healthnewslink
General Newsletter
October 8, 2012 |
| In this Issue |
|
|
|
|
West Nile Cases Continue to Climb, CDC Says
Number of deaths now stands at 163, up from 147 last week
 WEDNESDAY, Oct. 3 (HealthDay News) -- The number of new West Nile virus cases continued to rise in the past week, and the death toll now stands at 163, up from 147 last week, U.S. health officials reported Wednesday.
As of Tuesday, 48 states had reported West Nile infections in people, birds, or mosquitoes. A total of 3,969 cases involved people. Of these cases, 2,010 (51 percent) were classified as neuroinvasive disease (such as meningitis or encephalitis) and 1,959 (49 percent) were classified as non-neuroinvasive disease.
The total number of West Nile cases reported so far in 2012 is the highest since 2003. Seventy percent of the cases have been reported from eight states -- Texas, South Dakota, Oklahoma, Mississippi, Michigan, Louisiana, Illinois and California -- and one-third of all cases have been in Texas, according to the U.S. Centers for Disease Control and Prevention.
The best way to avoid the virus is to wear insect repellant and support local programs to eradicate mosquitoes. There is currently no treatment for West Nile virus and no vaccine to prevent it, according to the CDC.
Typically, 80 percent of people infected with the virus develop no or few symptoms, while 20 percent develop mild symptoms such as headache, joint pain, fever, skin rash and swollen lymph glands, according to the CDC.
Although most people with mild cases of West Nile virus will recover on their own, the CDC recommends that anyone who develops symptoms see their doctor right away.
People older than 50 and those with certain medical conditions, such as cancer, diabetes, hypertension, kidney disease and organ transplants, are at greater risk for serious illness.
The best way to protect yourself from West Nile virus is to avoid getting bitten by mosquitoes, which can pick up the disease from infected birds.
The CDC recommends the following steps to protect yourself:
- Use insect repellents when outside.
- Wear long sleeves and pants from dawn to dusk.
- Don't leave standing water outside in open containers, such as flowerpots, buckets and kiddie pools.
- Install or repair windows and door screens.
- Use air conditioning when possible.
More information
For more on West Nile virus, visit the U.S. Centers for Disease Control and Prevention.

|
Juggling a Hospital Job and Family Can Be Painful
Administrators should assess job conditions, researchers say
 THURSDAY, Oct. 4 (HealthDay News) --
The greater the conflict between their job and family demands, the more likely it is that nurses and other hospital workers will suffer musculoskeletal pain, a new study finds.
Researchers surveyed nearly 1,200 patient care workers at two Boston hospitals. Overall, those who reported high levels of conflict between their work duties and obligations at home were twice as likely to suffer from any kind of musculoskeletal pain in the previous three months.
They were twice as likely to have neck or shoulder pain, and those with the greatest home-work imbalance were nearly three times more likely to have arm pain. There was no link between work-family conflict and lower back pain.
The study was published online Sept. 27 in the American Journal of Industrial Medicine.
"Work-family conflict can be distracting and stressful for hospital employees," lead author Seung-Sup Kim, a postdoctoral scientist and professorial lecturer in environmental and occupational health at the George Washington University School of Public Health and Health Services, said in a university news release.
"Hospitals that adopt policies to reduce the juggling act might gain a host of benefits, including a more productive workforce, one that is not slowed down by chronic aches and pains," Kim suggested.
Further research is required to confirm a direct link between work-family conflict and an increased risk of musculoskeletal pain. But even these initial findings should convince hospital administrators to assess working conditions in their facilities, the researchers said.
"Hospital employees who don't have to juggle extreme work hours and family obligations might be happier and more productive on the job. And that's a win-win situation that will benefit not just hospitals but also workers, patients -- and family members," Kim noted.
More information
The American Academy of Physical Medicine and Rehabilitation outlines how to prevent neck pain  . .

|
Same Part of Brain Recognizes Faces and Objects, Study Finds
Fusiform face area 'lit up' identically on MRI whether auto lovers looked at cars or people
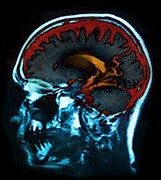 FRIDAY, Oct. 5 (HealthDay News) -- The region of the brain that we use to recognize faces is also used for other forms of specialized visual recognition, such as auto experts' ability to identify cars, a new study finds.
The fusiform face area is a blueberry-sized region located in the temporal lobe of the brain. Previous research has shown that this area is activated when people look at faces. There has been ongoing debate about whether this region is also used to recognize commonly seen objects.
In this study, researchers from Vanderbilt University in Nashville, Tenn., used MRI scans to record fusiform face area activity in the brains of automobile enthusiasts and found no evidence of a special section devoted exclusively to facial recognition. Instead, the fusiform face area of the auto experts had small, interspersed areas that responded strongly to photos of both faces and cars.
"We can't say that the same groups of neurons process both facial images and objects of expertise, but we have now mapped the area in enough detail to rule out the possibility of an area exclusively devoted to facial recognition," study author Rankin McGugin said in a university news release.
The study was published online Oct. 1 in the journal Proceedings of the National Academy of Sciences.
The researchers suggest that the knowledge that the fusiform face area can support visual expertise for categories other than faces may help scientists improve treatments for people who have trouble recognizing faces, such as those with autism.
More information
The U.S. National Institute of Neurological Disorders and Stroke has more about autism.

|
Humanitarian Work May Raise Risk of Anxiety, Depression
Researchers offer recommendations to improve mental health of aid workers
 FRIDAY, Oct. 5 (HealthDay News) -- Humanitarian aid workers are at increased risk for mental health problems such as anxiety and depression, both while in the field and after they return home, researchers say.
The workers' employers, however, can take steps to reduce this risk, according to a new report.
For the study, the investigators surveyed more than 200 international humanitarian aid workers at 19 non-governmental organizations (NGOs) and found that nearly 4 percent had symptoms of anxiety and more than 10 percent had symptoms of depression before they were deployed. Those rates are about the same as in the general population.
After deployment, nearly 12 percent of the aid workers had anxiety and about 19 percent had depression. Three to six months after arriving home, the rate of anxiety fell to less than 8 percent but the rate of depression increased to over 20 percent.
Readjusting to life at home can be difficult for aid workers, the study authors pointed out.
"It is quite common for people returning from deployment to be overwhelmed by the comforts and choices available, but unable to discuss their feelings with friends and family," study co-author Alastair Ager, a professor of clinical population and family health at Columbia University's Mailman School of Public Health, in New York City, said in a university news release.
The researchers found that it wasn't the experience of being in dangerous or threatening situations that increased the risk for depression, but instead it was the continual exposure to a challenging work environment. In addition, having weak levels of social support and a history of mental illness also boosted the risks.
Aid workers who were highly motivated and self-governing, however, reported less burnout and higher levels of life satisfaction, respectively.
The researchers recommend that NGOs should: screen candidates for history of mental illness; fully inform them of the risks related to humanitarian work; offer mental health support during and after deployment; provide a supportive work environment, manageable workload and recognition; and encourage and assist with social support and peer networks.
The study was published online recently in the journal PLoS One.
More information
The U.S. National Institute of Mental Health has more about depression.

|
| Copyright © 2012 ScoutNews, LLC. All rights reserved. |
|