Appendix F: PowerPoint Presentation: Executive Summary
Slides:
Slide 1: Improving Patient Safety Systems for LEP Patients
Slide 2: Improving Patient Safety Systems for LEP Patients (continued)
Slide 3: Improving Patient Safety Systems for LEP Patients (continued)
Slide 4: What We Know About Patient Safety and LEP
Slide 5: What We Know About Patient Safety and LEP
Slide 6: Why Focus on LEP and Patient Safety?
Slide 7: Why Focus on LEP and Patient Safety? (continued)
Slide 8: Why Focus on LEP and Patient Safety? (continued)
Slide 9: Why Focus on LEP and Patient Safety? (continued)
Slide 10: Causes of Adverse Events for LEP and Culturally Diverse Patients
Slide 11: Systems and Strategies To Improve Safety for LEP Patients
Slide 12: Five Recommendations To Improve Patient Safety
Slide 13: Systems and Strategies To Improve Safety for LEP Patients: Culture
Slide 14: Systems and Strategies To Improve Safety for LEP Patients: Identification
Slide 15: Systems and Strategies To Improve Safety for LEP Patients: Reporting
Slide 16: Systems and Strategies To Improve Safety for LEP Patients: Monitor
Slide 17: Systems and Strategies To Improve Safety for LEP Patients: Address
Slide 18: Systems and Strategies To Improve Safety for LEP Patients: Address (continued)
Slide 19: Specific Recommendations for High-Risk Scenarios
Slide 20: Improving Team Communication To Foster Safety for LEP Patients: TeamSTEPPS®
Slide 21: Improving Team Communication To Foster Safety for LEP Patients: TeamSTEPPS® (continued)
Slide 22: Summary
Slide 23: References
Slide 1. Improving Patient Safety Systems for Limited English Proficiency (LEP) Patients: A Guide for Hospitals

Slide 2. Improving Patient Safety Systems for LEP Patients

- Goal of the Guide:
- Help hospital leaders better understand how to address the issue of patient safety for limited-English proficient (LEP) and culturally diverse patients
- The Guide provides guidance on how to:
- Foster a Supportive Culture for Safety of Diverse Patient Populations
- Adapt Current Systems to Better Identify Medical Errors among LEP Patients
- Improve Reporting of Medical Errors for LEP Patients
- Routinely Monitor Patient Safety for LEP Patients
- Address Root Causes to Prevent Medical Errors among LEP Patients
Slide 3. Improving Patient Safety Systems for LEP Patients
- This presentation will:
- Highlight what we know about patient safety and LEP patients
- Provide evidence for why we should focus on LEP patient safety
- Identify common causes of adverse events for LEP and culturally diverse patients
- Present five key strategies for how to improve detection of medical errors and prevent high-risk scenarios from becoming safety events
Slide 4. What We Know About Patient Safety and LEP

- The Institute of Medicine Report To Err is Human: Building a Safer Health System states patients should not be harmed by care that is intended to help them
- The Institute of Medicine Report Crossing the Quality Chasm defined patient safety as one of the essential components of high quality health care
- Patient safety efforts are now a central component of strategies to improve quality of care for all patients
Images of report covers are also shown.
Slide 5. What We Know About Patient Safety and LEP
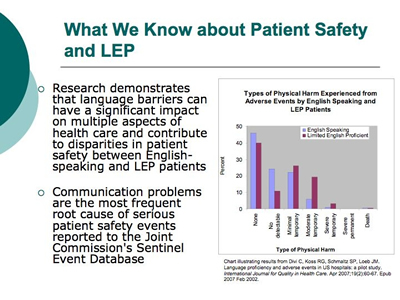
- Research demonstrates that language barriers can have a significant impact on multiple aspects of health care and contribute to disparities in patient safety between English-speaking and LEP patients
- Communication problems are the most frequent root cause of serious patient safety events reported to the Joint Commission's Sentinel Event Database
Chart illustrating results from Divi C, Koss RG, Schmaltz SP, Loeb JM. Language proficiency and adverse events in U.S. hospitals: a pilot study. International Journal for Quality in Health Care April 2007;19(2):60-67. Types of Physical Harm Experienced From Adverse Events by English Speaking and LeP Patients. Bar chart showing percentage of patients in each group experiencing physical harm. The percentage of patients experiencing harm was higher for LEP patients than for English speaking patients. About 70 percent of English speaking patients experienced no harm or no detectable harm. For LEP patients, only about half experienced no harm or no detectable harm.
Slide 6. Why Focus on LEP and Patient Safety?

- A Large and Growing Population
- Minority groups are the nation’s fastest-growing demographic accounting for one-third of U.S. population
- Nearly 25 million (8.6%) of U.S. population are defined as LEP and therefore at risk for adverse events because of language barriers and culture
Slide 7. Why Focus on LEP and Patient Safety?
- Patient Safety, Quality, and Cost Drivers
- Greater risk of line infections, surgical infections, falls, and pressure ulcers, due to LEP patients’ longer hospital stays compared to English-speaking patients with the same clinical condition
- Greater risk of surgical delays and readmission due to LEP patients’ greater difficulty understanding instructions including how to prepare for a procedure, manage their condition, take their medications, and which symptoms should prompt a return to care, or when to follow up
Slide 8. Why Focus on LEP and Patient Safety?
- Risk Management
- Multiple liability exposures arise when providing care to LEP populations
- These may include situations relating to:
- Patient comprehension of medical condition
- Treatment plan
- Discharge instructions
- Complications and follow-up
- Inaccurate and incomplete medical history
- Ineffective or improper use of medications or serious medication errors
- Improper preparation for tests and procedures
- Poor or inadequate informed consent
Slide 9. Why Focus on LEP and Patient Safety?
- Accreditation Standards
- In 2011, the Joint Commission published Patient-Centered Communication standards in the Comprehensive Accreditation Manual for Hospitals (CAMH): The Official Handbook
- These standards emphasize the importance of effective communication, cultural competence, and patient-centered care as important elements of providing safe quality of care
Image of manual cover.
Slide 10. Common Causes: Adverse Events for LEP Culturally Diverse Patients

- Use of Family Members/Friends or Non-Qualified Staff as Interpreters
- Family members and friends typically don’t understand subtle nuances of language and culture that may influence the interaction, and will not question use of medical terminology
- Research confirms that bilingual hospital staff often serve as ad hoc interpreters for LEP patients, despite evidence that they are more likely to make clinically significant mistakes than qualified medical interpreters
- Use of Basic Language Skills to “Get By”
- Clinicians with basic or intermediate foreign language skills often attempt to “make do” or “get by” without the use of a competent interpreter, increasing patient risk
- Cultural Beliefs and Traditions Affecting Patient Care
- Cultural beliefs and traditions, such as minimizing reports of pain, deference to authority figures, and gender roles, among others, can influence the medical encounter and compound the risk for LEP patients
Slide 11. Systems and Strategies To Improve Safety for LEP Patients

- Hospitals can engage in a systematic approach to better identify and prevent medical errors and adverse events that occur commonly among LEP patients
- We present five key recommendations that represent the “ideal system,” however, they can be implemented in different phases depending on existing hospital systems and structures
- Foster a Supportive Culture for Safety of Diverse Patient Populations
- Adapt Current Systems to Better Identify Medical Errors among Patients with LEP
- Improve Reporting of Medical Errors for LEP Patients
- Routinely Monitor Patient Safety for LEP Patients
- Address Root Causes to Prevent Medical Errors among LEP Patients
Slide 12. Five Recommendations To Improve Patient Safety

Flow chart illustrating five key recommendations to improve detection of medical errors across diverse populations and prevent high-risk scenarios from becoming safety events. The first recommendation is “Fostering a Supportive Culture for Safety of Diverse Patient Populations,” which includes: Incorporate into mission, messaging, and operations; Engage interdepartmental collaborations; Foster continuous learning. The second recommendation is “Identifying,” which includes: Collect race, ethnicity and language data; Improve Patient Safety systems to capture root causes and risk factors; Link patient safety and registration databases to make information more readily accessible. The third recommendation is “Reporting,” which includes: Develop into strategies to empower staff to report medical errors for limited English proficient patients; Provide staff with training and systems to do so efficiently and effectively. The fourth recommendation is Monitoring. The fifth recommendation is Addressing/Preventing, which encompasses the use of the TEAMSTEPPS module, which has two components: General Strategies and High Risk Scenarios. The High Risk Scenarios consist of the following: Medication Reconciliation, discharge, informed consent, Emergency Department care, and Surgical care. The chart shows how these 5 recommendations interact to support one another. Identify and Reporting leads to improved Monitoring, which leads to Addressing/Preventing, which then leads back to Identifying and Reporting.
Slide 13. Systems and Strategies To Improve Safety for LEP Patients: Culture

- Foster a Supportive Culture for Safety of Diverse Patient Populations
Foster a supportive culture for safety of diverse patient populations, articulated clearly by leadership, operationalized in strategic planning for the organization, and supported by providing staff with key tools and resources to accomplish this successfully
- Link the goal of overcoming language and cultural barriers into the overall message and mission of the culture of quality and safety, and frame this within existing operational policies and standards related to quality and safety for all patients
- Share lessons learned from patient safety events with all staff to: 1) help build an institutional culture sensitive to issues that affect LEP patients, and 2) assure on-going continuous learning and training in this area
- Involve patients in Family Advisory Councils or Cultural Advisory Groups to incorporate patient perspectives
Slide 14. Systems and Strategies To Improve Safety for LEP Patients: Identification

- Adapt Current Systems to Better Identify Medical Errors among Patients with LEP
Adapt current systems to better identify medical errors in patients, improve the capacity of patient safety systems to capture key root causes and risk factors, and link databases so information is readily accessible
- Document data on race, ethnicity, and patient language and interpreter services needs in the electronic medical record to allow for ongoing monitoring and easy integration with other reporting systems for quality of care monitoring purposes
- Include these data fields in patient safety systems to track the role of language and culture in the patient safety events reported by staff
Slide 15. Systems and Strategies To Improve Safety for LEP Patients: Reporting
- Improve Reporting of Medical Errors for LEP Patients
Develop institutional strategies to empower frontline staff and interpreters to report medical errors, and provide them with training and systems to do so effectively and efficiently
- Develop targeted messages so that frontline staff and interpreters are empowered to report any patient safety events they might encounter
- Train all staff, particularly frontline and interpreters, on the full spectrum of what constitutes a patient safety event (including near-misses) and how to report them, and consider other methods of identifying errors outside of standard reporting
- The term “frontline staff” includes all patient-facing staff such as registrars, medical technicians, medical assistants and nurses.
Slide 16. Systems and Strategies To Improve Safety for LEP Patients: Monitor

- Routinely Monitor Patient Safety for LEP Patients
Develop systems to routinely monitor patient safety among LEP patients, as well as processes to analyze medical errors and near misses that occur among these populations
- Develop routine (quarterly, yearly) hospital-wide safety reports or dashboards that focus on patient safety among LEP patients
- Create routine forums for analyzing cases of medical errors and near misses that occur among LEP and culturally diverse populations so as to better understand root causes and high-risk scenarios, and develop strategies for improvement and error prevention
Slide 17. Systems and Strategies To Improve Safety for LEP Patients: Address
- Address Root Causes to Prevent Medical Errors among LEP Patients
Develop strategies and systems to prevent medical errors among LEP patients by strengthening interpreter services and improving coordination with the provision of clinical services, providing translated materials, and developing training for health care providers and staff on interpreter use, cultural competency, and advocacy
- Develop dedicated services for medical interpretation that include either in-person or telephonic qualified medical interpreters, or both
- Provide patients with written materials—such as for informed consent, or procedure preparation—in their own preferred written language
Slide 18. Systems and Strategies To Improve Safety for LEP Patients: Address

- Address Root Causes to Prevent Medical Errors Among LEP Patients
- Create a mechanism to automatically schedule an interpreter at clinical points of service for patients who are identified as having LEP
- Train staff on team communication, the use of interpreter services, cultural competency, and advocacy by using the new TeamSTEPPS® LEP training module
- Fluent bilingual staff may be used as a form of language assistance, but should receive training in basic medical interpretation
Slide 19. Specific Recommendations for High-Risk Scenarios
- Certain high-risk clinical situations need immediate attention to prevent adverse events among LEP patients:
- Medication reconciliation
- Patient discharge
- Informed consent
- Emergency department care
- Surgical care
- Ensuring that resources are available to address these high-risk scenarios should be a priority. Below are three recommendations to address high-risk scenarios:
- Require presence of qualified interpreters
- Provide translated materials in preferred language
- Use “teach back” to confirm patient understanding
Slide 20. Improving Team Communication To Foster Safety for LEP Patients: TeamSTEPPS®

- There are several activities that can be implemented to prevent errors in the short-term—primary among these is the use of TeamSTEPPS
- In November 2006, the Agency for Health Care Research and Quality, in collaboration with the Department of Defense, released Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS™) as the national standard for team training in health care
- TeamSTEPPS is an evidence-based teamwork system aimed at optimizing patient outcomes by improving communication and other teamwork skills among health care professionals
Slide 21. Improving Team Communication To Foster Safety for LEP Patients: TeamSTEPPS®

The TeamSTEPPS LEP module trains interprofessional care teams working together in hospital units to acquire the knowledge, attitudes, and team behaviors needed to reduce the number and severity of patient safety events affecting LEP and culturally diverse patients
http://teamstepps.ahrq.gov — The module is free, publicly accessible, and customizable, and contains the following components: training module, video vignettes, workshop materials, training guide, and evaluation guide and metrics
| TeamSTEPPS® LEP Module Objectives
Participants in the TeamSTEPPS® Module will be able to:
- Identify high-risk situations for LEP and culturally diverse patients
- Assemble the most appropriate and effective care team for LEP patients
- Apply new TeamSTEPPS strategies to enhance the safe of LEP and culturally diverse patients
- Utilize TeamSTEPPS structured communication skills to identify and raise patient communication issues with the care team
|
Slide 22. Summary
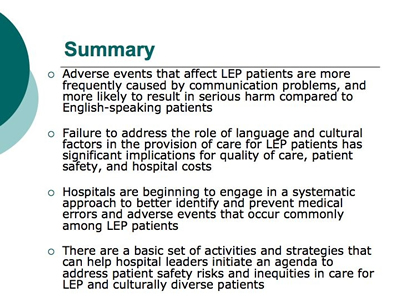
- Adverse events that affect LEP patients are more frequently caused by communication problems, and more likely to result in serious harm compared to English-speaking patients
- Failure to address the role of language and cultural factors in the provision of care for LEP patients has significant implications for quality of care, patient safety, and hospital costs
- Hospitals are beginning to engage in a systematic approach to better identify and prevent medical errors and adverse events that occur commonly among LEP patients
- There are a basic set of activities and strategies that can help hospital leaders initiate an agenda to address patient safety risks and inequities in care for LEP and culturally diverse patients
Slide 23. References

- Institute of Medicine, Committee on Quality of Health Care in America. To err is human: building safer health system. Washington: National Academies Press; 2000.
- Institute of Medicine, Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington: National Academies Press; 2001.
- Divi C, Koss RG, Schmaltz SP, Loeb JM. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. Apr 2007;19(2):60-67. Epub 2007 Feb 2002.
- Cohen AL, Rivara F, Marcuse EK, McPhillips H, Davis R. Are language barriers associated with serious medical events in hospitalized pediatric patients? Pediatrics. Sep 2005;116(3):575-579.
- Flores G, Laws MB, Mayo SJ, et al. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. Jan 2003;111(1):6-14.
- The Joint Commission. Root Causes for Sentinel Events. Available at: http://www.jointcommission.org/assets/1/18/Root_Causes_Event_Type_2004-3Q2011.pdf
 . Accessed October, 2011. . Accessed October, 2011.
- U.S. Census Bureau, 2009. American Community Survey (ACS), data accessed through American Factfinder. Available at: http://factfinder.census.gov/home/saff/main.html?_lang=en.
- John-Baptiste A, Naglie G, Tomlinson G, et al. The effect of English language proficiency on length of stay and in-hospital mortality. J Gen Intern Med. Mar 2004;19(3):221-228.
- Graham CL, Ivey SL, Neuhauser L. From Hospital to Home: Assessing the Transitional Care Needs of Vulnerable Seniors. The Gerontologist. February 1, 2009 2009;49(1):23-33.
- Jiang HJ, Andrews R, Stryer D, Friedman B. Racial/ethnic disparities in potentially preventable readmissions: the case of diabetes. Am J Public Health. Sep 2005;95(9):1561-1567.
- Price-Wise G. Language, Culture, and Medical Tragedy: The Case of Willie Ramirez. Health Affairs Blog. November 19, 2008. Available at: http://healthaffairs.org/blog/2008/11/19/language-culture-and-medical-tragedy-the-case-of-willie-ramirez/
 . .
- Quan K. The High Costs of Language Barriers in Medical Malpractice: University of California, Berkeley. School of Public Health. National Health Law Program; 2010. Available at: http://www.healthlaw.org/images/stories/High_Costs_of_Language_Barriers_in_Malpractice.pdf
 . .
- Carbone E, Gorrie J, Oliver R. Without proper language interpretation, sight is lost in Oregon and a $350,000 verdict is reached. Legal Rev Commentary Suppl Healthcare Risk Manage. 2003(May 1–3).
- 2011 Comprehensive Accreditation Manual for Hospitals: The Official Handbook. Oakbrook Terrace, IL: Joint Commission on Accreditation of Healthcare Organizations; 2010.
Return to Contents
AHRQ Publication No. 12-0041
Current as of September 2012
Internet Citation:
Improving Patient Safety Systems for Patients With Limited English Proficiency: A Guide For Hospitals. AHRQ Publication No. 12-0041, September 2012, Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/populations/lepguide/
|


