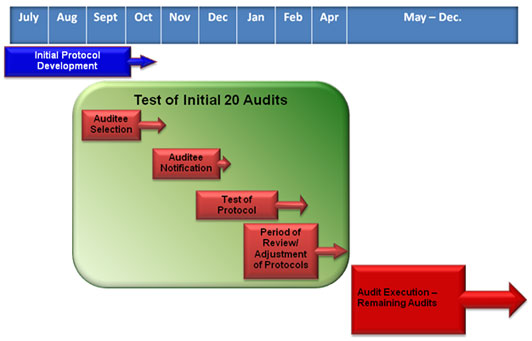
| Audit Pilot ProgramProgram Objectives: The audit program serves as a new part of OCR’s health information privacy and security compliance program. OCR will use the audit program to assess HIPAA compliance efforts by a range of covered entities, Audits present a new opportunity to examine mechanisms for compliance, identify best practices and discover risks and vulnerabilities that may not have come to light through OCR’s ongoing complaint investigations and compliance reviews. OCR will broadly share best practices gleaned through the audit process and guidance targeted to observed compliance challenges via this web site and other outreach portals. When Will Audits Begin? The pilot audit program is a three step process. The first step entailed developing the audit protocols. Next, a limited number of audits will be conducted in an initial wave to test these protocols. OCR expects the initial audits to begin in November 2011.The results of the initial audits will inform how the rest of the audits will be conducted. The last step will include conducting the full range of audits using revised protocol materials. All audits in this pilot will be completed by the end of December, 2012. 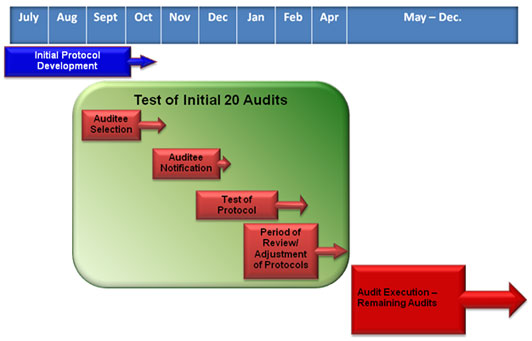 Hide Details Who Will Be Audited? Every covered entity and business associate is eligible for an audit. Selections in the initial round will be designed to provide a broad assessment of a complex and diverse health care industry. OCR is responsible for selection of the entities that will be audited. OCR will audit as wide a range of types and sizes of covered entities as possible; covered individual and organizational providers of health services, health plans of all sizes and functions, and health care clearinghouses may all be considered for an audit. We expect covered entities to provide the auditors their full cooperation and support and remind them of their cooperation obligations under the HIPAA Enforcement Rule. Business Associates will be included in future audits. Hide Details How Will the Audit Program Work? The privacy and security performance audit process will include generally familiar audit mechanisms. Entities selected for an audit will be informed by OCR of their selection and asked to provide documentation of their privacy and security compliance efforts. In this pilot phase, every audit will include a site visit and result in an audit report. During site visits, auditors will interview key personnel and observe processes and operations to help determine compliance. Following the site visit, auditors will develop and share with the entity a draft report; audit reports generally describe how the audit was conducted, what the findings were and what actions the covered entity is taking in response to those findings. Prior to finalizing the report, the covered entity will have the opportunity to discuss concerns and describe corrective actions implemented to address concerns identified. The final report submitted to OCR will incorporate the steps the entity has taken to resolve any compliance issues identified by the audit, as well as describe any best practices of the entity. 
References to days are in business days.
Hide Details What is the General Timeline for an Audit? When a covered entity is selected for an audit, OCR will notify the covered entity in writing. The OCR notification letter will introduce the audit contractor, explain the audit process and expectations in more detail, and describe initial document and information requests. It will also specify how and when to return the requested information to the auditor. OCR expects covered entities and business associates who are the subject of the audit to provide requested information within 10 business days of the request for information. OCR expects to notify selected covered entities between 30 and 90 days prior to the anticipated onsite visit. Onsite visits may take between 3 and 10 business days depending upon the complexity of the organization and the auditor’s need to access materials and staff. After fieldwork is completed, the auditor will provide the covered entity with a draft final report; a covered entity will have 10 business days to review and provide written comments back to the auditor. The auditor will complete a final audit report within 30 business days after the covered entity’s response and submit it to OCR. Hide Details What Happens After an Audit? Audits are primarily a compliance improvement activity. OCR will review the final reports, including the findings and actions taken by the audited entity to address findings. The aggregated results of the audits will enable OCR to better understand compliance efforts with particular aspects of the HIPAA Rules. Generally, OCR will use the audit reports to determine what types of technical assistance should be developed, and what types of corrective action are most effective. Should an audit report indicate a serious compliance issue, OCR may initiate a compliance review to address the problem. OCR will not post a listing of audited entities or the findings of an individual audit which clearly identifies the audited entity. Hide Details How will Consumers Be Affected? The audit program represents one more avenue by which OCR ensures compliance with HIPAA protections of health information to the benefit of consumers. For example, the audit program may uncover reasons many health information breaches are occurring and help OCR create tools for covered entities to better protect individually identifiable health information. Concerns about compliance identified and corrected by an audit will serve to improve the privacy and security of health records. The technical assistance and best practices that OCR generates will also assist covered entities and business associates in improving their efforts to keep health records safe and secure. OCR continues to accept complaints from individuals and covered entities continue to have the obligation to accept complaints from persons about their HIPAA Rule activities. Hide Details Will audits differ depending on the size and type of covered entity? The audit protocol is designed to work with a broad range of covered entities. The audit procedures vary depending on the size and complexity of the entity being audited. Hide Details Will auditors be looking at state specific privacy and security rules in addition to HIPAA's Privacy, Security and Breach Notification Rules? No, the scope of the audit program does not extend beyond the Privacy, Security, and Breach Notification Rules. Hide Details
Who is responsible for paying the on-site auditors? The Department has entered into a contract with the audit contractor to conduct the audits on its behalf. Covered entities are not responsible for remuneration of the auditing firm. Hide Details
Auditee Selection | | For this pilot phase of the audit program, OCR identified a pool of covered entities for audits that broadly represent the wide range of healthcare providers, health plans and healthcare clearinghouses operating today. Using this spectrum of audit candidates permits OCR to assess HIPAA compliance in a variety of entities with unique operating environments and relationships with patients. Among the specific criteria used to select particular candidates are whether the entity is public or private, the size of an entity, affiliation with other healthcare organizations, the type of entity and relationship to patient care, and past and present interaction with OCR concerning HIPAA enforcement and breach notification. OCR also considers geographic factors in the selection process. Entities that received notification letters |
|
|