Comprehensive Primary Care Initiative
Recent Updates:
08/22 - Announced: The 500 Participating Primary Care Practices
07/26 - Updated to reflect that the practice application period has ended.
06/25 - Webinar video for primary care practitioners held 6/19 posted.
Overview
The Comprehensive Primary Care (CPC) initiative is a multi-payer initiative fostering collaboration between public and private health care payers to strengthen primary care. Medicare will work with commercial and State health insurance plans and offer bonus payments to primary care doctors who better coordinate care for their patients. Primary care practices that choose to participate in this initiative will be given resources to better coordinate primary care for their Medicare patients.
The Participating Practices
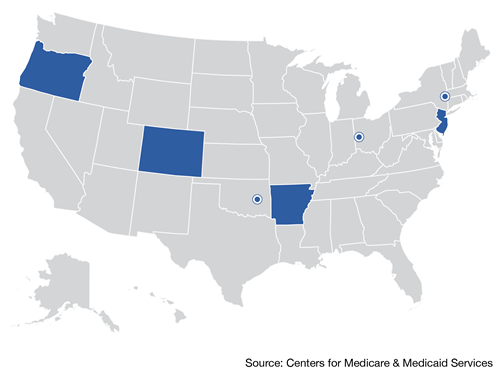
There are 500 primary care practices participating in the CPC initiative. ( List | Map )
This represents 2,144 providers serving an estimated 313,000 Medicare beneficiaries.
 | Arkansas: Statewide66 Primary Care Practices | 228 Providers | 4 Payers |
 | Colorado: Statewide73 Primary Care Practices | 335 Providers | 9 Payers |
 | New Jersey: Statewide73 Primary Care Practices | 252 Providers | 5 Payers |
 | New York: Capital District-Hudson Valley Region75 Primary Care Practices | 286 Providers | 6 Payers |
 | Ohio & Kentucky: Cincinnati-Dayton Region75 Primary Care Practices | 261 Providers | 10 Payers |
 | Oklahoma: Greater Tulsa Region68 Primary Care Practices | 265 Providers | 3 Payers |
 | Oregon: Statewide70 Primary Care Practices | 517 Providers | 6 Payers |
Background
Primary care is critical to promoting health, improving care, and reducing overall system costs, but it has been historically under-funded and under-valued in the United States. Without a significant enough investment across multiple payers, independent health plans-- covering only their own members and offering support only for their segment of the total practice population-- cannot provide enough resources to transform entire primary care practices and make expanded services available to all patients served by those practices.
Initiative Details
The CPC initiative offers a way to break through this historical impasse by inviting payers to join with Medicare in investing in primary care in 7 selected localities across the country. Eligible practices in each market were invited to apply to participate and start delivering enhanced health care services in the fall of 2012.
Practices were selected through a competitive application process based on their use of health information technology, ability to demonstrate recognition of advanced primary care delivery by accreditation bodies, service to patients covered by participating payers, participation in practice transformation and improvement activities, and diversity of geography, practice size and ownership structure.
The resources will help doctors work with patients to ensure the following:
Additional information
- Comprehensive Primary Care Initiative Fact Sheet (PDF)
- FAQ: The CPC initiative and participation in other CMS initiatives (PDF)
- Webinar: The CPC Initiative for Primary Care Practitioners
- Application materials (archived): CPC Primary Care Practice Solicitation (PDF) | CPC Payer initiative solicitation (PDF)
For more information, please send your questions to CPCi@cms.hhs.gov.

