
2

2
Co-Lead Agencies: |
Centers for Disease Control and Prevention |
[Note: The National Library of Medicine has provided PubMed links to available references that appear at the end of this focus area document.]
Contents
Interim Progress Toward Year 2000 Objectives
Healthy People 2010—Summary of Objectives
Healthy People 2010 Objectives
 Arthritis and Other Rheumatic Conditions
Arthritis and Other Rheumatic Conditions
Related Objectives From Other Focus Areas
Prevent illness and disability related to arthritis and other rheumatic conditions, osteoporosis, and chronic back conditions.
The current and projected growth in the number of people aged 65 years and older in the United States has focused attention on preserving quality of life as well as length of life. Chief among the factors involving preserving quality of life are the prevention and treatment of musculoskeletal conditions—the major causes of disability in the United States. Among musculoskeletal conditions, arthritis and other rheumatic conditions, osteoporosis, and chronic back conditions have the greatest impact on public health and quality of life.
Demographic trends suggest that people will need to continue working at older ages (for example, beyond age 65 years), increasing the adverse social and economic consequences of the high rates of activity limitation and disability of older persons with these conditions. At the same time, effective public health interventions exist to reduce the burden of all three conditions. (See Focus Area 6. Disability and Secondary Conditions.)
The various forms of arthritis affect more than 15 percent of the U.S. population—over 43 million persons—and more than 20 percent of the adult population, making arthritis one of the most common conditions in the United States.[1], [2], [3], [4]
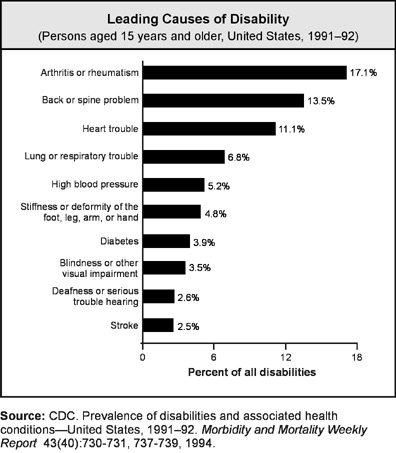
The significant public health impact of arthritis is reflected in a variety of measures. First, arthritis is the leading cause of disability.[5] Arthritis limits the major activities (for example, working, housekeeping, school) of nearly 3 percent of the entire U.S. population (7 million persons), including nearly 1 out of every 5 persons with arthritis.1, 2, 3 Arthritis trails only heart disease as a cause of work disability.[6] As a consequence, arthritis limits the independence of affected persons and disrupts the lives of family members and other caregivers.
Second, health-related quality-of-life measures are consistently worse for persons with arthritis, whether the measure is healthy days in the past 30 days, days without severe pain, “ability days” (that is, days without activity limitations), or difficulty in performing personal care activities.[7], [8]
Third, arthritis has a sizable economic impact. Arthritis is the source of at least 44 million visits to health care providers, 744,000 hospitalizations, and 4 million days of hospital care per year.4, [9] Estimated medical care costs for persons with arthritis were $15 billion, and total costs (medical care plus lost productivity) were $65 billion in 1992.[10] This latter amount is equal to 1.1 percent of the gross domestic product. Nearly 60 percent of persons with arthritis are in the working-aged population1, 2, 3 and they have a low rate of labor force participation.[11]
Fourth, arthritis, like other chronic pain conditions, has an important negative effect on a person’s mental health.[12], [13]
Fifth, although death is not a frequent outcome of arthritis, persons with certain forms of arthritis have higher death rates than the general population. For example, the 2 million persons in the United States with rheumatoid arthritis are at greater risk of premature death from respiratory and infectious diseases than the overall U.S. population.[14]
A variety of demographic trends indicate that the impact of arthritis will only increase.[15] Given current population projections, arthritis will affect over 18 percent of all persons in the United States (nearly 60 million persons) in the year 2020 and will limit the major activities of nearly 4 percent (11.6 million).1, 2, 3 Direct and indirect costs are expected to rise proportionately.
About 13 to 18 percent of women aged 50 years and older and 3 to 6 percent of men aged 50 years and older have osteoporosis, a reduction in bone mass or density that leads to deteriorated and fragile bones. These rates correspond to 4 million to 6 million women and 1 million to 2 million men in the United States who have osteoporosis.[16] Another 37 to 50 percent of women aged 50 years and older and 28 to 47 percent of men of the same age group have some degree of osteopenia, reduction in bone mass that is not as severe as osteoporosis.
The major health consequence of osteoporosis is an increased risk of fractures. Approximately 1.5 million fractures per year are attributed to osteoporosis.[17] One in three women and one in eight men aged 50 years and older will experience an osteoporotic-related fracture in their lifetime.17 Health care costs for these fractures are estimated at $13.8 billion per year in 1996 dollars.[18]
The risk of any fracture increases with the presence of osteoporosis, but hip fractures represent the most serious impact in terms of health care costs and consequences for the individual. In 1994, there were 281,000 hospital discharges for hip fracture among people aged 45 years and older. Of these, 74,000, or 26 percent, were among men.16 In all, 1 out of 6 white women and 1 out of 17 white men will experience a hip fracture by the time they reach age 90 years.[19] Although the hip fracture rate among women seems relatively constant, the rate among men seems to be increasing over time.[20]
An average of 24 percent of hip fracture patients aged 50 years and older die in the year following fracture, with higher death rates among men than among women.[21] Also, hip fracture is more likely to lead to functional impairment than are other serious medical conditions, including heart attack, stroke, and cancer.21 For example, half of all hip fracture patients will be unable to walk without assistance.17
Chronic low back pain is described in different ways, such as the occurrence of back pain lasting for more than 7 to 12 weeks, back pain lasting beyond the expected period of healing, or frequently recurring back pain. Moreover, a wide range of outcome measures are used to describe chronic back problems, such as low back pain (LBP), activity limitation, impairment, and disability. Compounding the problem is the lack of a single data source to track chronic back problems. Sources that have been used include workers compensation data, Occupational Safety and Health Administration and Bureau of Labor Statistics records, and data from national health surveys.
Chronic back conditions are both common and debilitating. Back pain occurs in 15 to 45 percent of people each year,[22], [23], [24], [25], [26] and 70 to 85 percent of people have back pain some time in their lives. In the United States, back pain is the most frequent cause of activity limitation in people under age 45 years,[27], [28] the second most frequent reason for physician visits, the fifth-ranking reason for hospitalization, and the third most common reason for surgical procedures.[29]
Work-related risk factors, such as heavy physical work, lifting and forceful movements, awkward postures, and whole body vibration, are associated with low back disorders. Work-related risk factors account for 28 to 50 percent of the low back problems in an adult population.[30] A number of personal factors may be risk factors for low back pain. These include nonmodifiable factors, such as age and gender, some anthropometric characteristics (for example, height and body build), history of low back problems, and spinal abnormalities as well as modifiable factors, such as weight, physical fitness, smoking, some aspects of lumbar flexibility, trunk muscle strength, and hamstring elasticity. A history of low back problems is one of the most reliable predictors of subsequent back problems.[31]
Arthritis is a leading health problem among all demographic groups, although significant and sometimes surprising disparities exist. Arthritis affects 50 percent of people aged 65 years and older. However, most people with arthritis are younger than age 65 years and of working age.1, 2, 3 Arthritis also affects 285,000 children,[32] making it one of the more common chronic conditions of childhood. Arthritis is more common in women aged 18 years and older than in men and is the leading chronic condition and cause of activity limitation among women.[33], [34]
Whites and African Americans have similar rates of disease, but African Americans have greater rates of activity limitation.1, 2, 3 For African Americans, arthritis is the third most common chronic condition and the leading cause of activity limitation.[35] For Hispanics and American Indians or Alaska Natives, arthritis is the second most common chronic condition and the second leading cause of activity limitation.35 For Asians or Pacific Islanders, arthritis is the fourth most common chronic condition and the second leading cause of activity limitation.35 For whites, arthritis is the most common chronic condition and the second leading cause of activity limitation.35
The rate of arthritis and its associated disabilities is higher among persons with low education and low income.1, 2, 3 African Americans have lower rates of total joint replacement, a surgical procedure that is highly successful in reducing the impact of arthritis in persons with severe pain or disability, than do whites.[36] Certain types of jobs, such as shipyard work, farm work, and occupations that place high knee-bending demands on workers, increase the risks for osteoarthritis.[37], [38]
Osteoporosis is more common among women than men. The rates of disease increase markedly with increasing age. Rates are higher among non-Hispanic white Americans than among Mexican Americans or non-Hispanic African Americans.16 White postmenopausal women are at highest risk of the disease.
The risk for chronic back pain increases with age. Although back pain appears to be equally common in men and women, impairment from back and spine conditions is more common in women.
The importance of physical activity for bone and joint health was highlighted in a 1996 report Physical Activity and Health: A Report of the Surgeon General.[39] Although behavioral interventions seem to have potential benefits, risk factors for the various types of arthritis need to be identified. Recreational or occupational joint injury has been identified as a risk factor for later osteoarthritis, and overweight is a risk factor for osteoarthritis of the knee and possibly the hip and hand.[40] Overweight appears to be a risk factor associated with the progression and severity of osteoarthritis.40, [41]
Genetic research may soon identify persons at high risk for certain types of arthritis and thereby offer a better target for interventions. Current medical care offers considerable relief from pain and other symptoms for all types of arthritis. Available interventions often are not used, however, because of the popular belief that arthritis is part of normal aging, that a person can do nothing about it, and that it affects only old persons. However, early diagnosis and aggressive treatment of rheumatoid arthritis with disease-modifying drugs, for example, appear to reduce its symptoms and related disability.[42], [43], [44], [45], [46], [47]
Educational and behavioral interventions also can relieve symptoms and reduce disability. Telephone contacts with clinicians and several land-based and water exercise programs have had beneficial outcomes.[48], [49], [50], [51] The Arthritis Self-Help Course, a 6-week, 2-hour per week educational intervention, has been shown to reduce pain up to 20 percent beyond what was achieved through conventional medical care.[52] The course has the additional benefit of reducing medical care costs by reducing the number of physician visits for arthritis.52, [53] These and other effective interventions currently are underused, with some reaching less than 1 percent of target populations.[54] Countering myths about arthritis and applying available interventions can help reduce the impact of this health problem. (See Focus Area 6. Disability and Secondary Conditions.)
Interventions for osteoporosis and fractures can be designed to prevent the development of the disease, reduce further bone loss after the occurrence of the disease, and lessen the risk of fractures. Opportunities for primary prevention occur throughout the lifespan and include programs to promote exercise, avoid smoking, reduce excessive alcohol consumption, and improve nutrition, particularly the amount of calcium and vitamin D in the diet. (See Focus Area 19. Nutrition and Overweight.) These approaches may be important in achieving a high peak bone mass during adolescence to delay the onset of osteoporosis as bone mass declines with age. The approaches also may reduce the rate of bone loss later in life.
Women need to be particularly concerned about bone loss occurring at the time of menopause, when bone can be lost at the rate of 2 to 4 percent per year. Women should be counseled on methods to minimize their bone loss. Evidence indicates that older persons, even those who have had a fracture, can benefit from treatment to prevent further bone loss or restore some lost bone to decrease the risk of subsequent fractures.[55]
A wide range of interventions prevent or reduce low back problems. These interventions may include activities designed to reduce the physical demands of work activities by redesigning the task or to address the individual’s specific needs, such as strength or endurance training or counseling for nutrition and lifestyle changes. Ergonomic interventions that are directed at changing the job or work environment have proved effective in reducing risk of occupational low back pain. (See Focus Area 20. Occupational Safety and Health.) Thus, it is reasonable to assume that ergonomic approaches would be effective in preventing chronic LBP as well. Even in a nonwork environment, the physical demands of an activity can be reduced by using ergonomic principles. Interventions involving training in proper lifting techniques, physical conditioning, and weight loss have been investigated in programmatically oriented studies. These have shown that workplace interventions may have an effect on low back disorders.[56] The overall benefits of exercise, nutrition, and lifestyle changes on an individual’s health and well-being would certainly justify efforts in this area. Also, interventions directed at improving strength and endurance may have an important impact on reducing activity limitations due to chronic LBP.
Because national data systems will not be available in the first half of the decade for tracking progress, four subjects of interest concerning arthritis and osteoporosis are not covered in this focus area’s objectives. Representing a research and data collection agenda for the coming decade, the topics involve appropriate management, patient education, provider counseling, and bone fracture prevention. The first addresses persons with systemic rheumatic disease who receive an early specific diagnosis and appropriate management plan. The second topic concerns hospitals, managed care organizations, and large group practices that provide effective, evidence-based arthritis education (including information about community and self-help resources) for patients to use as an integral part of the management of their condition. The third topic concerns health care provider counseling for persons at risk for or who have arthritis. Women aged 65 years and older who are eligible under Medicare criteria to have an initial bone density measurement are the focus of the fourth topic about bone fracture prevention.
The national health objectives for the year 2000 included two objectives for osteoporosis, one objective for chronic back conditions, and no objectives for arthritis. The objective of increasing the proportion of women of menopausal age who have been counseled about estrogen replacement therapy for the prevention of osteoporosis had no data subsequent to the 1994 baseline to chart progress. Annual hip fracture rates increased among people aged 65 years and older, and rates of activity limitation due to chronic back conditions increased from the 1986–88 baseline.
Note: Unless otherwise noted, data are from the Centers for Disease Control and Prevention, National Center for Health Statistics, Healthy People 2000 Review, 1998–99.
Arthritis, Osteoporosis, and Chronic Back Conditions
Goal: Prevent illness and disability related to arthritis and other rheumatic conditions, osteoporosis, and chronic back conditions.
|
Number |
Objective Short Title |
|
Arthritis and Other Rheumatic Conditions |
|
|
2-1 |
Mean number of days without severe pain |
|
2-2 |
Activity limitations due to arthritis |
|
2-3 |
Personal care limitations |
|
2-4 |
Help in coping |
|
2-5 |
Employment rate |
|
2-6 |
Racial differences in total knee replacement |
|
2-7 |
Seeing a health care provider |
|
2-8 |
Arthritis education |
|
Osteoporosis |
|
|
2-9 |
Cases of osteoporosis |
|
2-10 |
Hospitalizationfor vertebral fractures |
|
Chronic Back Conditions |
|
|
2-11 |
Activity limitations due to chronic back conditions |
2-1 | (Developmental) Increase the mean number of days without severe pain among adults who have chronic joint symptoms. |
Potential data sources: Behavioral Risk Factor Surveillance System (BRFSS), CDC, NCCDPHP; National Health Interview Survey (NHIS), CDC, NCHS.
Public health researchers measure days without severe pain by asking, “During the past 30 days, for about how many days did pain make it hard for you to do your usual activities, such as self-care, work, or recreation?” Pain is the most important symptom among persons with arthritis, resulting in the widespread use of conventional prescription and nonprescription medications, surgical interventions, and alternative medical treatments. A measure of pain-free days provides a pertinent and understandable performance-based approach for tracking this key health-related quality of life (HRQOL) determinant for persons with arthritis. Increasing days without severe pain is a feasible target, given more widespread use of available interventions (medical, educational, exercise, nutritional) that are likely to affect this measure. Health surveys variously ask about chronic joint symptoms or arthritis in addressing arthritis and other rheumatic conditions, which is why both terms are used for these objectives.
2-2. | Reduce the proportion of adults with chronic joint symptoms who experience a limitation in activity due to arthritis. |
Target: 21 percent.
Baseline: 27 percent of adults aged 18 years and older with chronic joint symptoms experienced a limitation in activity due to arthritis in 1997 (age adjusted to the year 2000 standard population).
Target setting method: Better than the best.
Data source: National Health Interview Survey (NHIS), CDC, NCHS.
|
Adults Aged 18 Years and
Older |
Limitation |
|
Percent |
|
|
TOTAL |
27 |
|
Race and ethnicity |
|
|
American Indian or Alaska Native |
27 |
|
Asian or Pacific Islander |
18 |
|
Asian |
16 |
|
Native Hawaiian and other Pacific Islander |
DSU |
|
Black or African American |
32 |
|
White |
27 |
|
|
|
|
Hispanic or Latino |
28 |
|
Not Hispanic or Latino |
27 |
|
Black or African American |
32 |
|
White |
27 |
|
Gender |
|
|
Female |
31 |
|
Male |
22 |
|
Family income level |
|
|
Poor |
36 |
|
Near Poor |
30 |
|
Middle/high income |
24 |
|
Education level (aged 25 years and older) |
|
|
Less than high school |
34 |
|
High school graduate |
32 |
|
At least some college |
26 |
DNA = Data have not been analyzed. DNC = Data are not
collected. DSU = Data are statistically unreliable.
Note: Age adjusted to the year 2000 standard population.
2-3. | Reduce the proportion of all adults with chronic joint symptoms who have difficulty in performing two or more personal care activities, thereby preserving independence. |
Target: 1.4 percent.
Baseline: 2.0 percent of adults aged 18 years and older with chronic joint symptoms experienced difficulty performing two or more personal care activities in 1997 (age adjusted to the year 2000 standard population).
Target setting method: Better than the best.
Data source: National Health Interview Survey (NHIS), CDC, NCHS.
|
Adults Aged 18 Years and
Older |
Personal Care Limitations |
|
Percent |
|
|
TOTAL |
2.0 |
|
Race and ethnicity |
|
|
American Indian or Alaska Native |
DSU |
|
Asian or Pacific Islander |
DSU |
|
Asian |
DSU |
|
Native Hawaiian and other Pacific Islander |
DSU |
|
Black or African American |
3.6 |
|
White |
1.8 |
|
|
|
|
Hispanic or Latino |
3.5 |
|
Not Hispanic or Latino |
1.9 |
|
Black or African American |
3.4 |
|
White |
1.7 |
|
Gender |
|
|
Female |
2.2 |
|
Male |
1.6 |
|
Family income level |
|
|
Poor |
5.4 |
|
Near Poor |
2.4 |
|
Middle/high income |
0.9 |
|
Education level (aged 25 years and older) |
|
|
Less than high school |
3.4 |
|
High school graduate |
2.2 |
|
At least some college |
1.4 |
DNA =
Data have not been analyzed. DNC = Data are not collected. DSU = Data are
statistically unreliable.
Note: Age adjusted to the year 2000 standard population.
Arthritis and other rheumatic conditions affect quality of life in many ways and are key items of personal interest to individuals with these conditions.7, 8, [57], [58], [59], [60], [61] From a public health perspective, validated measures of HRQOL are essential for monitoring the impact of clinical and public health interventions.
Activity limitation occurs frequently among persons with arthritis and is an important functional element that can compromise independence. Activity limitation affects 27 percent of all persons who have arthritis,1 making it the number one cause of activity limitations in the United States.5 The activity limitations of arthritis also indirectly affect health and independence by decreasing physical activity, increasing weight, and placing persons at higher risk for all the adverse outcomes of those risk factors.
As the leading cause of disability, arthritis is a leading cause of difficulty in performing personal care activities and thereby a leading cause of loss of independence. Therefore, maintaining independence, especially in personal care, is important for persons with arthritis.
2-4. | (Developmental) Increase the proportion of adults aged 18 years and older with arthritis who seek help in coping if they experience personal and emotional problems. |
Potential data sources: National Health Interview Survey (NHIS), CDC, NCHS; Behavioral Risk Factor Surveillance System (BRFSS), CDC, NCCDPHP.
Coping difficulties, depression, anxiety, and low self-efficacy are recognized as major personal and emotional problems among persons with arthritis.12 These problems are especially frequent among persons who experience physical pain. Because arthritis is a leading cause of chronic pain, monitoring these mental health outcomes can help assess the success of applied interventions.13
2-5. | Increase the employment rate among adults with arthritis in the working-aged population. |
Target: 78 percent.
Baseline: 67 percent of adults aged 18 to 64 years with arthritis were employed in the past week in 1997 (age adjusted to the year 2000 standard population).
Target setting method: Better than the best.
Data source: National Health Interview Survey (NHIS), CDC, NCHS.
|
Adults Aged 18 to 64 Years With Arthritis, 1997 |
Employed
in |
|
Percent |
|
|
TOTAL |
67 |
|
Race and ethnicity |
|
|
American Indian or Alaska Native |
46 |
|
Asian or Pacific Islander |
56 |
|
Asian |
54 |
|
Native Hawaiian and other Pacific Islander |
DSU |
|
Black or African American |
52 |
|
White |
69 |
|
|
|
|
Hispanic or Latino |
60 |
|
Not Hispanic or Latino |
67 |
|
Black or African American |
53 |
|
White |
70 |
|
Gender |
|
|
Female |
60 |
|
Male |
74 |
|
Family income level |
|
|
Poor |
39 |
|
Near Poor |
54 |
|
Middle/high income |
77 |
|
Education level (aged 25 to 64 years) |
|
|
Less than high school |
47 |
|
High school graduate |
65 |
|
At least some college |
78 |
DNA = Data have not been analyzed. DNC = Data are not
collected. DSU = Data are statistically unreliable.
Note: Age adjusted to the year 2000 standard population.
Labor force participation rates (which parallel employment rates) for all persons of working age (18 to 64 years) in 1994 were 71 percent for females and 87 percent for males.11 Rates for persons with arthritis, however, are far below these numbers.11 A part of this low rate may be increased through early diagnosis and appropriate management, improved self-management, and improved job retention efforts. Raising this low rate will help foster independence for affected persons and reduce the demands on families and society. Reducing demands on families and society is particularly important as demographic changes lead to fewer workers for each nonworker.
2-6. | (Developmental) Eliminate racial disparities in the rate of total knee replacements. |
Potential data sources: Medicare data, HCFA; National Hospital Discharge Survey (NHDS), CDC, NCHS; Hospital Cost and Utilization Project (HCUP), AHRQ.
Studies have shown that African Americans have much lower rates of total knee replacement than whites, even when adjusted for age, gender, and insurance coverage.36 The reasons for this difference are unclear, but the effect is that many persons are not getting needed interventions to reduce pain and disability. This is one component of a more widespread problem of racial differences in medical care that is difficult to explain by financial or access-to-care issues.
2-7. | (Developmental) Increase the proportion of adults who have seen a health care provider for their chronic joint symptoms. |
Potential data source: National Health Interview Survey (NHIS) CDC, NCHS.
Studies using the 1989 National Health Interview Survey have shown that 16 percent of adults aged 18 years and older have not seen a doctor for their arthritis.[62] Appropriate medical management, patient and provider education, improved self-management, and physical activity—all encouraged by providers—can reduce arthritis pain and disability. Increasing the percentage of persons who seek a diagnosis and treatment from a health care provider for their chronic joint symptoms is an objective amenable to public awareness campaigns to counter the myths that arthritis is part of normal aging and nothing can be done for it. This objective is especially important for the working-aged population, the upper age limit of which is likely to rise as the overall population ages through the 2030s.
2-8. | (Developmental) Increase the proportion of persons with arthritis who have had effective, evidence-based arthritis education as an integral part of the management of their condition. |
Potential data sources: National Health Interview Survey (NHIS), CDC, NCHS; Behavioral Risk Factor Surveillance System (BRFSS), CDC, NCCDPHP.
Existing evidence-based education interventions, such as the Arthritis Self-Help Course, are effective in reducing arthritis pain and reducing physician visits for arthritis.52 These beneficial interventions, which include information about community and self-help resources, are estimated to reach less than 1 percent of the population with arthritis.54 Expanding the dissemination of the benefits of interventions currently available offers the opportunity of quickly improving the health of all persons with arthritis and reducing the impact of arthritis nationally. Education efforts should be provided in a culturally and linguistically competent manner.
2-9. | Reduce the proportion of adults with osteoporosis. |
Target: 8 percent.
Baseline: 10 percent of adults aged 50 years and older had osteoporosis as measured by low total femur bone mineral density (BMD) in 1988–94 (age adjusted to the year 2000 standard population).
Target setting method: 20 percent improvement.
Data source: National Health and Nutrition Examination Survey (NHANES), CDC, NCHS.
|
Adults Aged 50 Years and Older, 1988–94 |
Osteoporosis |
|
Percent |
|
|
TOTAL |
10 |
|
Race and ethnicity |
|
|
American Indian or Alaska Native |
DSU |
|
Asian or Pacific Islander |
DSU |
|
Asian |
DNC |
|
Native Hawaiian and other Pacific Islander |
DNC |
|
Black or African American |
7 |
|
White |
10 |
|
|
|
|
Hispanic or Latino |
DSU |
|
Mexican American |
10 |
|
Not Hispanic or Latino |
10 |
|
Black or African American |
7 |
|
White |
10 |
|
Gender |
|
|
Female |
16 |
|
Male |
3 |
|
Education level |
|
|
Less than high school |
11 |
|
High school graduate |
11 |
|
At least some college |
9 |
DNA = Data have not been analyzed. DNC = Data are not
collected. DSU = Data are statistically unreliable.
Note: Age adjusted to the year 2000 standard population.
BMD has been identified as one of the primary predictive factors for osteoporosis-related fractures.[63], [64], [65] Osteoporosis is defined as a BMD value that is more than 2.5 standard deviations below that of an average young adult.[66]
The proportion of adults aged 50 years and older with osteoporosis in the total femur region is 10 percent (16 percent in women and 3 percent in men). Osteoporosis occurs in nonwhite women and in men, although the rates of disease are not as high as the rates found among white women. These estimates are based on the total femur; estimates based on a different skeletal site (or combination of sites) may differ. For example, the proportion of white women with osteoporosis in Olmsted County, Minnesota, was established to be approximately 16 to 17 percent at the femur, lumbar spine, or wrist when each site was considered separately. However, 30 percent of women had osteoporosis in at least one of the three sites.[67]
Osteoporosis is a major risk factor for hip fracture. Virtually all persons with a hip fracture are hospitalized for treatment.21 Two-thirds of persons who fracture a hip do not return to their prefracture level of functioning. Health care expenditures for hip fractures in 1995 have been estimated at $8.7 billion.18 Interventions that reduce the rate of osteoporosis should have a marked impact on the rate of hip fractures. Estimates indicate that osteoporosis contributes to 90 percent of hip fractures in women and 80 percent of hip fractures in men.65 Increasing BMD by 5 percent may decrease the risk of fractures by 25 percent.[68]
Although osteoporosis increases the risk of fractures, most hip fractures result from falls.66 Some risk factors associated with falls may be amenable to interventions. These risk factors include impaired vision, use of long-acting psychotropic drugs, physical inactivity, muscle weakness, and poor health.[69] (See Focus Area 15. Injury and Violence Prevention.)
2-10. | Reduce the proportion of adults who are hospitalized for vertebral fractures associated with osteoporosis. |
Target: 14.0 hospitalizations per 10,000 adults aged 65 years and older.
Baseline: 17.5 hospitalizations per 10,000 adults aged 65 years and older were for vertebral fractures associated with osteoporosis in 1998 (age adjusted to the year 2000 standard population).
Target setting method: 20 percent improvement.
Data source: National Hospital Discharge Survey (NHDS), CDC, NCHS.
|
Adults Aged 65 Years and Older, 1998 |
Hospitalizations for Vertebral Fractures Associated With Osteoporosis |
|
Rate per 10,000 |
|
|
TOTAL |
17.5 |
|
Race and ethnicity |
|
|
American Indian or Alaska Native |
DSU |
|
Asian or Pacific Islander |
DSU |
|
Asian |
DNC |
|
Native Hawaiian and other Pacific Islander |
DNC |
|
Black or African American |
DSU |
|
White |
14.0 |
|
|
|
|
Hispanic or Latino |
DSU |
|
Not Hispanic or Latino |
DSU |
|
Black or African American |
DSU |
|
White |
DSU |
|
Gender |
|
|
Female |
19.6 |
|
Male |
13.9 |
|
Select populations |
|
|
Age groups (not age adjusted) |
|
|
65 to 74 years |
6.7 |
|
75 to 84 years |
26.0 |
|
85 years and older |
39.0 |
DNA = Data have not been analyzed. DNC = Data are not
collected. DSU = Data are statistically unreliable.
Note: Age adjusted to the year 2000 standard population.
Vertebral fractures are the most common fracture due to osteoporosis.[70] About 30 to 50 percent of women and 20 to 30 percent of men will experience vertebral fractures in their lifetime.70 The overall number of cases of these fractures rises rapidly with increasing age. Among white women, the rate rises from 6 percent among those aged 50 to 59 years to about 75 percent among those aged 90 years and older.[71] Most of these fractures cause little difficulty and go unrecognized. However, 33 percent of the fractures will be diagnosed clinically, 8 percent will require hospitalization,[72] and about 2 percent will require long-term nursing care.[73]
The most common symptom of vertebral fractures is back pain, which is reported in about half of the cases. People with these fractures are more likely to have difficulty performing activities of daily living, such as bending, reaching above the head, and walking. Changes in the outward appearance of people experiencing these fractures is a loss of height and the development of a humped back.70
Interventions that reduce the number of persons with osteoporosis should reduce the rates of vertebral fractures. Falls associated with fractures at other sites do not play a prominent role in these fractures. Normal daily activities can place sufficient stress on the vertebra to cause fractures.71
For discussion of calcium and vitamin D, see Focus Area 19. Nutrition and Overweight.
2-11. | Reduce activity limitation due to chronic back conditions. |
Target: 25 adults per 1,000 population aged 18 years and older.
Baseline: 32 adults per 1,000 population aged 18 years and older experienced activity limitation due to chronic back conditions in 1997 (age adjusted to the year 2000 standard population).
Target setting method: Better than the best.
Data source: National Health Interview Survey (NHIS), CDC, NCHS.
|
Adults Aged 18 Years and Older, 1997 |
Activity Limitation Due to Chronic Back Conditions |
|
Rate per 1,000 |
|
|
TOTAL |
32 |
|
Race and ethnicity |
|
|
American Indian or Alaska Native |
68 |
|
Asian or Pacific Islander |
18 |
|
Asian |
15 |
|
Native Hawaiian and other Pacific Islander |
DSU |
|
Black or African American |
36 |
|
White |
31 |
|
|
|
|
Hispanic or Latino |
28 |
|
Not Hispanic or Latino |
32 |
|
Black or African American |
36 |
|
White |
32 |
|
Gender |
|
|
Female |
32 |
|
Male |
31 |
|
Family income level |
|
|
Poor |
77 |
|
Near Poor |
53 |
|
Middle/high income |
24 |
|
Education level (aged 25 years and older) |
|
|
Less than high school |
54 |
|
High school graduate |
35 |
|
Some college |
28 |
DNA = Data have not been analyzed. DNC = Data are not
collected. DSU = Data are statistically unreliable.
Note: Age adjusted to the year 2000 standard population.
Persons who are overweight and persons who frequently bend over or lift heavy objects are at risk for low back injuries.[74] Occupations that require repetitive lifting, particularly in a forward bent and twisted position, place employees at especially high risk. Other risk factors for low back injury include exposure to vibration produced by vehicles or industrial machinery, prolonged vehicle driving, and certain sports activities. 24 , 25, 26, [75], [76] Predictors of back problems may include diminished lumbar flexibility, trunk muscle strength, and hamstring elasticity.[77] Osteoporosis increases the risk of vertebral compression, which may account for the increase in reported low back pain in older females.[78], [79] Increased age also is associated with back pain.[80] In addition, persons who have experienced back problems in the past are at increased risk for future injury. 80, [81]
(A listing of abbreviations and acronyms used in this publication appears in Appendix H.)
Activity limitations: Problems in a person’s performance of everyday functions such as communication, self-care, mobility, learning, and behavior.
Arthritis: Shorthand for arthritis and other rheumatic conditions.
Arthritis and other rheumatic conditions: More than 100 conditions (or diseases or problems) that primarily affect the joints, muscles, fascia, tendons, bursa, ligaments, and other connective tissues of the body.
Bone mineral density (BMD): Measurement used to determine the presence of osteoporosis.
Chronic back conditions: Low back pain and other conditions affecting only the back.
Chronic joint symptoms: Pain, aching, stiffness, or swelling in or around a joint that was present on most days for at least 1 month in the past 12 months.
Disability: General term used to represent the interactions between individuals with a health condition and barriers in their environment. The term disability is operationalized as self-reported activity limitations or use of assistive devices or equipment related to an activity limitation.
Musculoskeletal conditions: Problems that affect the skeleton, joints, muscles, and connective tissues of the body.
Osteoarthritis: A slowly progressive, degenerative joint disease that results from the breakdown of cartilage and leads to pain and stiffness; usually affects the knees, hips, and hands; the most common form of arthritis.
Osteopenia: A condition similar to osteoporosis (see below) except the reduction in bone mass is not as severe.
Osteoporosis: Bone disease characterized by a reduction of bone mass and a deterioration of the microarchitecture of the bone leading to bone fragility.
Personal care activities: Eating, bathing, dressing, or getting around inside the home, including getting in or out of bed or chairs and using the toilet (including getting to the toilet).
Rheumatoid arthritis: A chronic, inflammatory disease of the body that produces its most prominent manifestations in joints, often leading to joint pain, stiffness, and deformity.
Work disability: Limited in the amount or kind of work; unable to work.
[1] Centers for Disease Control and Prevention (CDC). Arthritis prevalence and activity limitations—United States, 1990. Morbidity and Mortality Weekly Report 43(24):433-438, 1994. PubMed; PMID 8202076
[2] Lawrence, R.C.; Helmick, C.G.; Arnett, F.C.; et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis & Rheumatism 41(5):778-799, 1998. PubMed; PMID 9588729
[3] Helmick, C.G.; Lawrence, R.C.; Pollard, R.A.; et al. Arthritis and other rheumatic conditions: Who is affected now, who will be affected later? National Arthritis Data Workgroup Arthritis Care and Research 8:203-211, 1995. PubMed; PMID 8605258
[4] CDC. Impact of arthritis and other rheumatic conditions on the health-care system. Morbidity and Mortality Weekly Report 48(17):349-353, 1999. PubMed; PMID 10363958
[5] CDC. Current trends: Prevalence of disabilities and associated health conditions—United States, 1991–1992. Morbidity and Mortality Weekly Report 43(40):730-731, 737-739, 1994. PubMed; PMID 7935302
[6] LaPlante, M.P. Data on Disability from the National Health Interview Survey, 1983–1985. Washington, DC: National Institute on Disability and Rehabilitation Research (NIDRR), U.S. Department of Education (DOE), 1988.
[7] CDC. Health-related quality of life and activity limitation—8 states, 1995. Morbidity and Mortality Weekly Report 47(67):134-140, 1998. PubMed; PMID 9498296
[8] CDC. State differences in reported healthy days among adults—United States, 1993–1996. Morbidity and Mortality Weekly Report 47(12):239-243, 1998. PubMed; PMID 9572632
[9] CDC. Targeting Arthritis: The Nation’s Leading Cause of Disability. At-a-Glance, 1998. Atlanta, GA: Technical Information and Editorial Services Branch, National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP), CDC, 1998.
[10] Yelin, E., and Callahan, L.F. The economic cost and social and psychological impact of musculoskeletal conditions. Arthritis & Rheumatism 38(10):1351-1362, 1995. PubMed; PMID 7575685
[11] Trupin, L.; Sebesta, D.S.; Yelin, E.; et al. Trends in Labor Force Participation Among Persons With Disability, 1983–1994. Disability Statistics Report 10. Washington, DC: DOE, NIDRR, 1997.
[12] Frank, R.G., and Hagglund, K.J. Mood disorders. In: Wegener, S.T., ed. Clinical Care in the Rheumatic Diseases. Atlanta, GA: American College of Rheumatology, 1996, 125-130.
[13] Bradley, L.A.; Wegener, S.T.; Belza, B.L.; et al. Pain management interventions for patients with rheumatic diseases. In: Melvin, J., and Jensen, G., eds. Rheumatologic Rehabilitation Series Volume I: Assessment and Management. Rockville, MD: American Occupational Therapy Association, 1998, 259-278.
[14] Wolf, F. The natural history of rheumatoid arthritis. Journal of Rheumathology 23(Suppl. 44):13-22, 1996.
[15] Boult, C.; Altmann, M.; Gilbertson, D.; et al. Decreasing disability in the 21st century: The future effects of controlling six fatal and non-fatal conditions. American Journal of Public Health 86:1388-1393, 1996. PubMed; PMID 8876506
[16] Looker, A.C.; Orwoll, E.S.; Johnston, C.C.; et al. Prevalence of low femoral bone density in older U.S. adults from NHANES III. Journal of Bone and Mineral Research 12(11):1761-1768, 1997. PubMed; PMID 9383679
[17] Riggs, B.L., and Melton, III, L.J. The worldwide problem of osteoporosis: Insights afforded by epidemiology. Bone 17(Suppl. 5):505S-511S, 1995. PubMed; PMID 8573428
[18] Ray, N.F.; Chan, J.K.; Thamer, M.; et al. Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: Report from the National Osteoporosis Foundation. Journal of Bone and Mineral Research 12(1):24-35, 1997. PubMed; PMID 9240722
[19] Melton, III, L.J.; Chrischilles, E.A.; Cooper, C.; et al. How many women have osteoporosis? Journal of Bone and Mineral Research 7:1005-1010, 1992. PubMed; PMID 1414493
[20] Bacon, W.E. Secular trends in hip fracture occurrence and survival: Age and sex differences. Journal of Aging Health 8(4):538-553, 1996. PubMed; PMID 10182385
[21] U.S. Congress, Office of Technology Assessment. Hip Fracture Outcomes in People Age 50 and Over—Background Paper. OTA-BP-H-120. Washington, DC: U.S. Government Printing Office, July 1994.
[22] Anderson, G.B.J. The epidemology of spinal disorders. In: Frymoyer, J.W., ed. The Adult Spine: Principles and Practice. 2nd ed. Philadelphia, PA: Lippencott-Raven, 1997.
[23] Biering-Sorensen, F. Physical measurements as risk indicators for low-back trouble over a one year period. Spine 9:106-119, 1984. PubMed; PMID 6233709
[24] Frymoyer, J.W.; Pope, M.H.; Clements, J.H.; et al. Risk factors in low-back pain: An epidemiological survey. Journal of Bone and Joint Surgery 65(2):213-218, 1983. PubMed; PMID 6218171
[25] Frymoyer, J.W. Back pain and sciatica. New England Journal of Medicine 318(5):291-300, 1988. PubMed; PMID 2961994
[26] Svensson, H.O., and Anderson, G.B.J. Low-back pain in 40- to 47-year-old men: Work history and work environment factors. Spine 8(3):272-276, 1983. PubMed; PMID 6226117
[27] Anderson, G.B. Epidemiological aspects on low back pain in industry. Spine 6(1):53-60, 1981. PubMed; PMID 6451937
[28] Kelsey, J.L.; White, A.A.; Pastides, H.; et al. The impact of musculoskeletal disorders on the population of the United States. Journal of Bone and Joint Surgery 61(7):959-964, 1979. PubMed; PMID 158597
[29] Praemer, A.; Furner, S.; and Rice, D.P. Musculoskeletal conditions in the United States. Park Ridge, IL: American Academy of Orthoscopic Surgery, 1992.
[30] Wegman, D.H., and Fine, L.J. Occupational and Environmental Medicine. Journal of the American Medical Association 275(23):1831-1832, 1996. PubMed; PMID 8642735
[31] Shelerud, R. Epidemiology of Occupational Low Back Pain. In: Occupational Medicine: State of the Art Reviews. Philadelphia, PA: Hanley and Belfus, 1998, 1-22.
[32] CDC. NCCDPHP, Division of Adult and Community Health, Health Care and Aging Studies Branch, Atlanta, GA, unpublished data, 1990.
[33] CDC. Prevalence and impact of arthritis among women. United States, 1989–1991. Morbidity and Mortality Weekly Report 44(17):329-334, 517-518, 1995. PubMed; PMID 7715591
[34] Callahan, L.F.; Rao, J.; and Boutaugh, M. Arthritis and women’s health: Prevalence, impact, and prevention. American Journal of Preventive Medicine 12(5):401-409, 1996. PubMed; PMID 8909652
[35] CDC. Prevalence and impact of arthritis by race and ethnicity—United States, 1989–1991. Morbidity and Mortality Weekly Report 45(18):373-378, 1996. PubMed; PMID 8606687
[36] Wilson, M.G.; May, D.S.; and Kelly, J.J. Racial differences in the use of total knee arthroplasty for osteoarthritis among older Americans. Ethnicity & Disease 4(1):57-67, 1994. PubMed; PMID 7742733
[37] Hochberg, J.C. Osteoarthritis. In: Silman, A.J., and Hochberg, J.C., eds. Epidemiology of the Rheumatic Diseases. Oxford: Oxford University Press, 1993, 257-288.
[38] Felson, D.T. Epidemiology of hip and knee osteoarthritis. Epidemiologic Reviews 10:1-28, 1988. PubMed; PMID 3066625
[39] U.S. Department of Health and Human Services (HHS). Physical Activity and Health: A Report of the Surgeon General. Atlanta, GA: HHS, CDC, 1996.
[40] Felson, D.T., and Zhang, Y. Personal communication. An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. August 1998.
[41] Felson, D.T.; Zhang, Y.; Anthony, J.M.; et al. Weight loss reduces the risk for symptomatic knee osteoarthritis in women. The Framingham Study. Annals of Internal Medicine 116(7):535-539, 1992. PubMed; PMID 1543306
[42] Weinblatt, M.E. Rheumatoid arthritis: Treat now, not later! (Editorial). Annals of Internal Medicine 124:773-774, 1996. PubMed; PMID 8633840
[43] Van der Heide, A.; Jacobs, J.W.; Bijlsma, J.W.; et al. The effectiveness of early treatment with “second-line” antirheumatic drugs. A randomized, controlled trial. Annals of Internal Medicine 124(8):699-707, 1996. PubMed; PMID 8633829
[44] Fries, J.F.; Williams, C.A.; Morrfeld, D.; et al. Reduction in long-term disability in patients with rheumatoid arthritis by disease-modifying antirheumatic drug-based treatment strategies. Arthritis & Rheumatism 39:616-622, 1996. PubMed; PMID 8630111
[45] Egsmose, C.; Lund, B.; Borg, G.; et al. Patients with rheumatoid arthritis benefit from early 2nd line therapy: 5-year follow up of a prospective double blind placebo controlled study. Journal of Rheumatology 22:2208-2213, 1995. PubMed; PMID 8835550
[46] Kirwan, J.R. The Arthritis and Rheumatism Council, Low-Dose Glucocorticoid Study Group. The effect of glucocorticoids on joint destruction in rheumatoid arthritis. New England Journal of Medicine 333(3):142-146, 1995. PubMed; PMID 7791815
[47] Emery, P., and Salmon, M. Early rheumatoid arthritis: Time to aim for remission? Annals of Rheumatic Diseases 54:944-947, 1995. PubMed; PMID 8546524
[48] Maisiak, R.; Austin, J.; and Heck, L. Health outcomes of two telephone interventions for patients with rheumatoid arthritis or osteoarthritis. Arthritis & Rheumatism 39:1391-1399, 1996. PubMed; PMID 8702449
[49] Minor, M.A. Arthritis and exercise: The times they are a-changin’ (Editorial). Arthritis Care and Research 9:9-81, 1996. PubMed; PMID 8970264
[50] Minor, M.A., and Kay, D.R. Arthritis. In: Exercise Management for Persons With Chronic Diseases and Disabilities. Champaign, IL: Human Kinetics, 1997.
[51] Puett, D.W., and Griffin, M.R. Published trials of nonmedicinal and noninvasive therapies for hip and knee osteoarthritis. Annals of Internal Medicine 121(2):133-140, 1994. PubMed; PMID 8017727
[52] Lorig, K.R.; Mazonson, P.D.; and Holman, H.R. Evidence suggesting that health education for self-management in patients with chronic arthritis has sustained health benefits while reducing health care costs. Arthritis & Rheumatism 36(4):439-446, 1993. PubMed; PMID 8457219
[53] Kruger, J.M.S.; Helmick, C.G.; Callahan, L.F.; et al. Cost-effectiveness of the Arthritis Self-Help Course. Archives of Internal Medicine, 1998. PubMed; PMID 9625404
[54] Boutaugh, M., Group Vice President, Health Promotion, Arthritis Foundation. Personal communication. August 1999.
[55] Seeman, E. Introduction. American Journal of Medicine 103(Suppl. 2a):1S-2S, 1997.
[56] Violinn, E. Do workplace interventions prevent low-back disorders? If so: Why?: A methodological commentary. Erognomics 42(1):258-272, 1999. PubMed; PMID 9973883
[57] Hennessy, C.H.; Moriarty, D.G.; Zack, M.M.; et al. Measuring health-related quality of life for public health surveillance. Public Health Reports 109(5):665-672, 1994. PubMed; PMID 7938388
[58] CDC. Quality of life as a new public health measure—Behavioral Risk Factor Surveillance System, 1993. Morbidity and Mortality Weekly Report 43(20):375-380, 1994. PubMed; PMID 8183229
[59] CDC. Health-related quality-of-life measures—United States, 1993. Morbidity and Mortality Weekly Report 44(11):195-200, 1995. PubMed; PMID 7885309
[60] Newschaffer, C.J. Validation of BRFSS HRQOL Measures in a Statewide Sample. Atlanta, GA: HHS, Public Health Service, CDC, NCCDPHP, 1998.
[61] Verbrugge, L.M.; Merrill, S.S.; and Liu, X. Measuring disability with parsimony. Disability Rehabilitation 21(5-6):295-306, 1999. PubMed; PMID 10381242
[62] Rao, J.K.; Callahan, L.F.; and Helmick, C.G. Characteristics of persons with self-reported arthritis and other rheumatic conditions who do not see a doctor. Journal of Rheumatology 24:169-173, 1997. PubMed; PMID 9002029
[63] Cummings, S.R.; Black, D.M.; Nevitt, M.C.; et al. Bone density at various sites for prediction of hip fractures. Lancet 341(8837):72-75, 1993. PubMed; PMID 1543306
[64] Melton, III, L.J.; Atkinson, E.J.; O’Fallon, W.M.; et al. Long-term fracture prediction by bone mineral assessed at different skeletal sites. Journal of Bone and Mineral Research 8(10):1227-1233, 1993. PubMed; PMID 8256660
[65] Melton, III, L.J.; Thamer, M.; Ray, N.F.; et al. Fractures attributable to osteoporosis: Report from the National Osteoporosis Foundation. Journal of Bone and Mineral Research 12(1):16-23, 1997. PubMed; PMID 9240721
[66] World Health Organization (WHO). Assessment of Fracture Risk and Its Application to Screening for Postmenopausal Osteoporosis. Technical Report Series No. 843. Geneva, Switzerland: WHO, 1994.
[67] Melton, III, L.J. How many women have osteoporosis now? Journal of Bone and Mineral Research 10(2):175-177, 1995. PubMed; PMID 7754796
[68] Lips, P. Prevention of hip fractures: Drug therapy. Bone 18(Suppl. 3):159S-163S, 1996. PubMed; PMID 8805996
[69] Cummings, S.R. Treatable and untreatable risk factors for hip fracture. Bone 18 (Suppl. 3):165S-176S, 1996. PubMed; PMID 8777083
[70] Ross P.D. Clinical consequences of vertebral fractures. American Journal of Medicine 103:30S-43S, 1997. PubMed; PMID 9302895
[71] Melton, III, L.J.; Kan, S.H.; Frye, M.A.; et al. Epidemiology of vertebral fractures in women. American Journal of Epidemiology 129:1000-1011, 1989. PubMed; PMID 2784934
[72] Jacobsen, S.J.; Cooper, C.; Gottlieb, M.S.; et al. Hospitalization with vertebral fracture among the aged: A national population-based study 1986–1989. Epidemiology 3(6):515-518, 1992. PubMed; PMID 1420517
[73] Chrischilles, E.A.; Butler, C.D.; Davis, S.C.; et al. A model of lifetime osteoporosis impact. Archives of Internal Medicine 151(10):2026-2032, 1991. PubMed; PMID 1929691
[74] Schuchmann, J.A. Low back pain: A comprehensive approach. Comprehensive Therapy 14(1):14-18, 1988. PubMed; PMID 2963722
[75] Kelsey, J.L.; Githens, P.B.; White, III, A.A.; et al. An epidemiologic study of lifting and twisting on the job and risk for acute, prolapsed lumbar vertebral disc. Journal of Orthopaedic Research 2(1):61-66, 1984. PubMed; PMID 6491800
[76] Kelsey, J.L.; Githens, P.B.; O’Conner, T.; et al. Acute prolapsed lumbar intervertebral disc. An epidemiologic study with special reference to driving automobiles and cigarette smoking. Spine 9(6):608-613, 1984. PubMed; PMID 6495031
[77] Parnianpour, M.; Bejjani, F.J.; and Pavlidis, L. Worker training: The fallacy of single, correct lifting technique. Ergonomics 30(2):331-334, 1987. PubMed; PMID 3582345
[78] Porter, R.W.; Hibbert, C.; and Wellman, P. Backache and the lumbar spinal canal. Spine 5(2):99-105, 1980. PubMed; PMID 6446166
[79] Buchanan, J.R.; Myers, C.; Greer, III, R.B.; et al. Assessment of the risk of vertebral fracture in menopausal women. Journal of Bone and Joint Surgery 69(2):212-218, 1987. PubMed; PMID 3805081
[80] Chaffin, D.B., and Park, K.S. A longitudinal study of low back pain as associated with occupational weight lifting factors. American Industrial Hygiene Association Journal 34(12):513-525, 1973. PubMed; PMID 4272346
[81] Venning, P.J.; Walter, S.D.; and Stitt, L.W. Personal and job-related factors as determinants of incidence of back injuries among nursing personnel. Journal of Occupational Medicine 29(10):820-825, 1987. PubMed; PMID 2960792