Breast and Lymphatic System Basics
Check With Your Health Care Provider About Breast Changes
Breast Changes During Your Lifetime That Are Not Cancer
Finding Breast Changes
Getting Your Mammogram Results
Follow-up Tests to Diagnose Breast Changes
Breast Changes and Conditions: Getting Follow-up Test Results
Getting the Support You Need
Breast Conditions and Follow-Up Care
Resources to Learn More
Introduction
You may be reading this booklet because you, or your health care provider, found a breast lump or other breast change. Keep in mind that breast changes are very common. Most breast changes are not cancer. But it is very important to get the follow-up tests that your health care provider asks you to.
What are breast changes?
Many breast changes are changes in how your breast or nipple looks or feels. You may notice a lump or firmness in your breast or under your arm. Or perhaps the size or shape of your breast has changed. Your nipple may be pointing or facing inward (inverted) or feeling tender. The skin on your breast, areola, or nipple may be scaly, red, or swollen. You may have nipple discharge, which is an abnormal fluid coming from the nipple.
If you have these or other breast changes, talk with your health care provider to get these changes checked as soon as possible.
This booklet can help you take these steps:
- Call your health care provider to make an appointment as soon as you notice any breast changes.
- Go back to see your health care provider if your mammogram result is abnormal.
- Get all of the follow-up tests and care that your health care provider asks you to.
It may be helpful to bring this booklet with you. It discusses breast changes that are not cancer (benign), as well as changes that are abnormal or could be signs of cancer. Feel free to read different sections in this booklet as you need them.
To order free copies of this booklet, call the National Cancer Institute (NCI) at 1-800-4-CANCER (1-800-422-6237) or click here to get free copies sent to you.
Breast and Lymphatic System Basics
To better understand breast changes, it helps to know what the breasts and lymphatic system are made of.
What are breasts made of?
Breasts are made of connective tissue, glandular tissue, and fatty tissue. Connective tissue and glandular tissue look dense, or white on a mammogram. Fatty tissue is non-dense, or black on a mammogram. Dense breasts can make mammograms harder to interpret.
Breasts have lobes, lobules, ducts, an areola, and a nipple.
- Lobes are sections of the glandular tissue. Lobes have smaller sections called lobules that end in tiny bulbs that can make milk.
- Ducts are thin tubes that connect the lobes and lobules. Milk flows from the lobules through the ducts to the nipple.
- The nipple is the small raised area at the tip of the breast. Milk flows through the nipple. The areola is the area of darker-colored skin around the nipple. Each breast also has lymph vessels.
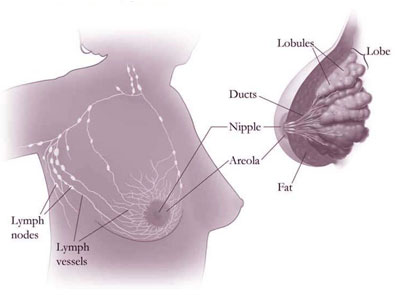
What is the lymphatic system made of?
The lymphatic system, which is a part of your body's defense system, contains lymph vessels and lymph nodes.
- Lymph vessels are thin tubes that carry a fluid called lymph and white blood cells.
- Lymph vessels lead to small, bean-shaped organs called lymph nodes. Lymph nodes are found near your breast, under your arm, above your collarbone, in your chest, and in other parts of your body.
- Lymph nodes filter substances in lymph to help fight infection and disease. They also store disease-fighting white blood cells called lymphocytes.
Check With Your Health Care Provider About Breast Changes
Check with your health care provider if you notice that your breast looks or feels different. No change is too small to ask about. In fact, the best time to call is when you first notice a breast change.
Breast changes to see your health care provider about:
A lump (mass) or a firm feeling
- A lump in or near your breast or under your arm
- Thick or firm tissue in or near your breast or under your arm
- A change in the size or shape of your breast
Lumps come in different shapes and sizes. Most lumps are not cancer.
If you notice a lump in one breast, check your other breast. If both breasts feel the same, it may be normal. Normal breast tissue can sometimes feel lumpy.
Some women do regular breast self-exams (BSE). Doing a BSE regularly can help you learn how your breast normally feels and make it easier to notice and find any changes.
Remember—doing a BSE regularly is not a substitute for regular mammograms.
| Always get a lump checked. Don't wait until your next mammogram. You may need to have tests to be sure that the lump is not cancer. |
Nipple discharge or changes
- Nipple discharge (fluid that is not breast milk)
- Nipple changes, such as a nipple that points or faces inward (inverted) into the breast
Nipple discharge may be different colors or textures. Nipple discharge is not usually a sign of cancer. It can be caused by birth control pills, some medicines, and infections.
| Get nipple discharge checked, especially fluid that comes out by itself or fluid that is bloody. |
Skin changes
- Itching, redness, scaling, dimples, or puckers on your breast
| If the skin on your breast changes, get it checked as soon as possible. |
|
Talk with your health care provider.
To get the most from your visit, talk with your health care provider about any breast changes you notice, as well as your personal medical history and your family medical history.
Tell your health care provider about breast changes or problems:
- These are the breast changes or problems I have noticed: ________________________________
- This is what the breast change looks or feels like: (For example: Is the lump hard or soft? Does your breast feel tender or swollen? How big is the lump? What color is the nipple discharge?) ______________________________________________________________________________
- This is where the breast change is: (For example: What part of the breast feels different? Do both breasts feel different or only one breast?) _____________________________________________
- This is when I first noticed the breast change: __________________________________________
- Since then, this is the change I've noticed: (For example: Has it stayed the same or gotten worse?) ______________________________________________________________________________
Share your personal medical history:
- I've had these breast problems in the past: ____________________________________________
- These are the breast exams and tests that I have had: ___________________________________
- My last mammogram was on this date: _______________________________________________
- My last menstrual period began on this date: ___________________________________________
- These are the medicines or herbs that I take: __________________________________________
- Right now, I:
- Have breast implants
- Am pregnant
- Am breastfeeding
- I've had this type of cancer before: ___________________________________________________
Share your family medical history:
- My family members have had these breast problems or diseases: __________________________
- These family members had breast cancer: ____________________________________________
- They were this old when they had breast cancer: ________________________________________
For a printable checklist, please see page 6 of the Understanding Breast Changes: A Health Guide for Women pdf.
Breast Changes During Your Lifetime That Are Not Cancer
Most women have changes in their breasts during their lifetime. Many of these changes are caused by hormones. For example, your breasts may feel more lumpy or tender at different times in your menstrual cycle.
Other breast changes can be caused by the normal aging process. As you near menopause, your breasts may lose tissue and fat. They may become smaller and feel lumpy. Most of these changes are not cancer; they are called benign changes. However, if you notice a breast change, don't wait until your next mammogram. Make an appointment to get it checked.
Young women who have not gone through menopause often have more dense tissue in their breasts. Dense tissue has more glandular and connective tissue and less fat tissue. This kind of tissue makes mammograms harder to interpret--because both dense tissue and tumors show up as solid white areas on x-ray images. Breast tissue gets less dense as women get older.
Before or during your menstrual periods, your breasts may feel swollen, tender, or painful. You may also feel one or more lumps during this time because of extra fluid in your breasts. These changes usually go away by the end of your menstrual cycle. Because some lumps are caused by normal hormone changes, your health care provider may have you come back for a return visit, at a different time in your menstrual cycle.
During pregnancy, your breasts may feel lumpy. This is usually because the glands that produce milk are increasing in number and getting larger.
While breastfeeding, you may get a condition called mastitis. This happens when a milk duct becomes blocked. Mastitis causes the breast to look red and feel lumpy, warm, and tender. It may be caused by an infection and it is often treated with antibiotics. Sometimes the duct may need to be drained. If the redness or mastitis does not go away with treatment, call your health care provider.
As you approach menopause, your menstrual periods may come less often. Your hormone levels also change. This can make your breasts feel tender, even when you are not having your menstrual period. Your breasts may also feel more lumpy than they did before.
If you are taking hormones (such as menopausal hormone therapy, birth control pills, or injections) your breasts may become more dense. This can make a mammogram harder to interpret. Be sure to let your health care provider know if you are taking hormones.
When you stop having menstrual periods (menopause), your hormone levels drop, and your breast tissue becomes less dense and more fatty. You may stop having any lumps, pain, or nipple discharge that you used to have. And because your breast tissue is less dense, mammograms may be easier to interpret.
|
Finding Breast Changes
Here are some ways your health care provider can find breast changes:
Clinical breast exam
During a clinical breast exam, your health care provider checks your breasts and nipples and under your arms for any abnormal changes. This exam is part of a routine check-up.
Mammogram

A mammogram is an x-ray picture of your breast tissue. This test may find tumors that are too small to feel. During a mammogram, each breast is pressed between two plastic plates. Some discomfort is normal, but if it's painful, tell the mammography technician.
The best time to get a mammogram is at the end of your menstrual period. This is when your breasts are less tender. Some women have less breast tenderness if they don't have any caffeine for a couple of days before the mammogram.
After the x-ray pictures are taken, they are sent to a radiologist, who studies them and sends a report to your health care provider.
Both film and digital mammography use x-rays to make a picture of the breast tissue. The actual procedure for getting the mammogram is the same. The difference is in how the images are recorded and stored. It's like the difference between a film camera and a digital camera.
- Film mammography stores the image directly on x-ray film.
- Digital mammography takes an electronic image of the breast and stores it directly in a computer. Digital images can be made lighter, darker, or larger. Images can also be stored and shared electronically.
A research study sponsored by the National Cancer Institute (NCI) showed that digital mammography and film mammography are about the same in terms of detecting breast cancer. However, digital mammography may be better at detecting breast cancer in woman who are under age 50, have very dense breasts, or are premenopausal or perimenopausal (the times before and at the beginning of menopause).
Talk with your health care provider to learn more about what is best for you.
| Mammograms are tests to check for breast changes that are often too small for you or your doctor to feel. Getting mammograms on a regular basis is the best way to find breast cancer early in most women. Talk with your health care provider about how often to get mammograms. |
| Mammograms are used for both screening and diagnosis. |
|---|
|
| Talk with the women in your life. Let them know that mammograms save lives. Take time to care for yourself and those who need you. |
|
| Mammograms and breast implants |
|---|
When you make your appointment, be sure to tell the staff if you have breast implants. Ask if they have specialists who are trained in taking and reading mammograms of women with breast implants. This is important because breast implants can make it harder to see cancer or other abnormal changes on the mammogram. A special technique called implant displacement views is used.
|
MRI
Magnetic resonance imaging, also called MRI, uses a powerful magnet, radio waves, and a computer to take detailed pictures of areas inside the breast. MRI is another tool that can be used to find breast cancer. However, MRIs don't replace mammograms. They are used in addition to mammograms in women who are at increased risk of breast cancer.
MRIs have some limits. For example, they cannot find breast changes such as microcalcifications. MRIs are also less specific than other tests. This means that they may give false-positive test results—the test shows that there is cancer when there really is not.
Talk with your health care provider about having other screening tests, such as an MRI, in addition to mammograms. Ask your health care provider if you are at increased risk of breast cancer due to:
Getting Your Mammogram Results
You should get a written report of your mammogram results within 30 days of your mammogram, since this is the law. Be sure the mammography facility has your address and phone number. It's helpful to get your mammogram at the same place each year. This way, your current mammogram can be compared with past mammograms.
If your results were normal:
- Your breast tissue shows no signs of a mass or calcification.
- Visit your health care provider if you notice a breast change before your next appointment.
If your results were abnormal:
- A breast change was found. It may be benign (not cancer), premalignant (may become cancer), or cancer.
- It's important to get all the follow-up tests your health care provider asks you to.
If you don't get your results, call your health care provider.
Keep in mind that most breast changes are not cancer. But all changes need to be checked, and more tests may be needed.
|
What can a mammogram show?

Mammograms can show lumps, calcifications, and other changes in your breast. The radiologist will study the mammogram for breast changes that do not look normal and for differences between your breasts. When possible, he or she will compare your most recent mammogram with past mammograms to check for changes.
Lump (or mass)
The size, shape, and edges of a lump give the radiologist important information. A lump that is not cancer often looks smooth and round and has a clear, defined edge. Lumps that look like this are often cysts. See Breast Changes and Conditions: Getting Follow-up Test Results for more information about cysts. However, if the lump on the mammogram has a jagged outline and an irregular shape, more tests are needed.
Depending on the size and shape of the lump, your health care provider may ask you to have:
- Another clinical breast exam
- Another mammogram to have a closer look at the area
- An ultrasound exam to find out if the lump is solid or is filled with fluid
- A test called a biopsy to remove cells, or the entire lump, to look at under a microscope to check for signs of disease
Calcifications
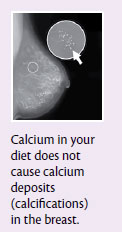
Calcifications are deposits of calcium in the breast tissue. They are too small to be felt, but can be seen on a mammogram. There are two types:
- Macrocalcifications look like small white dots on a mammogram. They are common in women over 50 years old. Macrocalcifications are not related to cancer and usually don't need more testing.
- Microcalcifications look like tiny white specks on a mammogram. They are usually not a sign of cancer. However, if they are found in an area of rapidly dividing cells, or grouped together in a certain way, you may need more tests.
Depending on how many calcifications you have, their size, and where they are found, your health care provider may ask you to have:
- Another mammogram to have a closer look at the area
- A test called a biopsy to check for signs of disease
Are mammogram results always right?
Mammography is an excellent tool to find breast changes in most women who have no signs of breast cancer. However, it may not detect all breast cancers. See your health care provider if you have a lump that was not seen on a mammogram or notice any other breast changes.
|
Follow-up Tests to Diagnose Breast Changes
An ultrasound exam, an MRI, a biopsy, or other follow-up tests may be needed to learn more about a breast change.
|
Ultrasound
An ultrasound exam uses sound waves to make a picture of breast tissue. This picture is called a sonogram. It helps radiologists to see if a lump or mass is solid or filled with fluid. A fluid-filled lump is called a cyst.
MRI
Magnetic resonance imaging, also called MRI, uses a powerful magnet, radio waves, and a computer to take detailed pictures of areas inside the breast. Sometimes breast lumps or large lymph nodes are found during a clinical breast exam or breast self-exam that were not seen on a mammogram or ultrasound. In these cases, an MRI can be used to learn more about these changes.
Breast biopsy
A breast biopsy is a procedure to remove a sample of breast cells or tissue, or an entire lump. A pathologist then looks at the sample under a microscope to check for signs of disease. A biopsy is the only way to find out if cells are cancer.
Biopsies are usually done in an office or a clinic on an outpatient basis. This means you will go home the same day as the procedure. Local anesthesia is used for some biopsies. This means you will be awake, but you won't feel pain in your breast during the procedure. General anesthesia is often used for a surgical biopsy. This means that you will be asleep and won't wake up during the procedure.
Common types of breast biopsies:
- Fine-needle aspiration biopsy
A fine-needle aspiration biopsy is a simple procedure that takes only a few minutes. Your health care provider inserts a thin needle into the breast to take out fluid and cells. - Core biopsy
A core biopsy, also called a core needle biopsy, uses a needle to remove small pieces or cores of breast tissue. The samples are about the size of a grain of rice. You may have a bruise, but usually not a scar. - Vacuum-assisted biopsy
A vacuum-assisted biopsy uses a probe, connected to a vacuum device, to remove a small sample of breast tissue. The small cut made in the breast is much smaller than with surgical biopsy. This procedure causes very little scarring, and no stitches are needed.
| Your doctor may use ultrasound or mammography during a breast biopsy to help locate the breast change. |
- Surgical biopsy
A surgical biopsy is an operation to remove part, or all, of a lump so it can be looked at under a microscope to check for signs of disease. Sometimes a doctor will do a surgical biopsy as the first step. Other times, a doctor may do a surgical biopsy if the results of a needle biopsy do not give enough information.
When only a sample of breast tissue is removed, it's called an incisional biopsy. When the entire lump or suspicious area is removed, it's called an excisional biopsy.
If the breast change cannot be felt, wire localization, also called needle localization, may be used to find the breast change. During wire localization, a thin, hollow needle is inserted into the breast. A mammogram is taken to make sure that the needle is in the right place. Then a fine wire is inserted through the hollow needle, to mark the area of tissue to be removed. Next, the needle is removed, and another mammogram is taken. You then go to the operating room where the surgeon removes the wire and surrounding breast tissue. The tissue is sent to the lab to be checked for signs of disease.
|
Questions to ask if a biopsy is recommended:
- Why is a biopsy needed? What will it tell us? ___________________________________________
- What type of biopsy will I have? How will the biopsy be done? ______________________________
- Where will the biopsy be done? How long will it take? ____________________________________
- Will it hurt? _____________________________________________________________________
- How much breast tissue will be removed?_____________________________________________
- Will I be awake? ________________________________________________________________
- What tests will be done on the breast tissue? __________________________________________
- When will I know the results?_______________________________________________________
- Will there be side effects? _________________________________________________________
- How should I care for the biopsy site? ________________________________________________
- Will I need to rest after the biopsy? __________________________________________________
Questions to ask about your biopsy results:
- What were the results of the biopsy? _________________________________________________
- What do the biopsy results mean? __________________________________________________
- What are the next steps? Do I need more tests? ________________________________________
- Who should I talk with next? ________________________________________________________
- Do I have an increased risk of breast cancer? __________________________________________
- Who can give me a second opinion on my biopsy results? ________________________________
For a printable checklist, please see page 19 of the Understanding Breast Changes: A Health Guide for Women pdf.
Breast Changes and Conditions: Getting Follow-up Test Results
Test results will tell if you have:
Breast changes that are not cancer
Breast changes that are not cancer, but increase your risk of cancer
Breast changes that may become cancer
Breast cancer
Breast changes that are not cancer
These changes are not cancer and do not increase your risk of breast cancer. They are called benign changes.
Adenosis: Small, round lumps, or a lumpy feeling that are caused by enlarged breast lobules. Sometimes the lumps are too small to be felt. If there is scar-like tissue, the condition may be painful and is called sclerosing adenosis.
Cysts: Lumps filled with fluid. Breast cysts often get bigger and may be painful just before your menstrual period begins. Cysts are most common in premenopausal women and in women who are taking menopausal hormone therapy.
Fat necrosis: Round, firm lumps that usually don't hurt. The lumps most often appear after an injury to the breast, surgery, or radiation therapy.
Fibroadenomas: Hard, round lumps that may feel like a small marble and move around easily. They are usually painless and are most common in young women under 30 years old.
Intraductal papilloma: A wart-like growth in a milk duct of the breast. It's usually found close to the nipple and may cause clear, sticky, or bloody discharge from the nipple. It may also cause pain and a lump. It is most common in women 35-55 years old.
| Ask your doctor when you will get your test results. See the chart in Breast Conditions and Follow-Up Care for follow-up information. |
Breast changes that are not cancer, but increase your risk of cancer
These conditions are not cancer, but having them increases your risk of breast cancer. They are considered risk factors for breast cancer. Other risk factors include, for example, your age and a family history of breast cancer.
- Atypical hyperplasia:
- Atypical lobular hyperplasia (ALH) is a condition in which abnormal cells are found in the breast lobules.
- Atypical ductal hyperplasia (ADH) is a condition in which abnormal cells are found in the breast ducts.
- Lobular carcinoma in situ (LCIS) is a condition in which abnormal cells are found in the breast lobules. There are more abnormal cells in the lobule with LCIS than with ALH. Since these cells have not spread outside the breast lobules, it's called "in situ," which is a Latin term that means "in place."
The abnormal cells found in these conditions are not cancer cells. If you have ALH, ADH, or LCIS, talk with a doctor who specializes in breast health to make a plan that works best for you. Depending on your personal and family medical history, it may include:
- Mammograms every year
- Clinical breast exams every 6 to 12 months
- Tamoxifen (for all women) or raloxifene (for postmenopausal women). These drugs have been shown to lower some women's risk of breast cancer.
- Surgery. A small number of women with LCIS and high risk factors for breast cancer may choose to have surgery.
- Clinical trials. Talk with your health care provider about whether a clinical trial is a good choice for you.
|
Breast changes that may become cancer
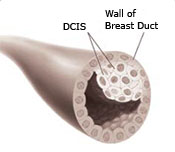
Ductal carcinoma in situ (DCIS): DCIS is a condition in which abnormal cells are found in the lining of a breast duct. These cells have not spread outside the duct to the breast tissue. This is why it is called "in situ," which is a Latin term that means "in place." You may also hear DCIS called Stage 0 breast carcinoma in situ or noninvasive cancer.
Since it's not possible to determine which cases of DCIS will become invasive breast cancer, it's important to get treatment for DCIS. Talk with a doctor who specializes in breast health to learn more. Treatment for DCIS is based on how much of the breast is affected, where DCIS is in the breast, and its grade. Most women with DCIS are cured with proper treatment.
Treatment choices for DCIS include:
- Lumpectomy. This is a type of breast-conserving surgery or breast-sparing surgery. It is usually followed by radiation therapy.
- Mastectomy. This type of surgery is used to remove the breast or as much of the breast tissue as possible.
- Tamoxifen. This drug may also be taken to lower the chance that DCIS will come back, or to prevent invasive breast cancer.
- Clinical trials. Talk with your health care provider about whether a clinical trial is a good choice for you.
Breast cancer
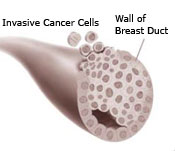
Breast cancer is a disease in which cancer cells form in the tissues of the breast. Breast cancer cells:
- Grow and divide without control
- Invade nearby breast tissue
- May form a mass called a tumor
- May metastasize, or spread, to the lymph nodes or other parts of the body
After breast cancer has been diagnosed, tests are done to find out the extent, or stage, of the cancer. The stage is based on the size of the tumor and whether the cancer has spread. Treatment depends on the stage of the cancer.
For more information about breast cancer and to get answers to any questions you may have, call 1-800-4-CANCER (1-800-422-6237). One free booklet you can ask for is: What You Need To Know About Breast Cancer. You can also visit the National Cancer Institute (NCI) online at www.cancer.gov.
| Get a second opinion |
|---|
You may want to talk with another doctor to get a second opinion on your diagnosis or on your treatment. Many women do. And remember—it's important to talk with a doctor who specializes in breast cancer or in the breast condition that you have. You can talk with your health care provider to find:
Most doctors welcome a second opinion, especially when treatment is involved. Getting a second opinion is often covered, or even required, by your health insurance. Talking with another doctor can give you peace of mind. It can also help you make the best choices about your health. |
Getting the Support You Need
It can be upsetting to notice a breast change, to get an abnormal test result, or to learn about a new condition or disease. We hope that the information in this booklet has answered some of your questions and calmed some of your fears as you talk with your health care provider and get the follow-up care you need.
Many women choose to get extra help and support for themselves. It may help to think about people who have been there for you during challenging times in the past.
- Ask friends or loved ones for support. Take someone with you while you are learning about your testing and treatment choices.
- Ask your health care provider to:
- Explain medical terms that are new or confusing
- Share with you how other people have handled the types of feelings that you are having
- Tell you about specialists that you can talk with to learn more
- Get in touch with the organizations listed in Resources to Learn More to learn more.
|
Breast Conditions and Follow-Up Care
| Conditions | Features | What Your Doctor May Recommend |
|---|---|---|
| Adenosis |
|
|
| Atypical lobular hyperplasia (ALH) |
| Regular follow-up, such as:
Treatment, such as:
|
| Atypical ductal hyperplasia (ADH) |
| Regular follow-up, such as:
Treatment, such as:
|
| Breast cancer |
| Treatment depends on the extent or stage of cancer. Tests are done to find out if the cancer has spread to others parts of your body. Treatment may include: Clinical trials may be an option for you. Talk with your doctor to learn more. |
| Cysts |
|
|
| Ductal carcinoma in situ (DCIS) |
| Treatment is needed because doctors don't know which cases of DCIS may become invasive breast cancer. Treatment choices include:
|
| Fat necrosis |
|
|
| Fibroadenoma |
|
|
| Intraductal papilloma |
|
|
| Lobular carcinoma in situ (LCIS) |
| Regular follow-up, such as:
Treatment choices:
|
| Macrocalcifications |
|
|
| Microcalcification |
|
|
| More information on these breast conditions can be found on www.cancer.gov or by calling 1-800-4-CANCER (1-800-422-6237). |
Resources to Learn More
National Cancer Institute (NCI)
NCI has comprehensive research-based information on cancer prevention, screening, diagnosis, treatment, genetics, and supportive care. We also have a clinical trials database and can offer tailored searches.
| Phone: | 1-800-4-CANCER (1-800-422-6237) |
| TTY: | 1-800-332-8615 |
| Web site: | www.cancer.gov or www.cancer.gov/espanol |
| LiveHelp: | www.cancer.gov/livehelp |
| Email: | cancergovstaff@mail.nih.gov |
Order publications at www.cancer.gov/publications or by calling 1-800-4-CANCER
We invite you to call or go online to talk with our trained information specialists, who speak English or Spanish, to:
- Get answers to any cancer-related questions you may have
- Get free NCI publications
- Learn more about specific resources and organizations in your area
- Find information on the NCI Web site www.cancer.gov
American Cancer Society (ACS)
ACS gives cancer information and support to patients, families, and caregivers. It also supports research, community education, advocacy, and public policy issues. Trained cancer information specialists can answer questions about cancer, link you to resources in your community, and provide information on local events.
| Phone: | 1-800-ACS-2345 (1-800-227-2345) |
| TTY: | 1-866-228-4327 |
| Web site: | www.cancer.org |
Centers for Disease Control and Prevention (CDC)
CDC conducts, supports, and promotes efforts to prevent cancer and increase early detection of cancer. CDC's National Breast and Cervical Cancer Early Detection Program (NBCCEDP) provides these services for underserved women:
- Clinical breast exams
- Mammograms (free or low-cost)
- Diagnostic tests if results are abnormal
- Referrals to treatment
| Toll Free: | 1-800-CDC-INFO (1-800-232-4636) |
| TTY: | 1-888-232-6348 |
| Web site: | www.cdc.gov |
Centers for Medicare & Medicaid Services (CMS)
CMS provides information for consumers about patient rights, prescription drugs, and health insurance issues, including Medicare and Medicaid.
Medicare is health insurance for people age 65 or older, under age 65 with certain disabilities, and any age with permanent kidney failure. It covers an annual screening mammogram, among other services. Medicare has information about providers in your area. English-or Spanish-speaking representatives can help you.
| Phone: | 1-800-MEDICARE (1-800-633-4227) |
| TTY: | 1-877-486-2048 |
| Web site: | www.cms.hhs.gov |
Medicaid is a program for people who need financial help with medical bills. You can learn more about this program by calling your local state welfare offices, state health department, state social services agencies, or your state's Medicaid office. Spanish-speaking staff is available in some offices.
| Web site: | www.cms.hhs.gov |
National Women's Health Information Center (NWHIC)
NWHIC is a gateway to women's health information. NWHIC has English-and Spanish-speaking Information and Referral Specialists who will order free health information for you. They can also help you find organizations that can answer your health-related questions.
| Phone: | 1-800-994-9662 |
| TTY: | 1-888-220-5446 |
| Web site: | www.womenshealth.gov |
U.S. Food and Drug Administration (FDA)
The FDA has fact sheets and brochures about mammography, as well as information about a certified mammography facility near you. It also has laws about how these facilities are run.
| Phone: | 1-888-INFO-FDA (1-888-463-6332) |
| Web site: | www.fda.gov |










