General Information About Childhood Acute Myeloid Leukemia and Other Myeloid Malignancies
Key Points for This Section
- Leukemia and other diseases of the blood and bone marrow may affect red blood cells, white blood cells, and platelets.
- Childhood acute myeloid leukemia (AML) is a type of cancer in which the bone marrow makes a large number of abnormal blood cells.
- Other myeloid diseases can affect the blood and bone marrow.
- The risk factors for developing childhood AML, childhood CML, JMML, TMD, and MDS are similar.
- Possible signs of childhood AML, childhood CML, JMML, or MDS include fever, feeling tired, and easy bleeding or bruising.
- Tests that examine the blood and bone marrow are used to detect (find) and diagnose childhood AML, childhood CML, JMML, TMD, and MDS.
- Certain factors affect prognosis (chance of recovery) and treatment options.
Leukemia and other diseases of the blood and bone marrow may affect red blood cells, white blood cells, and platelets.
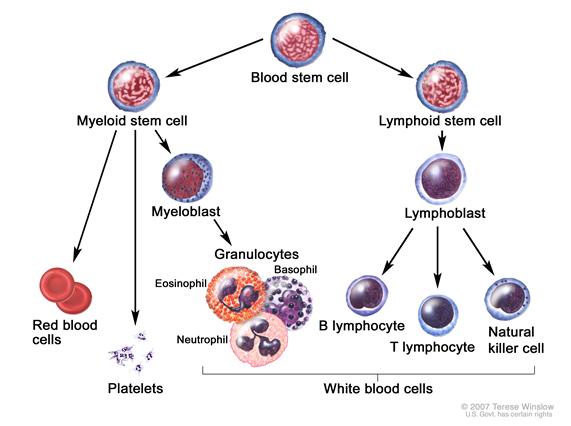
Normally, the bone marrow makes blood stem cells (immature cells) that become mature blood cells over time. A blood stem cell may become a myeloid stem cell or a lymphoid stem cell. A lymphoid stem cell becomes a white blood cell. A myeloid stem cell becomes one of three types of mature blood cells:
- Red blood cells that carry oxygen and other substances to all tissues of the body.
- White blood cells that fight infection and disease.
- Platelets that form blood clots to stop bleeding.
Childhood acute myeloid leukemia (AML) is a type of cancer in which the bone marrow makes a large number of abnormal blood cells.
Cancers that are acute usually get worse quickly if they are not treated. Cancers that are chronic usually get worse slowly. Acute myeloid leukemia (AML) is also called acute myelogenous leukemia, acute myeloblastic leukemia, acute granulocytic leukemia, or acute nonlymphocytic leukemia.
In AML, the myeloid stem cells usually become a type of immature white blood cell called myeloblasts (or myeloid blasts). The myeloblasts, or leukemia cells, in AML are abnormal and do not become healthy white blood cells. The leukemia cells can build up in the blood and bone marrow so there is less room for healthy white blood cells, red blood cells, and platelets. When this happens, infection, anemia, or easy bleeding may occur. The leukemia cells can spread outside the blood to other parts of the body, including the central nervous system (brain and spinal cord), skin, and gums. Sometimes leukemia cells form a solid tumor called a granulocytic sarcoma or chloroma.
There are subtypes of AML based on the type of blood cell that is affected. The treatment of AML is different when it is a subtype called acute promyelocytic leukemia (APL) or when the child has Down syndrome.
Other myeloid diseases can affect the blood and bone marrow.
In chronic myelogenous leukemia (CML), too many bone marrow stem cells become a type of white blood cell called granulocytes. Some of these bone marrow stem cells never become mature white blood cells. These are called blasts. Over time, the granulocytes and blasts crowd out the red blood cells and platelets in the bone marrow. CML is rare in children.
Juvenile myelomonocytic leukemia
Juvenile myelomonocytic leukemia (JMML) is a rare childhood cancer that occurs more often in children around the age of 2 years. In JMML, too many bone marrow stem cells become 2 types of white blood cells called myelocytes and monocytes. Some of these bone marrow stem cells never become mature white blood cells. These immature cells, called blasts, are unable to do their usual work. Over time, the myelocytes, monocytes, and blasts crowd out the red blood cells and platelets in the bone marrow. When this happens, infection, anemia, or easy bleeding may occur.
Transient myeloproliferative disorder
Transient myeloproliferative disorder (TMD) is a disorder of the bone marrow that can develop in newborns who have Down syndrome. This disorder usually goes away on its own within the first 3 weeks of life. Infants who have Down syndrome and TMD have an increased chance of developing AML before the age of 3 years.
In myelodysplastic syndromes (MDS), the bone marrow makes too few red blood cells, white blood cells, and platelets. These blood cells may not mature and enter the blood. The treatment for MDS depends on how much lower than normal the number of red blood cells, white blood cells, or platelets is. MDS may progress to AML.
This summary is about childhood AML, childhood CML, JMML, TMD, and MDS. See the following PDQ summaries for more information about other types of leukemia and diseases of the blood and bone marrow:
- Adult Acute Myeloid Leukemia Treatment
- Chronic Myelogenous Leukemia Treatment
- Adult Acute Lymphoblastic Leukemia Treatment
- Childhood Acute Lymphoblastic Leukemia Treatment
- Chronic Lymphocytic Leukemia Treatment
- Hairy Cell Leukemia Treatment
- Myelodysplastic Syndromes Treatment
- Myelodysplastic/Myeloproliferative Neoplasms Treatment
The risk factors for developing childhood AML, childhood CML, JMML, TMD, and MDS are similar.
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn’t mean that you will not get cancer. Talk with your child’s doctor if you think your child may be at risk. Possible risk factors for childhood AML, childhood CML, JMML, TMD, and MDS include the following:
- Having a brother or sister, especially a twin, with leukemia.
- Being Hispanic.
- Being exposed to cigarette smoke or alcohol before birth.
- Having a history of MDS (also called preleukemia) or aplastic anemia.
- Past treatment with chemotherapy or radiation therapy.
- Being exposed to ionizing radiation or chemicals such as benzene.
- Having certain genetic disorders, such as:
Possible signs of childhood AML, childhood CML, JMML, or MDS include fever, feeling tired, and easy bleeding or bruising.
These and other symptoms may be caused by childhood AML, childhood CML, JMML, or MDS. Other conditions may cause the same symptoms. Check with a doctor if your child has any of the following problems:
- Fever with or without an infection.
- Night sweats.
- Shortness of breath.
- Weakness or feeling tired.
- Easy bruising or bleeding.
- Petechiae (flat, pinpoint spots under the skin caused by bleeding).
- Pain in the bones or joints.
- Pain or feeling of fullness below the ribs.
- Painless lumps in the neck, underarm, stomach, groin, or other parts of the body. When seen in childhood AML, these lumps, called leukemia cutis, may be blue or purple.
- Painless lumps that are sometimes around the eyes. These lumps, called chloromas, are sometimes seen in childhood AML and may be blue-green.
- An eczema -like skin rash.
The symptoms of TMD may include the following:
- Swelling all over the body.
- Shortness of breath.
- Trouble breathing.
- Weakness or feeling tired.
- Pain below the ribs.
Tests that examine the blood and bone marrow are used to detect (find) and diagnose childhood AML, childhood CML, JMML, TMD, and MDS.
The following tests and procedures may be used:
- Physical exam and history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
- Complete blood count (CBC) with differential: A procedure in which a sample of blood is drawn and checked for the following:
- The number of red blood cells and platelets.
- The number and type of white blood cells.
- The amount of hemoglobin (the protein that carries oxygen) in the red blood cells.
- The portion of the blood sample made up of red blood cells.
Enlarge
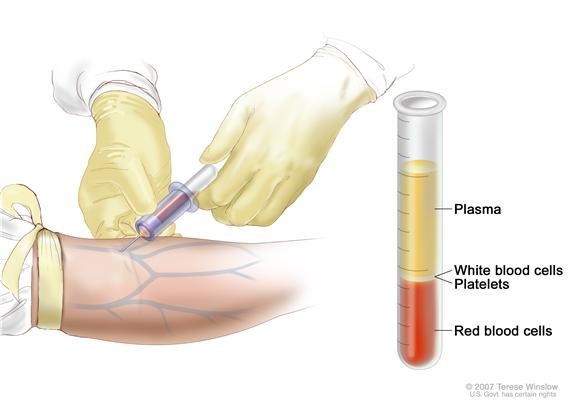 Complete blood count (CBC). Blood is collected by inserting a needle into a vein and allowing the blood to flow into a tube. The blood sample is sent to the laboratory and the red blood cells, white blood cells, and platelets are counted. The CBC is used to test for, diagnose, and monitor many different conditions.
Complete blood count (CBC). Blood is collected by inserting a needle into a vein and allowing the blood to flow into a tube. The blood sample is sent to the laboratory and the red blood cells, white blood cells, and platelets are counted. The CBC is used to test for, diagnose, and monitor many different conditions. - Blood chemistry studies: A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease in the organ or tissue that makes it.
- Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- Peripheral blood smear: A procedure in which a sample of blood is checked for blast cells, the number and kinds of white blood cells, number of platelets, and changes in the shape of the blood cells.
- Biopsy: The removal of cells or tissues so they can be viewed under a microscope by a pathologist to check for signs of cancer. Biopsies that may be done for childhood AML include the following:
- Bone marrow aspiration and biopsy: The removal of bone marrow, blood, and a small piece of bone by inserting a hollow needle into the hipbone or breastbone.Enlarge
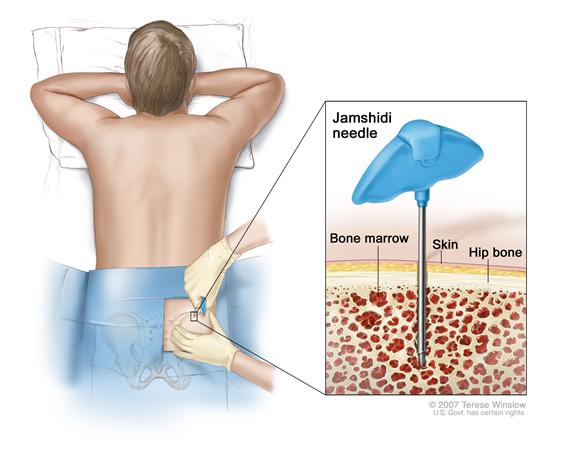 Bone marrow aspiration and biopsy. After a small area of skin is numbed, a Jamshidi needle (a long, hollow needle) is inserted into the patient’s hip bone. Samples of blood, bone, and bone marrow are removed for examination under a microscope.
Bone marrow aspiration and biopsy. After a small area of skin is numbed, a Jamshidi needle (a long, hollow needle) is inserted into the patient’s hip bone. Samples of blood, bone, and bone marrow are removed for examination under a microscope. - Tumor biopsy: A biopsy of a chloroma may be done.
- Lymph node biopsy: The removal of all or part of a lymph node.
- Bone marrow aspiration and biopsy: The removal of bone marrow, blood, and a small piece of bone by inserting a hollow needle into the hipbone or breastbone.
- Cytogenetic analysis: A laboratory test in which cells in a sample of blood or bone marrow are viewed under a microscope to look for certain changes in the chromosomes.
- Immunophenotyping: A process used to identify cells, based on the types of antigens or markers on the surface of the cell, that may include special staining of the blood and bone marrow cells. This process is used to diagnose the subtype of AML by comparing the cancer cells to normal cells of the immune system.
- FISH (fluorescence in situ hybridization): A laboratory technique used to look at genes or chromosomes in cells and tissues. Pieces of DNA that contain a fluorescent dye are made in the laboratory and added to cells or tissues on a glass slide. When these pieces of DNA bind to specific genes or areas of chromosomes on the slide, they light up when viewed under a microscope with a special light.
- Reverse transcription–polymerase chain reaction test (RT–PCR): A laboratory test in which cells in a sample of tissue are studied using chemicals to look for certain changes in the structure or function of genes.
- Lumbar puncture: A procedure used to collect cerebrospinal fluid from the spinal column. This is done by placing a needle into the spinal column. This procedure is also called an LP or spinal tap.Enlarge
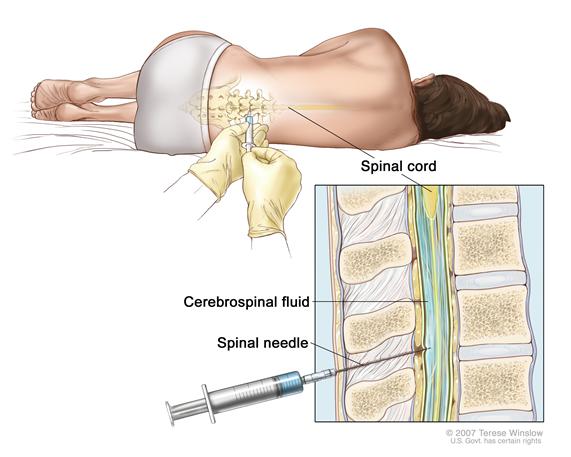 Lumbar puncture. A patient lies in a curled position on a table. After a small area on the lower back is numbed, a spinal needle (a long, thin needle) is inserted into the lower part of the spinal column to remove cerebrospinal fluid (CSF, shown in blue). The fluid may be sent to a laboratory for testing.
Lumbar puncture. A patient lies in a curled position on a table. After a small area on the lower back is numbed, a spinal needle (a long, thin needle) is inserted into the lower part of the spinal column to remove cerebrospinal fluid (CSF, shown in blue). The fluid may be sent to a laboratory for testing.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) and treatment options for childhood AML depend on the following:
- The age of the child at diagnosis.
- The race or ethnic group of the child.
- Whether the child is greatly overweight.
- Number of white blood cells in the blood at diagnosis.
- Whether the AML was caused by previous anticancer treatment.
- The subtype of AML.
- Whether there are certain chromosome or gene changes in the leukemia cells.
- Whether the child has Down syndrome. Most children with AML and Down syndrome can be cured of their leukemia.
- Whether the child has leukemia in the central nervous system (brain and spinal cord).
- How quickly the leukemia responds to initial treatment.
- Whether the AML is newly diagnosed or has recurred (come back) after being treated.
- The length of time since treatment ended, for AML that has recurred.
The prognosis and treatment options for childhood CML depend on how long it has been since the patient was diagnosed and how many blast cells are in the blood.
The prognosis (chance of recovery) and treatment options for JMML depend on the following:
- The age of the child at diagnosis.
- How many red blood cells, white blood cells, or platelets are in the blood.
- Whether the JMML is untreated or has recurred after treatment.
The prognosis (chance of recovery) and treatment options for MDS depend on the following:
- Whether the MDS was caused by previous cancer treatment.
- How low the numbers of red blood cells, white blood cells, or platelets are.
- Whether the MDS is untreated or has recurred after treatment.


 Back to Top
Back to Top