Aging Hearts and Arteries: A Scientific Quest
Chapter 1: A Host of Interconnections
"The heart is purest theater…throbbing in its cage palpably as any nightingale."
Richard Selzer, MD, American Surgeon and Author
It is scarcely as big as the palm of your hand yet it sustains life, pumping up to 5 quarts or more of blood per minute to the body's organs, tissues, and cells. In a typical day, it beats 100,000 times. And in a lifetime, it beats more than 2.5 billion times. Even as you rest, your heart is working twice as hard as your leg muscles would if you were running at full speed.
Little wonder then that from earliest mythology to modern medicine, the heart has fascinated and perplexed us. Fortunately, today we know far more about the heart and the blood vessels than was known even a decade ago. Yet for all scientists have learned, there is still much more to unravel. Investigators, for instance, now know that the cardiovascular system undergoes significant changes as we age, and the heart and arteries that we are born with are surprisingly different in later life.
But how and why do these changes occur? What influence do these changes have on our risk of developing heart disease and other cardiovascular disorders as we get older? Are there any underlying signs—even in people who appear to have healthy hearts—that precede and predict who will develop severe cardiovascular disease and who won't?
Scientists called gerontologists, who study aging, are seeking to answer these and other questions. As a result of this probing, some old ideas about the aging cardiovascular system are giving way to new theories. In other cases, gerontologists are just beginning to explore some questions, and the heart and arteries are yielding their secrets grudgingly.
But to truly understand what is emerging and what remains mysterious, we'll need to start where these gerontologists began: in the normal, healthy heart.
The Intricate Pump
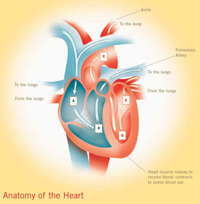
The heart is a marvel of coordination and timing. Almost completely composed of muscle called myocardium, it is well-equipped for its life-long marathon of ceaseless beating. It is essentially two pumps in one. The right side pumps blood to the lungs to load up on oxygen and dispose of carbon dioxide. The left side pumps oxygen-rich blood to the body.
To accomplish these tasks, the heart depends on a precise sequence of contractions involving its two upper chambers—the right and left atria—and its two lower ones, the right and left ventricles. Between these chambers are two valves, each with two or three flaps, also known as cusps. The tricuspid valve separates the right atrium and the right ventricle. Its counterpart, separating the left atrium and the left ventricle, is called the mitral valve. The pulmonic valve controls blood flow out of the right ventricle to the lungs where it picks up oxygen. The aortic valve controls the flow of oxygenated blood out of the left ventricle into the body. Normally these valves let blood flow in just one direction.
The heart beats in two synchronized stages. First, the right and left atria contract at the same time pumping blood into the right and left ventricles. Then the mitral and tricuspid valves close. A split second later, the ventricles contract (beat) simultaneously to pump blood out of the heart. Together, these coordinated contractions produce the familiar "lub-dub" sound of a heart beat—slightly faster than once a second. After contracting, the heart muscles momentarily relax, allowing blood to refill the heart.
To picture how this all works, imagine that as the heart relaxes dark red blood returning from the body flows into the right atrium. This blood carries little oxygen and is laden with carbon dioxide, which is produced by body tissues. When the right atrium contracts, it propels oxygen-poor blood through the tricuspid valve into the right ventricle. In turn, the right ventricle pumps blood into the pulmonary artery. From there, it flows into the lungs where it picks up oxygen and returns to the left atrium. When it contracts, the left atrium pumps the now bright red oxygenated blood through the mitral valve into the left ventricle, which pumps it into the aorta, from which it is distributed to other arteries to nourish your cells, tissues, and organs. Then the cycle begins again.
This cardiac cycle is regulated by electrical impulses, generated by the heart's internal pacemaker called the sinoatrial node (SA node), a small bundle of specialized cells located in the right atrium. These impulses cause the heart to beat. Once generated by the SA node, the impulses spread in a coordinated fashion across the heart muscle in less than a quarter of a second. As they travel, the impulses are relayed through switching stations at precise intervals, eventually causing millions of interlocked cells to contract in near unison.
Age, Change, and Adaptation
The major sequences in this ever-moving picture of the heart beat have been known for nearly 400 years. But gerontologists are uncovering another influence on this chain of events—age—and the picture appears to be even more complex. Aging, it turns out, brings not a simple slowing down of heart function, as one might expect, but a set of intricate alterations: a slowing here, an enhancement there, a minor adjustment elsewhere. The result of these numerous small alterations is adaptation. In various ingenious, important ways, the heart at age 65 has adapted to meet the needs of the 65-year-old body.
However, these refinements have a downside. In recent years, gerontologists have learned that some changes in the structure and function of the aging cardiovascular system, even in a healthy older person without any diagnosed medical condition, can actually greatly increase the risk of developing cardiovascular diseases, including high blood pressure, atherosclerosis, and heart failure. In fact, these changes can create the nearly perfect setting for the onset of severe cardiovascular disease in some healthy older people.
Gerontologists seeking to reconcile these two conflicting pictures of cardiovascular aging are intensely studying the fundamental underpinnings of the age-associated changes in the heart and arteries in hopes of discovering new ways to effectively prevent and treat cardiovascular disease in older people. This quest—from the impact of the smallest molecule to the influence of diet and exercise—is radically changing how scientists think about the cardiovascular system.
The notion, for instance, that heart cells can't replicate themselves is being reconsidered. Gerontologists now know far more about how aging affects blood vessels and how this process influences the development of atherosclerosis. They are learning much more about how physical activity, diet, and other lifestyle factors influence the "rate of aging" in the healthy older heart and arteries.
In the Beginning
Untangling the effects of age from those of disease and lifestyle is a theme that appears again and again in modern studies of aging. It wasn't always so. In the 1940s and 50s, clinical gerontologists had to conduct most of their studies in chronic care hospitals or nursing homes. The people they studied lived sedentary lives, and many may have had undetected heart disease or other illnesses. From this perspective, it appeared as if virtually all bodily functions, including the cardiovascular system, deteriorated markedly with age.
Then, in 1958, the National Institutes of Health (NIH) launched the Baltimore Longitudinal Study of Aging (BLSA). This ongoing investigation, now part of the National Institute on Aging (NIA), has tracked the lives of more than 3,000 people from age 20 to 90 and older in an effort to document the normal or usual physiological changes that occur in a stable population of people who live in the community rather than institutions. BLSA data have been valuable to scientists searching for different ways in which aging, lifestyle, and disease affect the heart and blood vessels.
The modern era of heart research has also depended heavily on the development of powerful, non-invasive technologies, such as echocardiography, magnetic resonance imaging, and radionuclide imaging, which have allowed investigators to easily see valves, walls, and chambers of the heart and the flow of blood through these chambers. Two techniques, thallium scintigraphy, a highly sensitive radionuclide stress test that can detect hidden coronary artery disease, and stress electrocardiogram (ECG), a measurement of the electrical activity of the heart, are particularly useful. In combination, these two tests allow researchers to differentiate between the effects of age and the effects of coronary disease that is so prevalent among older people—effects that were once entangled and indistinguishable.
The Next Steps
As you explore this booklet, you will find that scientists have learned a tremendous amount about aging. Today, more than ever, they understand what causes your blood vessels and heart to age and know a lot about how this process interacts with cardiovascular disease-related changes. In addition, they have even pinpointed risk factors that increase the odds a person will develop cardiovascular disease as well as other illnesses. And while many mysteries of the aging heart and arteries remain unsolved, gerontologists have discovered much about how to prevent or postpone heart disease in later life.
Publication Date: April 2005
Page Last Updated: May 3, 2012