancers. Patients and family members with an increased risk of these syndromes should have genetic counseling and tests to check for the syndromes.
The two main types of MEN syndromes are MEN1 and MEN2:
- MEN1 syndrome is also called Werner syndrome. This syndrome can cause tumors in the parathyroid, pancreas, and pituitary glands. A diagnosis of MEN1 syndrome is usually made when tumors are found in two or three of these glands. MEN1 syndrome may also cause tumors in the adrenal glands, gastrointestinal tract, fibrous tissue, and fat cells. The prognosis (chance of recovery) is usually good.
The most common sign of MEN1 syndrome is hypercalcemia. Hypercalcemia may cause weakness, feeling very tired, nausea and vomiting, loss of appetite, being very thirsty and urinating more than usual, and constipation.
Children who are diagnosed with MEN1 syndrome are checked for signs of cancer starting at age 5 and continuing for the rest of their life. Talk to your doctor about the tests and procedures that should be done to check for signs of cancer and how often they should be done.
- MEN2 syndrome includes three subgroups:
- MEN2A syndrome
MEN2A syndrome is also called Sipple syndrome. A diagnosis of MEN2A syndrome may be made when the patient or the patient's parents, brothers, sisters, or children have two or more of the following tumors:
- Medullary thyroid cancer.
- Pheochromocytoma (a tumor of the adrenal gland).
- Parathyroid gland cancer.
Symptoms of medullary thyroid cancer may include the following:
- A lump in the neck.
- Trouble breathing.
- Trouble swallowing.
- Hoarseness.
Symptoms of pheochromocytoma may include:
- Pain in the abdomen or chest.
- Fast or irregular heart beat.
- Being irritable or nervous.
- Headache.
Symptoms of parathyroid gland cancer may include:
- Hypercalcemia.
- Pain in the abdomen, side, or back that doesn't go away.
- Pain in the bones.
- A broken bone.
- A lump in the neck.
- Change in voice, such as hoarseness.
- Trouble swallowing.
Family members of patients with the MEN2A syndrome should have genetic counseling and be tested in early childhood, before age 5, for the gene changes that lead to this type of cancer.
A small number of medullary thyroid cancers may occur at the same time as Hirschsprung disease (chronic constipation that begins when a child is an infant), which has been found in some families with MEN2A syndrome. Hirschsprung disease may appear before other signs of MEN2A syndrome do. Patients who are diagnosed with Hirschsprung disease should be checked for certain gene changes that cause MEN2A syndrome.
- MEN2B syndrome
Patients with MEN2B syndrome may have a slender body build with long, thin arms and legs. The lips may appear thick and bumpy because of benign tumors in the mucous membranes. MEN2B syndrome may cause the following conditions:
- Medullary thyroid cancer.
- Parathyroid hyperplasia.
- Adenomas.
- Pheochromocytoma.
- Nerve cell tumors in the mucous membranes or other places.
- Familial medullary carcinoma of the thyroid (FMTC)
This type of MEN2 syndrome causes medullary thyroid cancer. A diagnosis of FMTC may be made when 2 or more family members have medullary thyroid cancer and no family members have parathyroid or adrenal gland problems.
- MEN2A syndrome
Tests used to diagnose and stage MEN syndromes depend on the symptoms and the patient's family history. They may include:
- Physical exam and history.
- Blood chemistry studies.
- Ultrasound.
- MRI.
- CT scan.
- PET scan.
- Fine-needle aspiration (FNA) or surgical biopsy.
See the General Information section for a description of these tests and procedures.
Other tests and procedures used to diagnose MEN syndromes include the following:
- Genetic testing: A test to analyze DNA and check for a genetic alteration that may indicate an increased risk for developing a specific disease or disorder.
- Blood hormone studies: A procedure in which a blood sample is checked to measure the amounts of certain hormones released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. The blood may be checked for abnormal levels of thyroid-stimulating hormone (TSH). TSH is made by the pituitary gland in the brain. It stimulates the release of thyroid hormone and controls how fast follicular thyroid cells grow. The blood may also be checked for high levels of the hormone calcitonin or parathyroid hormone (PTH).
- Radioactive iodine scan (RAI scan): A procedure to find areas in the body where thyroid cancer cells may be dividing quickly. Radioactive iodine (RAI) is used because only thyroid cells take up iodine. A very small amount of RAI is swallowed, travels through the blood, and collects in thyroid tissue and thyroid cancer cells anywhere in the body. Abnormal thyroid cells take up less iodine than normal thyroid cells do. Areas that do not take up the iodine normally are called cold spots. Cold spots show up lighter in the picture made by the scan. They can be either benign (not cancer) or malignant, so a biopsy is done to find out if they are cancer.
- Sestamibi scan: A type of radionuclide scan used to find an overactive parathyroid gland. A small amount of a radioactive substance called technetium 99 is injected into a vein and travels through the bloodstream to the parathyroid gland. The radioactive substance will collect in the overactive gland and show up brightly on a special camera that detects radioactivity.
- Angiogram: A procedure to look at blood vessels and the flow of blood. A contrast dye is injected into a blood vessel. As the contrast dye moves through the blood vessel, x-rays are taken to see if there are any blockages.
- Venous sampling for an overactive parathyroid gland: A procedure in which a sample of blood is taken from veins near the parathyroid glands. The sample is checked to measure the amount of parathyroid hormone released into the blood by each gland. Venous sampling may be done if blood tests show there is an overactive parathyroid gland but imaging tests don’t show which one it is.
- Somatostatin receptor scintigraphy: A type of radionuclide scan that may be used to find tumors. A small amount of radioactive octreotide (a hormone that attaches to tumors) is injected into a vein and travels through the blood. The radioactive octreotide attaches to the tumor and a special camera that detects radioactivity is used to show where the tumors are in the body. This procedure is also called octreotide scan and SRS.
- MIBG scan: A procedure used to find neuroendocrine tumors, such as pheochromocytoma. A very small amount of radioactive material called MIBG is injected into a vein and travels through the bloodstream. Pheochromocytoma cells take up the radioactive material and are detected by a device that measures radiation.
- Blood catecholamine studies: A procedure in which a blood sample is checked to measure the amount of certain catecholamines released into the blood. Substances caused by the breakdown of these catecholamines are also measured. An unusual (higher- or lower-than-normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. Higher-than-normal amounts may be a sign of pheochromocytoma.
- Twenty-four-hour urine test: A test in which urine is collected for 24 hours to measure the amounts of catecholamines in the urine. Substances caused by the breakdown of these catecholamines are also measured. An unusual (higher- or lower-than-normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. Higher-than-normal amounts may be a sign of pheochromocytoma.
- Pentagastrin stimulation test: A test in which blood samples are checked to measure the amount of calcitonin in the blood. Calcium gluconate and pentagastrin are injected into the blood and then several blood samples are taken over the next 5 minutes. If the level of calcitonin in the blood increases, it may be a sign of medullary thyroid cancer.
Treatment
There are several types of MEN syndrome, and each type may need different treatment:
- Patients with the MEN1 syndrome are treated for parathyroid, pancreatic and pituitary tumors.
- Patients with the MEN2A syndrome usually have surgery to remove the thyroid by age 5 or earlier if genetic tests show certain gene changes. The surgery is done to diagnose cancer or to prevent cancer from forming or spreading.
- Infants with the MEN2B syndrome may have the thyroid removed to prevent cancer.
- Patients with Hirschsprung disease and certain gene changes may have the thyroid removed to prevent cancer.
- A clinical trial of targeted therapy with a tyrosine kinase inhibitor for medullary thyroid cancer.
Pheochromocytoma and paraganglioma are rare tumors that come from the same type of nerve tissue.
- Pheochromocytoma forms in the adrenal glands. There are two adrenal glands, one on top of each kidney in the back of the upper abdomen. Each adrenal gland has two parts. The outer layer of the adrenal gland is the adrenal cortex. The center of the adrenal gland is the adrenal medulla. Pheochromocytoma is a tumor of the adrenal medulla. The adrenal glands make important hormones called catecholamines. Adrenaline (epinephrine) and noradrenaline (norepinephrine) are two types of catecholamines that help control heart rate, blood pressure, blood sugar, and the way the body reacts to stress. Some pheochromocytomas release extra adrenaline and noradrenaline into the blood and cause symptoms of disease.
- Paraganglioma forms outside the adrenal glands near the carotid artery, along nerve pathways in the head and neck, and in other parts of the body. Some paragangliomas make extra catecholamines called adrenaline and noradrenaline. The release of extra adrenaline and noradrenaline into the blood may cause symptoms of disease.
Risk Factors, Symptoms, and Diagnostic and Staging Tests
Anything that increases your chance of getting a disease is called a risk factor. Having a risk factor doesn't mean that you will get cancer; not having risk factors doesn’t mean that you will not get cancer. Talk to your doctor if you think you may be at risk.
The risk of pheochromocytoma or paraganglioma is increased by having any of the following inherited syndromes or gene changes:
- Multiple endocrine neoplasia 1 syndrome.
- Multiple endocrine neoplasia 2 syndrome (MEN2A and MEN2B).
- von Hippel-Lindau disease (VHL).
- Neurofibromatosis type 1 (NF1).
- Carney-Stratakis dyad (paraganglioma and gastrointestinal stromal tumor [GIST]).
- Carney triad (paraganglioma, GIST, and pulmonary chondroma).
- Changes in certain genes including SDHD, SDHB, SDHA, and TMEM127.
More than half of the children and adolescents diagnosed with pheochromocytoma or paraganglioma have an inherited syndrome or gene change that increased the risk of cancer. Genetic counseling (a discussion with a trained professional about inherited diseases) and testing is an important part of the treatment plan.
Some tumors do not make extra adrenaline or noradrenaline and do not cause symptoms. These tumors may be found when a lump forms in the neck or when a test or procedure is done for another reason. Symptoms of pheochromocytoma and paraganglioma occur when too much adrenaline or noradrenaline is released into the blood. These and other symptoms may be caused by pheochromocytoma and paraganglioma. Other conditions may cause the same symptoms. Check with your doctor if you have any of the following problems:
- High blood pressure.
- Headache.
- Heavy sweating for no known reason.
- A strong, fast, or irregular heartbeat.
- Being shaky.
- Being extremely pale.
These symptoms may come and go but high blood pressure is more likely to occur for long periods of time in young patients. These symptoms may also occur with physical activity, injury, anesthesia, surgery to remove the tumor, eating foods such as chocolate and cheese, or passing urine (if the tumor is in the bladder).
Tests used to diagnose and stage pheochromocytoma and paraganglioma depend on the symptoms and the patient's family history. They may include:
- Physical exam and history.
- PET scan.
- CT scan (CAT scan).
- MRI (magnetic resonance imaging).
See the General Information section for a description of these tests and procedures.
Other tests and procedures used to diagnose pheochromocytoma and paraganglioma include the following:
- Plasma-free metanephrines test: A blood test that measures the amount of metanephrines in the blood. Metanephrines are substances that are made when the body breaks down adrenaline or noradrenaline. Pheochromocytomas and paragangliomas can make large amounts of adrenaline and noradrenaline and cause high levels of metanephrines in both the blood and urine.
- Blood catecholamine studies: A procedure in which a blood sample is checked to measure the amount of certain catecholamines (adrenaline or noradrenaline) released into the blood. Substances caused by the breakdown of these catecholamines are also measured. An unusual (higher- or lower-than-normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. Higher-than-normal amounts may be a sign of pheochromocytoma or paraganglioma.
- Twenty-four-hour urine test: A test in which urine is collected for 24 hours to measure the amounts of catecholamines (adrenaline or noradrenaline) or metanephrines in the urine. Substances caused by the breakdown of these catecholamines are also measured. An unusual (higher- or lower-than-normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. Higher-than-normal amounts may be a sign of pheochromocytoma or paraganglioma.
- MIBG scan: A procedure used to find neuroendocrine tumors, such as pheochromocytoma and paraganglioma. A very small amount of radioactive material called MIBG is injected into a vein and travels through the bloodstream. Pheochromocytoma cells take up the radioactive material and are detected by a device that measures radiation.
- Somatostatin receptor scintigraphy: A type of radionuclide scan that may be used to find tumors. A small amount of radioactive octreotide (a hormone that attaches to tumors) is injected into a vein and travels through the blood. The radioactive octreotide attaches to the tumor and a special camera that detects radioactivity is used to show where the tumors are in the body. This procedure is also called octreotide scan and SRS.
Treatment
Treatment of pheochromocytoma and paraganglioma in children may include the following:
- Surgery to completely removed the tumor.
- Combination chemotherapy or treatment with high-dose 131I-MIBG for tumors that have spread.
Before surgery, drug therapy with alpha-blockers to control blood pressure and beta-blockers to control heart rate are given. If both adrenal glands are removed, life-long hormone therapy to replace hormones made by the adrenal glands is needed after surgery.
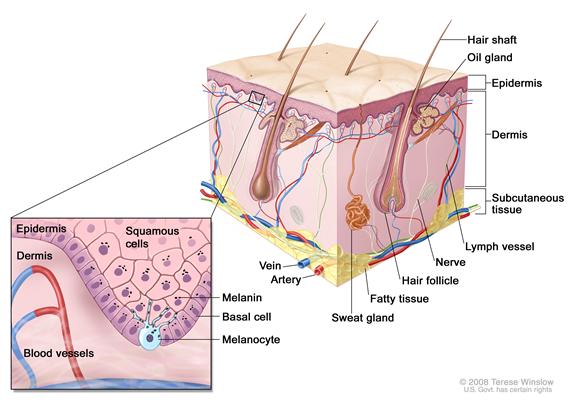
Skin Cancer (Melanoma, Squamous Cell Cancer, Basal Cell Cancer)Skin cancer is a disease in which malignant (cancer) cells form in the tissues of the skin. The skin is the body’s largest organ. It protects against heat, sunlight, injury, and infection. Skin also helps control body temperature and stores water, fat, and vitamin D. The skin has several layers, but the two main layers are the epidermis (upper or outer layer) and the dermis (lower or inner layer). Skin cancer begins in the epidermis, which is made up of three kinds of cells:
- Squamous cells: Thin, flat cells that form the top layer of the epidermis.
- Basal cells: Round cells under the squamous cells.
- Melanocytes: Found in the lower part of the epidermis, these cells make melanin, the pigment that gives skin its natural color. When skin is exposed to the sun, melanocytes make more pigment and cause the skin to darken.
There are three types of skin cancer:
Melanoma
Even though melanoma is rare, it is the most common skin cancer in children. It occurs more often in children aged 10 to 19 years. Melanoma rates in the United States have slowly increased since 1975.
The risk of having melanoma is increased by the following:
- Giant melanocytic nevi (large black spots, which may cover the trunk and thigh).
- Xeroderma pigmentosum.
- Certain disorders of the immune system.
- Multiple endocrine neoplasia Type I (MEN1) syndrome (Werner syndrome).
- A personal history of retinoblastoma.
Risk factors for melanoma in all age groups include:
- Having a fair complexion, which includes the following:
- Fair skin that freckles and burns easily, does not tan, or tans poorly.
- Blue or green or other light-colored eyes.
- Red or blond hair.
- Being exposed to natural sunlight or artificial sunlight (such as from tanning beds) over long periods of time.
- Having a history of many blistering sunburns as a child.
- Having several large or many small moles.
- Having a family history or personal history of unusual moles (atypical nevus syndrome).
- Having a family or personal history of melanoma.
Symptoms of melanoma include the following:
- A mole that:
- changes in size, shape, or color.
- has irregular edges or borders.
- is more than one color.
- is asymmetrical (if the mole is divided in half, the 2 halves are different in size or shape).
- itches.
- oozes, bleeds, or is ulcerated (a hole forms in the skin when the top layer of cells breaks down and the tissue below shows through).
- Change in pigmented (colored) skin.
- Satellite moles (new moles that grow near an existing mole).
Tests to diagnose and stage melanoma may include the following:
See the General Information section for a description of these tests and procedures.
Other tests and procedures used to diagnose melanoma include the following:
- Skin exam: A doctor or nurse checks the skin for bumps or spots that look abnormal in color, size, shape, or texture.
- Biopsy: All or part of the abnormal-looking growth is cut from the skin and viewed under a microscope by a pathologist to see if cancer cells are present. There are 4 main types of skin biopsies:
- Shave biopsy: A sterile razor blade is used to “shave-off” the abnormal-looking growth.
- Punch biopsy: A special instrument called a punch or a trephine is used to remove a circle of tissue from the abnormal-looking growth.
- Excisional biopsy: A scalpel is used to remove the entire growth.
- Wide local excision: A scalpel is used to remove some of the normal tissue around the area where melanoma was found, to check for cancer cells. Skin grafting may be needed to cover the area where tissue was removed.
- Sentinel lymph node biopsy: The removal of the sentinel lymph node during surgery. The sentinel lymph node is the first lymph node to receive lymphatic drainage from a tumor. It is the first lymph node the cancer is likely to spread to from the tumor. A radioactive substance and/or blue dye is injected near the tumor. The substance or dye flows through the lymph ducts to the lymph nodes. The first lymph node to receive the substance or dye is removed. A pathologist views the tissue under a microscope to look for cancer cells. If cancer cells are not found, it may not be necessary to remove more lymph nodes.
- Lymph node dissection: A surgical procedure in which lymph nodes are removed and a sample of tissue is checked under a microscope for signs of cancer. For a regional lymph node dissection, some of the lymph nodes in the tumor area are removed. For a radical lymph node dissection, most or all of the lymph nodes in the tumor area are removed. This procedure is also called a lymphadenectomy.
- FISH (fluorescence in situ hybridization): A laboratory test used to look at genes or chromosomes in cells and tissues. Pieces of DNA that contain a fluorescent dye are made in the laboratory and added to cells or tissues on a glass slide. When these pieces of DNA attach to certain genes or areas of chromosomes on the slide, they light up when viewed under a microscope with a special light. This test is done to tell the difference between melanoma and melanocytic tumors of unknown metastatic potential (MELTUMP).
- Cytogenetic analysis: A laboratory test in which cells in a sample of tissue are viewed under a microscope to look for certain changes in the chromosomes.
Treatment of Melanoma
Treatment for melanoma is surgery to remove the tumor and some tissue around the tumor. If cancer has spread to nearby lymph nodes, treatment is surgery to remove the lymph nodes with cancer. Biologic therapy with high-dose interferon alpha-2b may also be given.
Treatment for melanoma that has spread beyond the lymph nodes may include the following:
- Chemotherapy and/or biologic therapy.
- A clinical trial of high-dose biologic therapy or targeted therapy.
See the PDQ summary on adult Melanoma Treatment for more information.
Squamous Cell and Basal Cell Skin Cancer
The risk of squamous cell or basal cell cancer is increased by the following:
- Being exposed to natural sunlight or artificial sunlight (such as from tanning beds) over long periods of time.
- Having a fair complexion, which includes the following:
- Fair skin that freckles and burns easily, does not tan, or tans poorly.
- Blue or green or other light-colored eyes.
- Red or blond hair.
- Having actinic keratosis.
- Past treatment with radiation.
- Having a weakened immune system.
Symptoms of squamous cell and basal cell skin cancer include the following:
- A sore that does not heal.
- Areas of the skin that are:
- Small, raised, smooth, shiny, and waxy.
- Small, raised, and red or reddish-brown.
- Flat, rough, red or brown, and scaly.
- Scaly, bleeding, or crusty.
- Similar to a scar and firm.
Tests to diagnose squamous cell and basal cell skin cancer include the following:
- Skin exam: A doctor or nurse checks the skin for bumps or spots that look abnormal in color, size, shape, or texture.
- Biopsy: All or part of a growth that doesn't look normal is cut from the skin and viewed under a microscope by a pathologist to check for signs of cancer. There are three main types of skin biopsies:
- Shave biopsy: A sterile razor blade is used to “shave-off” the growth that does not look normal.
- Punch biopsy: A special instrument called a punch or a trephine is used to remove a circle of tissue from the growth that does not look normal.
- Excisional biopsy: A scalpel is used to remove the entire growth.
Treatment of Squamous Cell and Basal Cell Skin Cancer
Treatment for squamous cell and basal cell cancer is usually surgery to remove the tumor.
See the PDQ summary on adult Skin Cancer Treatment for more information.
ChordomaChordoma is a very rare type of bone tumor that forms anywhere along the spine from the base of the skull to the tailbone. In children and teenagers, chordomas develop more often in the base of the skull, making them hard to remove completely with surgery.
Childhood chordoma is linked to the condition tuberous sclerosis, a genetic disorder in which tumors that are benign (not cancer) form in the kidneys, brain, eyes, heart, lungs, and skin.
Symptoms
Chordoma may cause any of the following signs and symptoms. Check with your doctor if any of the following problems occur:
- Headache.
- Neck or back pain.
- Double vision.
- Paralysis of the muscles in the face.
- Numbness, tingling, or weakness of the arms and legs.
- A change in bowel or bladder habits.
Other conditions that are not chordoma may cause these same symptoms.
Chordomas may recur (come back), usually in the same place, but sometimes they recur in other areas of bone or in the lungs.
Treatment
Treatment for chordoma in children is usually surgery to remove as much of the tumor as possible, followed by radiation therapy. Proton beam radiation therapy may be used.
Cancer of Unknown Primary SiteCarcinoma of unknown primary is a rare disease in which malignant (cancer) cells are found in the body but the place the cancer began is not known. Cancer can form in any tissue of the body. The primary cancer (the cancer that first formed) can spread to other parts of the body. This process is called metastasis. Cancer cells usually look like the cells in the type of tissue in which the cancer began. For example, breast cancer cells may spread to the lung. Because the cancer began in the breast, the cancer cells in the lung look like breast cancer cells.
Sometimes doctors find where the cancer has spread but cannot find where in the body the cancer first began to grow. This type of cancer is called a cancer of unknown primary or occult primary tumor.
Tests are done to find where the primary cancer began and to get information about where the cancer has spread. When tests are able to find the primary cancer, the cancer is no longer a cancer of unknown primary and treatment is based on the type of primary cancer.
Because the place where the cancer started is not known, many different tests and procedures may be needed to find out what type of cancer it is. If tests show there may be cancer, a biopsy is done. A biopsy is the removal of cells or tissues so they can be viewed under a microscope by a pathologist. The pathologist views the tissue under a microscope to look for cancer cells and to find out the type of cancer. The type of biopsy that is done depends on the part of the body being tested for cancer. One of the following types of biopsies may be used:
- Excisional biopsy: The removal of an entire lump of tissue.
- Incisional biopsy: The removal of part of a lump or a sample of tissue.
- Core biopsy: The removal of tissue using a wide needle.
- Fine-needle aspiration (FNA) biopsy: The removal tissue or fluid using a thin needle.
When the type of cancer cells or tissue removed is different from the type of cancer cells expected to be found, a diagnosis of cancer of unknown primary may be made. The cells in the body have a certain look that depends on the type of tissue they come from. For example, a sample of cancer tissue taken from the breast is expected to be made up of breast cells. However, if the sample of tissue is a different type of cell (not made up of breast cells), it is likely that the cells have spread to the breast from another part of the body.
Adenocarcinomas, melanomas, and embryonal tumors are common tumor types that appear and it is not known where the cancer first formed. Embryonal tumors such as rhabdomyosarcomas and neuroblastomas are most common in children.
Treatment
Treatment depends on what the cancer cells look like under a microscope, the patient's age and symptoms, and where the cancer has spread in the body. Treatment is usually chemotherapy or radiation therapy.


 Back to Top
Back to Top