General Information About Chronic Lymphocytic Leukemia
Key Points for This Section
- Chronic lymphocytic leukemia is a type of cancer in which the bone marrow makes too many lymphocytes (a type of white blood cell).
- Older age can affect the risk of developing chronic lymphocytic leukemia.
- Possible signs of chronic lymphocytic leukemia include swollen lymph nodes and tiredness.
- Tests that examine the blood, bone marrow, and lymph nodes are used to detect (find) and diagnose chronic lymphocytic leukemia.
- Certain factors affect treatment options and prognosis (chance of recovery).
Chronic lymphocytic leukemia is a type of cancer in which the bone marrow makes too many lymphocytes (a type of white blood cell).
Chronic lymphocytic leukemia (also called CLL) is a blood and bone marrow disease that usually gets worse slowly. CLL is the second most common type of leukemia in adults. It often occurs during or after middle age; it rarely occurs in children.
Normally, the body makes blood stem cells (immature cells) that become mature blood cells over time. A blood stem cell may become a myeloid stem cell or a lymphoid stem cell.
A myeloid stem cell becomes one of three types of mature blood cells:
- Red blood cells that carry oxygen and other substances to all tissues of the body.
- White blood cells that fight infection and disease.
- Platelets that form blood clots to stop bleeding.
A lymphoid stem cell becomes a lymphoblast cell and then one of three types of lymphocytes (white blood cells):
- B lymphocytes that make antibodies to help fight infection.
- T lymphocytes that help B lymphocytes make antibodies to fight infection.
- Natural killer cells that attack cancer cells and viruses.
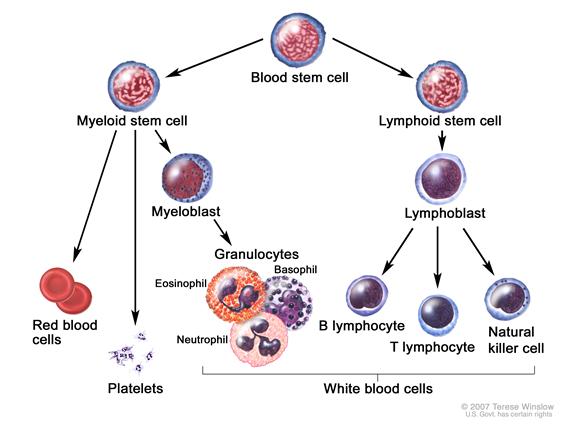
In CLL, too many blood stem cells become abnormal lymphocytes and do not become healthy white blood cells. The abnormal lymphocytes may also be called leukemia cells. The lymphocytes are not able to fight infection very well. Also, as the number of lymphocytes increases in the blood and bone marrow, there is less room for healthy white blood cells, red blood cells, and platelets. This may cause infection, anemia, and easy bleeding.
This summary is about chronic lymphocytic leukemia. See the following PDQ summaries for more information about leukemia:
- Adult Acute Lymphoblastic Leukemia Treatment.
- Childhood Acute Lymphoblastic Leukemia Treatment.
- Adult Acute Myeloid Leukemia Treatment.
- Childhood Acute Myeloid Leukemia/Other Myeloid Malignancies Treatment.
- Chronic Myelogenous Leukemia Treatment.
- Hairy Cell Leukemia Treatment
- Adult Non-Hodgkin Lymphoma Treatment
Older age can affect the risk of developing chronic lymphocytic leukemia.
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn’t mean that you will not get cancer. Talk with your doctor if you think you may be at risk. Risk factors for CLL include the following:
- Being middle-aged or older, male, or white.
- A family history of CLL or cancer of the lymph system.
- Having relatives who are Russian Jews or Eastern European Jews.
Possible signs of chronic lymphocytic leukemia include swollen lymph nodes and tiredness.
Usually CLL does not cause any symptoms and is found during a routine blood test. Sometimes symptoms occur that may be caused by CLL or by other conditions. Check with your doctor if you have any of the following problems:
- Painless swelling of the lymph nodes in the neck, underarm, stomach, or groin.
- Feeling very tired.
- Pain or fullness below the ribs.
- Fever and infection.
- Weight loss for no known reason.
Tests that examine the blood, bone marrow, and lymph nodes are used to detect (find) and diagnose chronic lymphocytic leukemia.
The following tests and procedures may be used:
- Physical exam and history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
- Complete blood count (CBC) with differential: A procedure in which a sample of blood is drawn and checked for the following:
- The number of red blood cells and platelets.
- The number and type of white blood cells.
- The amount of hemoglobin (the protein that carries oxygen) in the red blood cells.
- The portion of the blood sample made up of red blood cells.
Enlarge
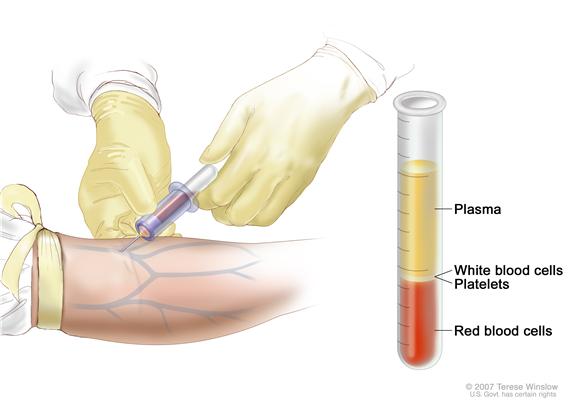 Complete blood count (CBC). Blood is collected by inserting a needle into a vein and allowing the blood to flow into a tube. The blood sample is sent to the laboratory and the red blood cells, white blood cells, and platelets are counted. The CBC is used to test for, diagnose, and monitor many different conditions.
Complete blood count (CBC). Blood is collected by inserting a needle into a vein and allowing the blood to flow into a tube. The blood sample is sent to the laboratory and the red blood cells, white blood cells, and platelets are counted. The CBC is used to test for, diagnose, and monitor many different conditions. - Immunophenotyping: A test in which the cells in a sample of blood or bone marrow are looked at under a microscope to find out if malignant lymphocytes (cancer) began from the B lymphocytes or the T lymphocytes.
- FISH (fluorescence in situ hybridization): A laboratory technique used to look at genes or chromosomes in cells and tissues. Pieces of DNA that contain a fluorescent dye are made in the laboratory and added to cells or tissues on a glass slide. When these pieces of DNA bind to specific genes or areas of chromosomes on the slide, they light up when viewed under a microscope with a special light.
- Flow cytometry: A laboratory test that measures the number of cells in a sample, the percentage of live cells in a sample, and certain characteristics of cells, such as size, shape, and the presence of tumor markers on the cell surface. The cells are stained with a light-sensitive dye, placed in a fluid, and passed in a stream before a laser or other type of light. The measurements are based on how the light-sensitive dye reacts to the light.
- IgVH gene mutation test: A laboratory test done on a bone marrow or blood sample to check for an IgVH gene mutation. Patients with an IgVH gene mutation have a better prognosis.
- Bone marrow aspiration and biopsy: The removal of bone marrow, blood, and a small piece of bone by inserting a hollow needle into the hipbone or breastbone. A pathologist views the bone marrow, blood, and bone under a microscope to look for abnormal cells.Enlarge
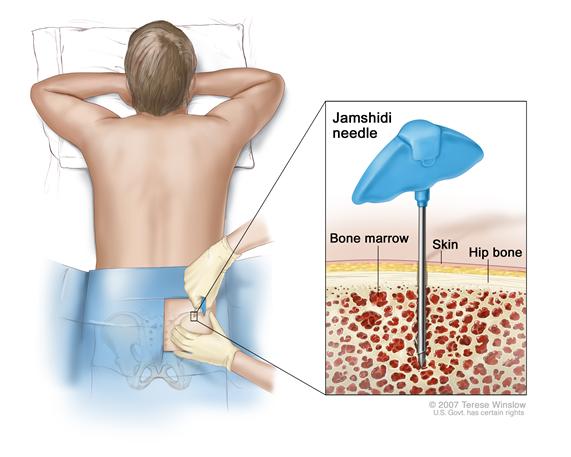 Bone marrow aspiration and biopsy. After a small area of skin is numbed, a Jamshidi needle (a long, hollow needle) is inserted into the patient’s hip bone. Samples of blood, bone, and bone marrow are removed for examination under a microscope.
Bone marrow aspiration and biopsy. After a small area of skin is numbed, a Jamshidi needle (a long, hollow needle) is inserted into the patient’s hip bone. Samples of blood, bone, and bone marrow are removed for examination under a microscope.
Certain factors affect treatment options and prognosis (chance of recovery).
Treatment options depend on:
- The stage of the disease.
- Red blood cell, white blood cell, and platelet blood counts.
- Whether there are symptoms, such as fever, chills, or weight loss.
- Whether the liver, spleen, or lymph nodes are larger than normal.
- The response to initial treatment.
- Whether the CLL has recurred (come back).
The prognosis (chance of recovery) depends on:
- Whether there is a change in the DNA and the type of change, if there is one.
- Whether lymphocytes are spread throughout the bone marrow.
- The stage of the disease.
- Whether the CLL gets better with treatment or has recurred (come back).
- Whether the CLL progresses to lymphoma or prolymphocytic leukemia.
- The patient's general health.


 Back to Top
Back to Top