What I need to know about Diarrhea
On this page:
- What is diarrhea?
- What causes diarrhea?
- What other symptoms might I have with diarrhea?
- When should I see a health care provider for diarrhea?
- When should I take my child to a health care provider for diarrhea?
- How is the cause of diarrhea diagnosed?
- How is diarrhea treated?
- Can diarrhea be prevented?
- Points to Remember
- Hope through Research
- Pronunciation Guide
- For More Information
- Acknowledgments
What is diarrhea?
Diarrhea is frequent, loose, and watery bowel movements. Bowel movements, also called stools, are body wastes passed through the rectum and anus. Stools contain what is left after your digestive system absorbs nutrients and fluids from what you eat and drink. If your body does not absorb the fluids, or if your digestive system produces extra fluids, stools will be loose and watery. Loose stools contain more water, salts, and minerals and weigh more than solid stools.
Diarrhea that lasts a short time is called acute diarrhea. Acute diarrhea is a common problem and usually lasts only 1 or 2 days, but it may last longer. Diarrhea that lasts for at least 4 weeks is called chronic diarrhea. Chronic diarrhea symptoms may be continual or they may come and go.
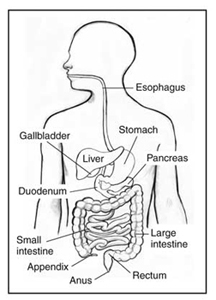
The digestive system
[Top]
What causes diarrhea?
Causes of diarrhea include
- bacteria from contaminated food or water
- viruses that cause illnesses such as the flu
- parasites, which are tiny organisms found in contaminated food or water
- medicines such as antibiotics
- problems digesting certain foods
- diseases that affect the stomach, small intestine, or colon, such as Crohn’s disease
- problems with how the colon functions, caused by disorders such as irritable bowel syndrome
Sometimes no cause can be found. As long as diarrhea goes away within 1 to 2 days, finding the cause is not usually necessary.
[Top]What other symptoms might I have with diarrhea?
In addition to passing frequent, loose stools, other possible symptoms include
- cramps or pain in the abdomen—the area between the chest and hips
- an urgent need to use the bathroom
- loss of bowel control
You may feel sick to your stomach or become dehydrated. If a virus or bacteria is the cause of your diarrhea, you may have fever and chills and bloody stools.
Dehydration
Being dehydrated means your body does not have enough fluid to work properly. Every time you have a bowel movement, you lose fluids. Diarrhea causes you to lose even more fluids. You also lose salts and minerals such as sodium, chloride, and potassium. These salts and minerals affect the amount of water that stays in your body.

Dehydration can be serious, especially for children, older adults, and people with weakened immune systems.
Signs of dehydration in adults are- being thirsty
- urinating less often than usual
- having dark-colored urine
- having dry skin
- feeling tired
- feeling dizzy or fainting
- having a dry mouth and tongue
- crying without tears
- having no wet diapers for 3 hours or more
- having sunken eyes, cheeks, or soft spot in the skull
- having a high fever
- being more cranky or drowsy than usual
Also, when people are dehydrated, their skin does not flatten back to normal right away after being gently pinched and released.
[Top]
When should I see a health care provider for diarrhea?
You should see a health care provider if you have any of the following symptoms:- signs of dehydration
- diarrhea for more than 2 days
- severe pain in your abdomen or rectum
- a fever of 102 degrees or higher
- stools containing blood or pus
- stools that are black and tarry
Diarrhea often goes away by itself, but it may be a sign of a more serious problem.
[Top]When should I take my child to a health care provider for diarrhea?
Take your child to a health care provider right away if your child has any of the following symptoms:
- signs of dehydration
- diarrhea for more than 24 hours
- a fever of 102 degrees or higher
- stools containing blood or pus
- stools that are black and tarry
Children with diarrhea become dehydrated much more easily than adults. Getting treatment quickly is most important if your baby is 6 months old or younger.

[Top]
How is the cause of diarrhea diagnosed?
To find the cause of diarrhea, the health care provider may
- perform a physical exam
- ask about any medicines you are taking
- test your stool or blood to look for bacteria, parasites, or other signs of disease or infection
- ask you to stop eating certain foods to see whether your diarrhea goes away
If you have chronic diarrhea, your health care provider may perform other tests to look for signs of disease.
[Top]
How is diarrhea treated?
Diarrhea is treated by replacing lost fluids, salts, and minerals to prevent dehydration.
Taking medicine to stop diarrhea can be helpful in some cases. Medicines you can buy over the counter without a prescription include loperamide (Imodium) and bismuth subsalicylate (Pepto-Bismol, Kaopectate). Stop taking these medicines if symptoms get worse or if the diarrhea lasts more than 2 days. If you have bloody diarrhea, you should not use over-the-counter diarrhea medicines. These medicines may make diarrhea last longer. The health care provider will usually prescribe antibiotics instead.
Over-the-counter medicines for diarrhea may be dangerous for babies and children. Talk with the health care provider before giving your child these medicines.
Eating, Diet, and Nutrition
To prevent dehydration when you have diarrhea, it is important to drink plenty of water, but you also need to drink fluids that contain sodium, chloride, and potassium.
- Adults should drink water, fruit juices, sports drinks, sodas without caffeine, and salty broths.
- Children should drink oral rehydration solutions—special drinks that contain salts and minerals to prevent dehydration. These drinks include Pedialyte, Naturalyte, Infalyte, and CeraLyte. These drinks are sold in most grocery stores and drugstores.
- bananas
- plain rice
- boiled potatoes
- toast
- crackers
- cooked carrots
- baked chicken without the skin or fat
If a certain food is the cause of diarrhea, try to avoid it.
While you wait for the diarrhea to end, avoid foods that can make it worse:- drinks with caffeine, such as coffee and cola
- high-fat or greasy foods, such as fried foods
- foods with a lot of fiber, such as citrus fruits
- sweet foods, such as cakes and cookies
During or after an episode of diarrhea, some people have trouble digesting lactose, the sugar in milk and milk products. However, you may be able to digest yogurt. Eating yogurt with active, live bacterial cultures may even help you feel better faster.
When babies have diarrhea, continue breastfeeding or formula feeding as usual.
After you have had diarrhea caused by a virus, problems digesting lactose may last up to 4 to 6 weeks. You may have diarrhea for a short time after you eat or drink milk or milk products.

[Top]
Can diarrhea be prevented?
Two types of diarrhea can be prevented—rotavirus diarrhea and traveler’s diarrhea.
Rotavirus Diarrhea
Two vaccines, RotaTeq and Rotarix, protect against rotavirus—a common virus that causes diarrhea in babies and children. RotaTeq is given to babies in three doses at 2, 4, and 6 months of age. Rotarix is given in two doses. The first dose is given when the baby is 6 weeks old, and the second is given at least 4 weeks later but before the baby is 24 weeks old. To learn more about rotavirus vaccines, talk with your child’s health care provider. You can also find more information at the Centers for Disease Control and Prevention rotavirus vaccination webpage at www.cdc.gov/vaccines/vpd-vac/rotavirus.
RotaTeq and Rotarix only prevent diarrhea caused by rotavirus. Children who have been vaccinated may still get diarrhea from another cause.
Traveler’s Diarrhea
People may develop traveler’s diarrhea while visiting developing areas of the world such as Latin America, Africa, and southern Asia. Traveler’s diarrhea is caused by eating food or drinking water that contains harmful bacteria, viruses, or parasites.
You can prevent traveler’s diarrhea by being careful:- Do not drink tap water, use tap water to brush your teeth, or use ice cubes made from tap water.
- Do not eat or drink unpasteurized milk or milk products.
- Do not eat raw fruits and vegetables unless they can be peeled and you peel them yourself.
- Do not eat raw or rare meat and fish.
- Do not eat meat or shellfish that is not hot when served to you.
- Do not eat food sold by street vendors.
You can drink bottled water, carbonated soft drinks, and hot drinks such as coffee and tea.
Before traveling outside the United States, talk with your health care provider. Your health care provider may suggest taking medicine with you. In some cases, taking antibiotics before traveling can help prevent traveler’s diarrhea. And early treatment with antibiotics can shorten an episode of traveler’s diarrhea.
[Top]Points to Remember
- Diarrhea is frequent, loose, and watery bowel movements.
- Acute diarrhea is a common problem. It usually lasts only 1 or 2 days, but it may last longer.
- Being dehydrated means your body does not have enough fluid to work properly. Dehydration can be serious, especially for children, older adults, and people with weakened immune systems.
- Diarrhea is treated by replacing lost fluids, salts, and minerals.
- See your health care provider if you have signs of dehydration, diarrhea for more than 2 days, severe pain in your abdomen or rectum, a fever of 102 degrees or higher, stools containing blood or pus, or stools that are black and tarry.
- Take your child to a health care provider right away if your child has signs of dehydration, diarrhea for more than 24 hours, a fever of 102 degrees or higher, stools containing blood or pus, or stools that are black and tarry.
- Two types of diarrhea can be prevented— rotavirus diarrhea and traveler’s diarrhea.
[Top]
Hope through Research
The Division of Digestive Diseases and Nutrition at the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) supports research on conditions such as diarrhea. Researchers are studying the causes of diarrhea and finding new ways to prevent and treat this condition.
Participants in clinical trials can play a more active role in their own health care, gain access to new research treatments before they are widely available, and help others by contributing to medical research. For information about current studies, visit www.ClinicalTrials.gov.
[Top]Pronunciation Guide
abdomen (AB-doh-men)
antibiotics (AN-tee-by-OT-iks)
anus (AY-nuhss)
bacteria (bak-TIHR-EE-uh)
chloride (KLOR-eyed)
colon (KOH-lon)
dehydrated (dee-HY-dray-ted)
diarrhea (DY-uh-REE-uh)
intestine (in-TESS-tin)
parasites (PAIR-uh-syts)
potassium (poh-TASS-ee-uhm)
rectum (REK-tuhm)
rotavirus (ROH-tuh-VY-ruhs)
sodium (SOH-dee-uhm)
unpasteurized (uhn-PASS-tyoor-eyezd)
vaccines (vak-SEENZ)
viruses (VY-ruhss-ez)
[Top]For More Information
American College of Gastroenterology
P.O. Box 342260
Bethesda, MD 20827–2260
Phone: 301–263–9000
Internet: www.acg.gi.org ![]()
Centers for Disease Control and Prevention
1600 Clifton Road
Atlanta, GA 30333
Phone: 1–800–311–3435 or 404–498–1515
Internet: www.cdc.gov
International Foundation for Functional Gastrointestinal Disorders
P.O. Box 170864
Milwaukee, WI 53217–8076
Phone: 1–888–964–2001 or 414–964–1799
Fax: 414–964–7176
Email: iffgd@iffgd.org
Internet: www.iffgd.org ![]()
North American Society for Pediatric Gastroenterology, Hepatology and Nutrition
P.O. Box 6
Flourtown, PA 19031
Phone: 215–233–0808
Fax: 215–233–3918
Email: naspghan@naspghan.org
Internet: www.naspghan.org ![]()
Acknowledgments
The National Digestive Diseases Information Clearinghouse (NDDIC) would like to thank the following individuals for assisting with scientific and editorial review of this publication.
Mark Donowitz, M.D.
Johns Hopkins University School of Medicine
John S. Fordtran, M.D.
Baylor University Medical College
Thanks also to Joe Surratt at the Digestive Center of Excellence, University of Virginia, Charlottesville, for facilitating field-testing of the original version of this publication.
[Top]
National Digestive Diseases Information Clearinghouse
2 Information Way
Bethesda, MD 20892–3570
Phone: 1–800–891–5389
TTY: 1–866–569–1162
Fax: 703–738–4929
Email: nddic@info.niddk.nih.gov
Internet: www.digestive.niddk.nih.gov
The National Digestive Diseases Information Clearinghouse (NDDIC) is a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The NIDDK is part of the National Institutes of Health of the U.S. Department of Health and Human Services. Established in 1980, the Clearinghouse provides information about digestive diseases to people with digestive disorders and to their families, health care professionals, and the public. The NDDIC answers inquiries, develops and distributes publications, and works closely with professional and patient organizations and Government agencies to coordinate resources about digestive diseases.
This publication is not copyrighted. The Clearinghouse encourages users of this publication to duplicate and distribute as many copies as desired.
This publication may contain information about medications. When prepared, this publication included the most current information available. For updates or for questions about any medications, contact the U.S. Food and Drug Administration toll-free at 1–888–INFO–FDA (1–888–463–6332) or visit www.fda.gov. Consult your health care provider for more information.
NIH Publication No. 11–5176
April 2011
Page last updated April 30, 2012