Chapter 7International Travel with Infants & Children
Vaccine Recommendations for Infants & Children
Vaccinating children for travel requires careful evaluation. Whenever possible, children should complete the routine immunizations of childhood on a normal schedule. However, travel at an earlier age may require accelerated schedules. Not all travel-related vaccines are effective in infants, and some are specifically contraindicated.
The recommended childhood and adolescent immunization schedules are depicted in Tables 7-02 and 7-03. Table 7-04 depicts the catch-up schedule for children and adolescents who start their vaccination schedule late or who are >1 month behind. This table also describes the recommended minimum intervals between doses for children who need to be vaccinated on an accelerated schedule, which may be necessary before international travel. Proof of yellow fever vaccination is required for entry into certain countries.
MODIFYING THE IMMUNIZATION SCHEDULE FOR INADEQUATELY IMMUNIZED INFANTS AND YOUNGER CHILDREN BEFORE INTERNATIONAL TRAVEL
Several factors influence recommendations for the age at which a vaccine is administered, including age-specific risks of the disease and its complications, the ability of people of a given age to develop an adequate immune response to the vaccine, and potential interference with the immune response by passively transferred maternal antibody.
The routine immunization recommendations and schedules for infants and children in the United States do not provide specific guidelines for those traveling internationally before the age when specific vaccines and toxoids are routinely recommended. Recommended age limitations are based on potential adverse events (yellow fever), lack of efficacy data or inadequate immune response (polysaccharide vaccines and influenza), maternal antibody interference (measles, mumps, rubella), or lack of safety data. In deciding when to travel with a young infant or child, parents should be advised that the earliest opportunity to receive routinely recommended immunizations in the United States (except for the dose of hepatitis B vaccine at birth) is at age 6 weeks.
Routine Infant and Childhood Vaccinations
Hepatitis B Vaccine
Hepatitis B virus (HBV) is a cause of acute and chronic hepatitis, cirrhosis, and hepatocellular carcinoma. There are more than 350 million chronically infected people worldwide. The risk of chronic infection is highest when infection occurs in infancy or childhood and declines with age. Infants and children who have not previously been vaccinated and who are traveling to areas where HBV is intermediately or highly endemic are at risk if they are directly exposed to blood (or body fluids containing blood) from the local population. HBV transmission could occur in children if they receive blood transfusions not screened for HBV surface antigen (HBsAg), are exposed to unsterilized medical or dental equipment, or have continuous close contact with local residents who have open skin lesions (impetigo, scabies, or scratched insect bites).
Hepatitis B vaccine is recommended for all infants in the United States, with the first dose administered soon after birth and before hospital discharge. Infants and children who will travel should receive 3 doses of HBV vaccine before traveling:
- The interval between doses 1 and 2 should be ≥4 weeks.
- The interval between doses 2 and 3 should be ≥8 weeks.
- The interval between doses 1 and 3 should be ≥16 weeks.
- The third dose should not be given before the infant is at least 24 weeks of age.
Adolescents not previously vaccinated with hepatitis B vaccine should be vaccinated at age 11–12 years:
- For adolescents, the usual schedule is 2 doses separated by ≥4 weeks, followed by a third dose 4–6 months after the second dose.
- A 2-dose series is licensed for adolescents aged 11–15 years, and doses can be separated by 4–6 months.
Diphtheria and Tetanus Toxoid and Pertussis Vaccine
Diphtheria, tetanus, and pertussis each occur worldwide and are endemic in countries with low immunization levels. Infants and children leaving the United States should be immunized before traveling. Optimum protection against diphtheria, tetanus, and pertussis is achieved with at least 3 but preferably 4 doses of diphtheria and tetanus toxoids and acellular pertussis vaccine (DTaP). Two doses of DTaP received at intervals ≥4 weeks apart can provide some protection; however, a single dose offers little protective benefit. Parents should be informed that infants and children who have not received ≥3 doses of DTaP might not be fully protected against pertussis.
The usual primary series includes 4 doses given at ages 2, 4, 6, and 15–18 months. A fifth (booster) dose is recommended when the child is aged 4–6 years. The fifth dose is not necessary, if the fourth dose in the primary series was given after the child’s fourth birthday.
The schedule can be accelerated as soon as the infant is 6 weeks of age, with the second and third doses given 4 weeks after each preceding dose. The fourth dose should not be given before the infant is 12 months of age and should be separated from the third dose by ≥6 months. The fifth (booster) dose should not be given before the child is 4 years of age.
Haemophilus influenzae Type b Conjugate Vaccine
Haemophilus influenzae type b (Hib) is an endemic disease worldwide that can cause fatal meningitis, epiglottitis, and other invasive diseases. Infants and children should have optimal protection before traveling. Routine Hib vaccination beginning at age 2 months is recommended for all US children. The first dose may be given when an infant is as young as 6 weeks of age. Children aged <6 weeks should not be given Hib vaccine, because it may induce immune tolerance to subsequent vaccines.
A primary series consists of 2 or 3 doses (depending on the type of vaccine used) with a minimum interval of 4 weeks between doses. A booster dose is recommended when the infant is aged ≥12 months and at least 8 weeks have passed since the previous dose. If Hib vaccination is started when the infant or child is aged ≥7 months, fewer doses are required.
A shortage of Hib vaccine supply in the United States in 2008 and 2009 may have resulted in deferral of the booster dose at 12–15 months. Clinicians need to review a child’s earlier vaccination history with Hib and update if indicated.
Considerations for travel by age include the following:
- If previously unvaccinated, infants aged <15 months should receive at least 2 vaccine doses before travel. An interval as short as 4 weeks between these 2–3 doses is acceptable.
- Unvaccinated infants and children aged 15–59 months should receive a single dose of Hib vaccine.
- Children aged >59 months, adolescents, and adults do not need to be vaccinated unless a specific condition exists, such as functional or anatomic asplenia, immunodeficiency, immunosuppression, or HIV infection.
If different brands of vaccine are administered, a total of 3 doses of Hib conjugate vaccine completes the primary series. After completion of the primary infant vaccination series, any of the licensed Hib conjugate vaccines may be used for the booster dose when the infant is aged 12–15 months.
Polio Vaccine
Although polio has been eliminated in the United States, poliovirus continues to circulate in other parts of the world. In the United States, all infants and children should receive 4 doses of inactivated poliovirus vaccine (IPV) at ages 2, 4, 6–18 months, and 4–6 years. If accelerated protection is needed, the minimum interval between doses is 4 weeks. The minimum age for the fourth dose is 4 years. If a child has received 4 doses of poliovirus vaccine before the fourth birthday, a fifth dose is recommended. The interval between the next-to-last and last dose should be ≥6 months. Infants and children who had initiated the poliovirus vaccination series with 1 or more doses of oral poliovirus vaccine (OPV) should receive IPV to complete the series.
Rotavirus Vaccine
Rotavirus is the most common cause of severe gastroenteritis in infants and young children worldwide. In developing countries, rotavirus gastroenteritis is responsible for approximately 500,000 deaths per year among children aged <5 years. Routine rotavirus vaccination beginning at age 2 months is recommended for all US infants.
Two rotavirus vaccines, RotaTeq (RV5) and Rotarix (RV1), are licensed for use in US infants. RV5 is administered orally in a 3-dose series at ages 2, 4, and 6 months. RV1 is administered orally in a 2-dose series at ages 2 and 4 months. The minimum age for the first dose of rotavirus vaccine is 6 weeks; the maximum age for the first dose is 14 weeks, 6 days. Vaccination should not be initiated for infants aged 15 weeks, 0 days or older because of insufficient data on the safety of the first dose of rotavirus vaccine in older infants. The minimum interval between doses of rotavirus vaccine is 4 weeks. All doses should be administered before age 8 months, 0 days.
Measles, Mumps, and Rubella Vaccine (MMR)
Measles is an endemic disease in many countries, and outbreaks occur even in developed countries. International travelers are at increased risk for measles exposure. Infants and children should be protected against measles, and the immunization series should be completed before traveling, if possible. While the risk for serious disease from either mumps or rubella is low, these diseases circulate in many parts of the world, and vaccination is recommended.
The Advisory Committee for Immunization Practices (ACIP) generally recommends combination vaccines over single-component vaccines. ACIP recommends that MMR vaccine be administered when any of the individual components is indicated as part of the routine immunization schedule. However, the risk of seizures after vaccination is increased if MMRV is used for the first dose in the series between the ages of 12 and 47 months. So for this dose, MMR and varicella administered separately are preferred over MMRV. The combination product MMRV is generally recommended for the second dose of the series, or for the first dose if it is given to someone aged 47 months through 12 years. Monovalent measles, monovalent mumps, monovalent rubella, and combination measles-rubella vaccines are not currently available in the United States. MMRV vaccine is licensed for children aged 12 months to 12 years and may be used in place of MMR vaccine, if vaccination for measles, mumps, rubella, and varicella is needed.
Two doses of MMR are routinely recommended for all children, usually at age 12 months and again at age 4–6 years. The second dose of MMR can be given as soon as 28 days after the first dose.
Children traveling abroad should be vaccinated at an earlier age than children remaining in the United States. Before departure, children aged 6–11 months should receive the first dose of MMR vaccine, and children aged ≥12 months should have received 2 doses of MMR vaccine before departure. Infants vaccinated before age 12 months must be revaccinated on or after their first birthday with 2 doses of MMR vaccine, separated by at least 28 days.
Varicella Vaccine
Varicella (chickenpox) is an endemic disease throughout the world. Two doses of varicella vaccine are recommended for all susceptible children and adolescents. The first dose is recommended at age 12–15 months. The second dose is routinely recommended at age 4–6 years but can be given earlier, provided that ≥3 months have passed since the first dose.
Efforts should be made to ensure varicella immunity before age 13 years, because varicella disease can be more severe among older children and adults. Children aged ≥13 should receive 2 doses of varicella vaccine 4–8 weeks apart.
Vaccination is not necessary for children with a history of documented chickenpox. When a prior history of chickenpox is uncertain, the vaccine should be given.
Meningococcal Vaccine
Meningococcal disease, caused by the bacterium Neisseria meningitidis, is associated with high morbidity and mortality. Epidemics occur in sub-Saharan Africa during the dry season, December through June (see Map 3-13), and CDC recommends that travelers be vaccinated before traveling to this region. Meningococcal vaccination is a requirement to enter Saudi Arabia when traveling to Mecca during the annual Hajj. Health requirements and recommendations for US travelers planning to travel to Saudi Arabia for Hajj are available on the CDC Travelers’ Health website after these recommendations are determined each fall (www.cdc.gov/travel).
Three vaccines are available in the United States that protect against 4 serogroups of N. meningitidis (A, C, Y, and W-135): 2 meningococcal conjugate vaccines (MenACWY) and 1 meningococcal polysaccharide vaccine (MPSV4). The 2 conjugate vaccines are differentiated by their protein conjugate. A one-dose primary series of MenACWY-D (Menactra) is licensed for people aged 2–55 years; a two-dose primary series of MenACWY-D is licensed for children aged 9–23 months. MenACWY-Crm (Menveo) is licensed for people aged 2–55 years.
CDC recommends routine vaccination of people with MenACWY at age 11 or 12 years, with a booster dose at age 16 years. For adolescents who receive the first dose at age 13–15 years, a one-time booster dose should be administered, preferably at age 16–18 years. People who receive their first dose of MenACWY at or after age 16 years do not need a booster dose, unless they remain at continued risk for meningococcal disease.
Meningococcal vaccine is also recommended for people aged 9 months through 10 years and ≥19 years who travel to or reside in areas where N. meningitidis is hyperendemic or epidemic. A conjugate product is preferred where licensed for a person’s age group, and providers should take care to use a meningococcal vaccine that is licensed for a particular age. MPSV4 (licensed for people aged ≥2 years) can be used when neither MenACWY vaccine is available.
Age considerations:
- The serogroup A polysaccharide in MPSV4 induces an antibody response in some children as young as 3 months. Thus, vaccinating infants traveling to high-risk areas can provide some degree of protection.
- For children vaccinated with either MPSV4 or MenACWY at age <7 years, revaccination with MenACWY in 3 years is recommended, if the children remain at high risk for infection, and every 5 years thereafter, if they remain at continued risk.
- For children vaccinated with either MPSV4 or MenACWY at age ≥7 years, revaccination with MenACWY is recommended in 5 years, if they remain at high risk, and every 5 years thereafter, if they remain at continued risk.
(Updated January 25, 2012)
Pneumococcal Vaccines
Streptococcus pneumoniae is a leading cause of illness and death worldwide. In the United States, 2 vaccines are available to prevent pneumococcal disease: the 13-valent pneumococcal conjugate vaccine (PCV13) is recommended for routine use in children aged ≤5 years, and the pneumococcal polysaccharide vaccine (PPSV23) is recommended for children and adults aged ≥2 years who have certain underlying medical conditions, and for all adults aged ≥65 years. Before March 2010, the 7-valent vaccine (PCV7) was used. Licensure of PCV13 with its improved serotype protection has prompted its use in place of PCV7 on the same schedule.
All infants should be vaccinated with PCV13. Infant vaccination provides the earliest protection, and children aged <2 years have high rates of pneumococcal disease. The primary series for PCV13 includes 3 doses given at ages 2, 4, and 6 months, with a fourth (booster) dose at age 12–15 months. Children who have been completely vaccinated with PCV7 should receive a single dose of PCV13 between the ages of 14 and 59 months to afford extra seroprotection to the additional components of the new vaccine. For children at risk of invasive S. pneumoniae disease, this supplemental dose is recommended through age 71 months. PCV13 should be given ≥8 weeks after the last dose of PCV7 or PPSV23.
Children aged ≥2 years who are at high risk for pneumococcal disease (such as those with sickle cell disease, asplenia, HIV, chronic illness, or immunocompromising conditions) should receive a dose of PPSV23 ≥2 months after their last dose of PCV7 or PCV13. A second dose of PPSV23 is recommended 5 years after the first dose of PPSV23 for people aged ≥2 years who are immunocompromised, have sickle cell disease, or have functional or anatomic asplenia.
All healthy children aged 24–59 months who have not completed any recommended schedule for PCV7 should receive 1 dose of PCV13. All children with underlying medical conditions through age 71 months who have received 3 doses should receive 1 dose of PCV13. This includes those who have previously received PPSV23. All children with underlying medical conditions aged 24–59 months who have received <3 doses and have not received any doses after age 12 months should receive 2 doses of PCV13 at least 8 weeks apart. The PCV13 vaccine is not routinely recommended for people aged >5 years, but providers are permitted to give a dose to children aged 6–18 years if they are at high risk of invasive S. pneumoniae disease.
Influenza Vaccine
Influenza viruses circulate predominantly in the winter months in temperate regions (typically November–April in the Northern Hemisphere and April–September in the Southern Hemisphere) but can occur year-round in tropical climates. Annual influenza vaccination of all people aged ≥6 months is recommended by ACIP as the most effective measure for preventing influenza and its associated complications. Prevention of influenza is particularly important for people who are (or live with those who are) at increased risk for influenza-related complications, such as children aged <5 years (particularly infants aged <6 months who are not eligible for influenza vaccination), people with medical conditions (such as immunosuppression, diabetes, asthma, pregnancy, and neurologic disorders) and children and adolescents who are receiving long-term aspirin therapy.
Two types of influenza vaccines are available for use in the United States: trivalent inactivated vaccine (TIV), administered by intramuscular injection; and live, attenuated influenza vaccine (LAIV), administered by nasal spray. LAIV is approved for use only in healthy people aged 2–49 years who are not pregnant. LAIV may result in an increase in asthma or reactive airway disease in children aged <5 years; therefore, LAIV should not be administered to children aged <2 years or to children aged 2–4 years who have a history of wheezing in the past year or who had a diagnosis of asthma.
Children receiving TIV should be administered an age-appropriate dose (0.25 mL for those aged 6–35 months and 0.5 mL for those aged ≥36 months). One dose of influenza vaccine per season is recommended for most people. Children aged <9 years who are receiving influenza vaccine for the first time or who received only 1 dose the previous season (if it was their first vaccination season) should receive 2 doses (separated by a 4-week interval). Only 1 dose per year is needed in previously unvaccinated children aged ≥9 years. More specific information about these influenza vaccine recommendations can be found on the CDC website (www.cdc.gov/flu).
Hepatitis A Vaccine or Immune Globulin for Hepatitis A
Hepatitis A virus (HAV) is endemic in most parts of the world, and infants and children traveling to these areas are at increased risk for acquiring HAV infection. Although HAV is often not severe in infants and children aged <5 years, infected children may transmit the infection to older children and adults, who are at higher risk for severe disease.
Hepatitis A vaccine
Hepatitis A vaccine is a routine immunization of childhood in the United States. It is recommended for all children at age 1 year (12–23 months). Vaccination should be ensured for all susceptible children traveling to areas where there is an intermediate or high risk of HAV infection. The hepatitis A vaccine is not approved for children aged <1 year. The HAV vaccine series consists of 2 doses ≥6 months apart. One dose of monovalent hepatitis A vaccine administered at any time before departure can provide adequate protection for most healthy children. The second dose is necessary for long-term protection.
Immune globulin
Children aged <1 year who are traveling to high-risk areas can receive immune globulin (IG). For optimal protection, children aged ≥1 year who are immunocompromised or have chronic medical conditions and who are planning to depart to a high-risk area in <2 weeks should receive the initial dose of vaccine, along with IG (0.02 mL/kg intramuscularly) at a separate anatomic injection site.
IG does not interfere with the response to yellow fever vaccine but can interfere with the response to other live injected vaccines (such as MMR and varicella vaccines). Administration of MMR should be delayed for ≥3 months and varicella for >5 months after administration of IG. IG should not be administered for 2 weeks after measles-, mumps-, rubella-, and varicella-containing vaccines. If IG is given during this time, the child should be revaccinated with the live vaccine ≥3 months after administration of IG. When travel plans do not allow adequate time to administer live vaccines and IG before travel, the severity of the diseases and their epidemiology at the destination will help determine the most appropriate course of preparation.
Human Papillomavirus Vaccine
Human papillomavirus (HPV) infection can be prevented with 2 licensed vaccines. One vaccine, HPV4, protects against HPV types 6, 11, 16, and 18; the other, HPV2, protects against types 16 and 18. Both protect against cervical cancer, and HPV4 also protects against genital warts. HPV vaccination is recommended for girls aged 11–12 years with catch-up vaccination recommended through 26 years. HPV2 is licensed for girls/women aged 10–25 years and HPV4 is licensed for girls and women aged 9-26 years. HPV4 is also licensed for use in boys and men aged 9–26 years. The schedule for both vaccines is 3 doses at 0, 1–2, and 6 months. The minimum interval between dose 1 and dose 2 is 4 weeks. Dose 3 should be given ≥12 weeks after dose 2.
Other Vaccines
Yellow Fever Vaccine
Yellow fever, a disease transmitted by mosquitoes, is endemic in certain areas of Africa and South America (see Maps 3-18 and 3-19). Proof of yellow fever vaccination is required for entry into some countries (see Chapter 3, Yellow Fever and Malaria Information, by Country). Infants and children aged ≥9 months can be vaccinated if they travel to countries within the yellow fever-endemic zone.
Infants are at high risk for developing encephalitis from yellow fever vaccine, a live virus vaccine. Vaccination of infants should be considered on an individual basis. Although the incidence of these adverse events has not been clearly defined, 14 of 18 reported cases of postvaccination encephalitis were in infants aged <4 months. One fatal case confirmed by viral isolation was in a 3-year-old child.
Travelers with infants <9 months of age should be advised against traveling to areas within the yellow fever-endemic zone. ACIP recommends that yellow fever vaccine never be given to infants aged <6 months. Infants ages 6–8 months should be vaccinated only if they must travel to areas of ongoing epidemic yellow fever and if a high level of protection against mosquito bites is not possible (see Chapter 3, Yellow Fever). Physicians considering vaccinating infants 6–8 months of age may contact their respective state health departments or CDC at 800-232-4636.
Typhoid Vaccine
Typhoid fever is caused by the bacterium Salmonella enterica serotype Typhi. Vaccination is recommended for travelers to areas where there is a recognized risk of exposure to S. Typhi.
Two typhoid vaccines are available: a Vi capsular polysaccharide vaccine (ViCPS) administered intramuscularly and an oral, live, attenuated vaccine (Ty21a). Both vaccines induce a protective response in 50%–80% of recipients. The ViCPS vaccine can be administered to children who are aged ≥2 years, with a booster dose 2 years later, if continued protection is needed. The Ty21a vaccine, which consists of a series of 4 capsules (1 taken every other day) can be administered to children aged ≥6 years. A booster series for Ty21a should be taken every 5 years, if indicated. The capsule cannot be opened for administration but must be swallowed whole. All 4 doses should be taken ≥1 week before potential exposure.
Japanese Encephalitis Vaccine
Japanese encephalitis (JE) virus is transmitted by mosquitoes and is endemic throughout Asia. The risk can be seasonal in temperate climates and year-round in more tropical climates. The risk to short-term travelers and those who confine their travel to urban centers is low. Travelers who plan to travel for ≥1 month or take up residence in an endemic area should be vaccinated against JE. The decision to vaccinate a child should follow the more detailed recommendations in Chapter 3, Japanese Encephalitis.
JE-Vax, an inactivated mouse brain–derived vaccine, was licensed in the United States in 1992 for use in travelers aged ≥1 year. However, JE-Vax is no longer manufactured and all remaining doses expired in May 2011. A new, inactivated Vero cell culture-derived JE vaccine (trade name Ixiaro) was licensed by the Food and Drug Administration on March 30, 2009, for use in the United States for travelers aged ≥17 years. Ixiaro is not approved for use in children aged <17 years of age. Pediatric clinical trials are being conducted to enable licensure of Ixiaro for use in children. However, it will likely be several years before Ixiaro is licensed in the United States for use in children. For information about current options for obtaining JE vaccine for US children, see Update on Japanese Encephalitis (JE) Vaccine for US Children.
(Updated September 1, 2011)
Rabies Vaccine
Rabies virus causes an acute viral encephalitis that is virtually 100% fatal. Traveling children may be at increased risk of rabies exposure, mainly from street dogs in developing countries. Bat bites carry a potential risk of rabies throughout the world. There are 2 strategies to prevent rabies in humans:
- Avoiding bite or scratch exposures.
- A 3-shot preexposure immunization series, on days 0, 7, and 21 or 28. In the event of a subsequent possible rabies virus exposure, the child will require 2 more doses of rabies vaccine on days 0 and 3. The decision whether to obtain preexposure immunization for children should follow the recommendations in Chapter 3, Rabies.
For children who have not received preexposure immunization and may have been exposed to rabies, a weight-based dose of human rabies immune globulin and a series of 4 rabies vaccine injections are required on days 0, 3, 7, and 14.
Table 7-02. Recommended immunization schedule for ages 0–6 years—United States, 2011
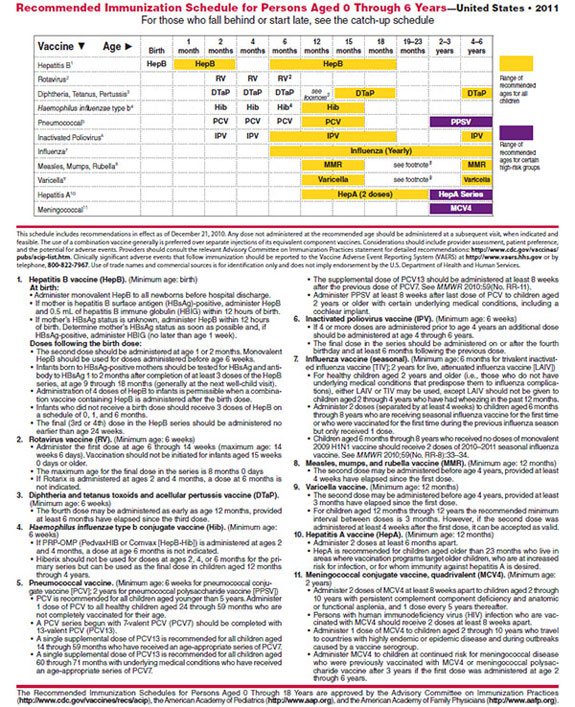 |
For a printable version of this chart, please see the CDC Vaccines site..
Table 7-03. Recommended immunization schedule for ages 7–18 years—United States, 2011
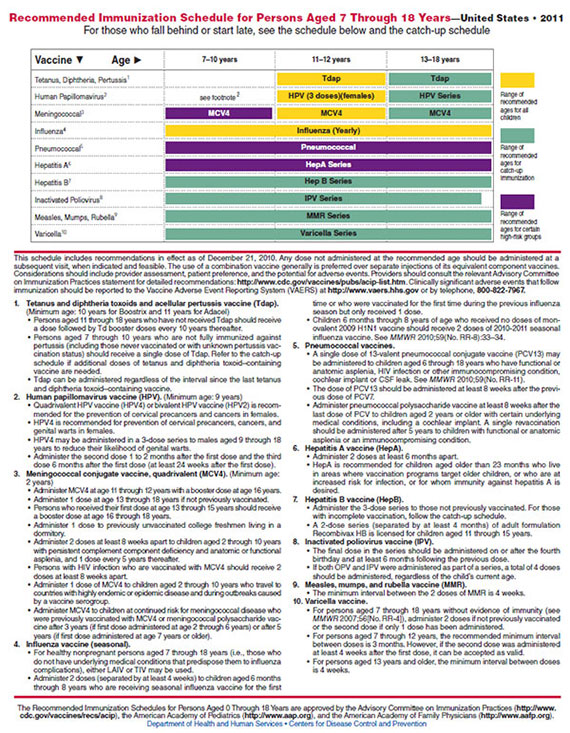 |
For a printable version of this chart, please see the CDC Vaccines site.
Table 7-04. Recommended childhood catch-up immunization schedule—United States, 2011. Children and adolescents who start late or who are more than 1 month behind.
The table below provides catch-up schedules and minimum intervals between doses for children whose vaccinations have been delayed. A vaccine series does not need to be restarted, regardless of the time that has elapsed between doses. Use the section appropriate for the child’s age.
| VACCINE | MINIMUM AGE FOR DOSE 1 | MINIMUM INTERVAL BETWEEN DOSES | |||
|---|---|---|---|---|---|
| DOSE 1 TO DOSE 2 | DOSE 2 TO DOSE 3 | DOSE 3 TO DOSE 4 | DOSE 4 TO DOSE 5 | ||
| Persons Aged 4 Months Through 6 Years | |||||
| Hepatitis B1 | Birth | 4 weeks | 8 weeks (and at least 16 weeks after first does) |
||
| Rotavirus2 | 6 weeks | 4 weeks | 4 weeks2 | ||
| Diphtheria, Tetanus, Pertussis3 | 6 weeks | 4 weeks | 4 weeks | 6 months | 6 months3 |
| Haemophilus influenzae type b4 | 6 weeks | 4 weeks if first dose administered at younger than age 12 months 8 weeks (as final dose) if first dose administered at age 12–14 months No further doses needed if first dose administered at age 15 months or older |
4 weeks4 if current age is younger than 12 months 8 weeks (as final dose)4 if current age is 12 months or older and first dose administered at younger than age 12 months and second dose administered at younger than 15 months No further doses needed if previous dose administered at age 15 months or older |
8 weeks (as final dose) This dose only necessary for children aged 12 months through 59 months who received 3 doses before age 12 months |
|
| Pneumo- coccal5 |
6 weeks | 4 weeks if first dose administered at younger than age 12 months 8 weeks (as final dose for healthy children) if first dose administered at age 12 months or older or current age 24 through 59 months No further doses needed for healthy children if first dose administered at age 24 months or older |
4 weeks if current age is younger than 12 months 8 weeks (as final dose for healthy children) if current age is 12 months or older No further doses needed for healthy children if previous dose administered at age 24 months or older |
8 weeks (as final dose) This dose only necessary for children aged 12 months through 59 months who received 3 doses before age 12 months or for children at high risk who received 3 doses at any age |
|
| Inactivated Poliovirus6 | 6 weeks | 4 weeks | 4 weeks | 6 months6 | |
| Measles, Mumps, Rubella7 | 12 months | 4 weeks | |||
| Varicella8 | 12 months | 3 months | |||
| Hepatitis A9 | 12 months | 6 months | |||
| Persons Aged 7 Through 18 Years | |||||
| Tetanus, Diphtheria/ Tetanus, Diphtheria, Pertussis10 | 7 years10 | 4 weeks | 4 weeks if first dose administered at younger than age 12 months 6 months if first dose administered at 12 months or older |
6 months if first dose administered at younger than age 12 months |
|
| Human Papilloma- virus11 |
9 years | Routine dosing intervals are recommended (females)11 | |||
| Hepatitis A9 | 12 months | 6 months | |||
| Hepatitis B1 | Birth | 4 weeks | 8 weeks (and at least 16 weeks after first dose) |
||
| Inactivated Poliovirus6 | 6 weeks | 4 weeks | 4 weeks6 | 6 months6 | |
| Measles, Mumps, Rubella7 | 12 months | 4 weeks | |||
| Varicella8 | 12 months | 3 months if person is younger than age 13 years 4 weeks if person is aged 13 years or older |
|||
- Administer the 3-dose series to those not previously vaccinated.
- The minimum age for the third dose of HepB is 24 weeks.
- A 2-dose series (separated by at least 4 months) of adult formulation Recombivax HB is licensed for children aged 11 through 15 years.
- The maximum age for the first dose is 14 weeks, 6 days. Vaccination should not be initiated for infants aged 15 weeks, 0 days or older.
- The maximum age for the final dose in the series is 8 months, 0 days.
- If Rotarix was administered for the first and second doses, a third dose is not indicated.
- The fifth dose is not necessary if the fourth dose was administered at age 4 years or older.
- 1 dose of Hib vaccine should be considered for unvaccinated persons aged 5 years or older who have sickle cell disease, leukemia, or HIV infection, or who have had a splenectomy.
- If the first 2 doses were PRP-OMP (PedvaxHIB or Comvax), and administered at age 11 months or younger, the third (and final) dose should be administered at age 12 through 15 months and at least 8 weeks after the second dose.
- If the first dose was administered at age 7 through 11 months, administer the second dose at least 4 weeks later and a final dose at age 12 through 15 months.
- Administer 1 dose of 13-valent pneumococcal conjugate vaccine (PCV13) to all healthy children aged 24 through 59 months with any incomplete PCV schedule (PCV7 or PCV13).
- For children aged 24 through 71 months with underlying medical conditions, administer 1 dose of PCV13 if 3 doses of PCV were received previously or administer 2 doses of PCV13 at least 8 weeks apart if fewer than 3 doses of PCV were received previously.
- A single dose of PCV13 is recommended for certain children with underlying medical conditions through 18 years of age. See age-specific schedules for details.
- Administer pneumococcal polysaccharide vaccine (PPSV) to children aged 2 years or older with certain underlying medical conditions, including a cochlear implant, at least 8 weeks after the last dose of PCV. A single revaccination should be administered after 5 years to children with functional or anatomic asplenia or an immunocompromising condition. See MMWR 2010;59(No. RR-11).
- The final dose in the series should be administered on or after the fourth birthday and at least 6 months following the previous dose.
- A fourth dose is not necessary if the third dose was administered at age 4 years or older and at least 6 months following the previous dose.
- In the first 6 months of life, minimum age and minimum intervals are only recommended if the person is at risk for imminent exposure to circulating poliovirus (i.e., travel to a polioendemic region or during an outbreak).
- Administer the second dose routinely at age 4 through 6 years. The minimum interval between the 2 doses of MMR is 4 weeks.
- Administer the second dose routinely at age 4 through 6 years.
- If the second dose was administered at least 4 weeks after the fi rst dose, it can be accepted as valid.
- HepA is recommended for children aged older than age 23 months who live in areas where vaccination programs target older children, or who are at increased risk for infection, or for whom immunity against hepatitis A is desired.
- Doses of DTaP are counted as part of the Td/Tdap series.
- Tdap should be substituted for a single dose of Td in the catch-up series for children aged 7 through 10 years or as a booster for children aged 11 through 18 years; use Td for other doses.
- Administer the series to females at age 13 through 18 years if not previously vaccinated or have not completed the vaccine series.
- Quadrivalent HPV vaccine (HPV4) may be administered in a 3-dose series to males aged 9 through 18 years to reduce their likelihood of genital warts.
- Use recommended routine dosing intervals for series catch-up (i.e., the second and third doses should be administered at 1 to 2 and 6 months after the first dose). The minimum interval between the first and second doses is 4 weeks. The minimum interval between the second and third doses is 12 weeks, and the third dose should be administered at least 24 weeks after the first dose.
Information about reporting reactions after immunization is available online at www.vaers.hhs.gov or by telephone, 800-822-7967. Suspected cases of vaccine-preventable diseases should be reported to the state or local health department. Additional information, including precautions and contraindications for immunization, is available from the National Center for Immunization and Respiratory Diseases at www.cdc.gov/vaccines or telephone, 800-CDC-INFO (800-232-4636).
BIBLIOGRAPHY
- Broder KR, Cortese MM, Iskander JK, Kretsinger K, Slade BA, Brown KH, et al. Preventing tetanus, diphtheria, and pertussis among adolescents: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccines—recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2006 Mar 24;55(RR-3):1–34.
- CDC. Epidemiology and prevention of vaccine-preventable diseases. 9th ed. Atkinson W, Hamborsky J, McIntyre L, Wolfe S, editors. Washington, DC: Public Health Foundation; 2006.
- CDC. Licensure of a 13-valent pneumococcal conjugate vaccine (PCV13) and recommendations for use among children—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2010 Mar 12;59(9):258–61.
- CDC. Notice to readers: recommendation from the Advisory Committee on Immunization Practices (ACIP) for use of quadrivalent meningococcal conjugate vaccine (MCV4) in children aged 2–10 years at increased risk for invasive meningococcal disease. MMWR Morb Mortal Wkly Rep. 2007;56(48):1265–6.
- CDC. Recommendation of the Advisory Committee on Immunization Practices [ACIP] for use of quadrivalent meningococcal conjugate vaccine [MenACWY-D] among children aged 9 through 23 months at increased risk for invasive meningococcal disease. MMWR 2011: 60(40);1391–2.
- CDC. Revised recommendations of the Advisory Committee on Immunization Practices to vaccinate all persons aged 11–18 years with meningococcal conjugate vaccine. MMWR Morb Mortal Wkly Rep. 2007 Aug 10;56(31):794–5.
- CDC. Update: recommendations from the Advisory Committee on Immunization Practices (ACIP) regarding administration of combination MMRV vaccine. MMWR Morb Mortal Wkly Rep. 2008 Mar 14;57(10):258–60.
- CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011 Jan 28;60(3):72–6.
- CDC. Updated recommendations of the Advisory Committee on Immunization Practices (ACIP) regarding routine poliovirus vaccination. MMWR Morb Mortal Wkly Rep. 2009 Aug 7;58(30):829–30.
- Cetron MS, Marfin AA, Julian KG, Gubler DJ, Sharp DJ, Barwick RS, et al. Yellow fever vaccine. Recommendations of the Advisory Committee on Immunization Practices (ACIP), 2002. MMWR Recomm Rep. 2002 Nov 8;51(RR-17):1–11.
- Cortese MM, Parashar UD. Prevention of rotavirus gastroenteritis among infants and children: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2009 Feb 6;58(RR-2):1–25.
- Fiore AE, Shay DK, Broder K, Iskander JK, Uyeki TM, Mootrey G, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2009. MMWR Recomm Rep. 2009 Jul 31;58(RR-8):1–52.
- Fiore AE, Wasley A, Bell BP. Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2006 May 19;55(RR-7):1–23.
- Fischer M, Lindsey N, Staples JE, Hills S. Japanese encephalitis vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2010 Mar 12;59(RR-1):1–27.
- Mast EE, Margolis HS, Fiore AE, Brink EW, Goldstein ST, Wang SA, et al. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP) part 1: immunization of infants, children, and adolescents. MMWR Recomm Rep. 2005 Dec 23;54(RR-16):1–31.
- Rupprecht CE, Briggs D, Brown CM, Franka R, Katz SL, Kerr HD, et al. Use of a reduced (4-dose) vaccine schedule for postexposure prophylaxis to prevent human rabies: recommendations of the advisory committee on immunization practices. MMWR Recomm Rep. 2010 Mar 19;59(RR-2):1–9.
Contact Us:
-
Centers for Disease Control and Prevention
1600 Clifton Rd
Atlanta, GA 30333 -
800-CDC-INFO
(800-232-4636)
TTY: (888) 232-6348 -
New Hours of Operation
8am-8pm ET/Monday-Friday
Closed Holidays - cdcinfo@cdc.gov


