
For more information, visit http://www.nhlbi.nih.gov/health/health-topics/topics/pad/
What Is Peripheral Arterial Disease?
Peripheral arterial disease (P.A.D.) is a disease in which plaque (plak) builds up in the arteries that carry blood to your head, organs, and limbs. Plaque is made up of fat, cholesterol, calcium, fibrous tissue, and other substances in the blood.
When plaque builds up in the body's arteries, the condition is called atherosclerosis (ATH-er-o-skler-O-sis). Over time, plaque can harden and narrow the arteries. This limits the flow of oxygen-rich blood to your organs and other parts of your body.
P.A.D. usually affects the arteries in the legs, but it also can affect the arteries that carry blood from your heart to your head, arms, kidneys, and stomach. This article focuses on P.A.D. that affects blood flow to the legs.
Normal Artery and Artery With Plaque Buildup
The illustration shows how P.A.D. can affect arteries in the legs. Figure A shows a normal artery with normal blood flow. The inset image shows a cross-section of the normal artery. Figure B shows an artery with plaque buildup that's partially blocking blood flow. The inset image shows a cross-section of the narrowed artery.
Overview
Blocked blood flow to your legs can cause pain and numbness. It also can raise your risk of getting an infection in the affected limbs. Your body may have a hard time fighting the infection.
If severe enough, blocked blood flow can cause gangrene (tissue death). In very serious cases, this can lead to leg amputation.
If you have leg pain when you walk or climb stairs, talk with your doctor. Sometimes older people think that leg pain is just a symptom of aging. However, the cause of the pain could be P.A.D. Tell your doctor if you're feeling pain in your legs and discuss whether you should be tested for P.A.D.
Smoking is the main risk factor for P.A.D. If you smoke or have a history of smoking, your risk of P.A.D. increases up to four times. Other factors, such as age and having certain diseases or conditions, also increase your risk of P.A.D.
Outlook
P.A.D. increases your risk of coronary heart disease (CHD; also called coronary artery disease), heart attack, stroke, and transient ischemic attack ("mini-stroke"). If you have CHD, you have a 1 in 3 chance of having blocked leg arteries.
Although P.A.D. is serious, it's treatable. If you have the disease, see your doctor regularly and treat the underlying atherosclerosis.
P.A.D. treatment may slow or stop disease progress and reduce the risk of complications. Treatments include lifestyle changes, medicines, and surgery or procedures. Researchers continue to explore new therapies for P.A.D.
Other Names for Peripheral Arterial Disease
- Atherosclerotic peripheral arterial disease
- Claudication (klaw-dih-KA-shen)
- Hardening of the arteries
- Leg cramps from poor circulation
- Peripheral vascular disease
- Poor circulation
- Vascular disease
What Causes Peripheral Arterial Disease?
The most common cause of peripheral arterial disease (P.A.D.) is atherosclerosis. Atherosclerosis is a disease in which plaque builds up in your arteries. The exact cause of atherosclerosis isn't known.
The disease may start if certain factors damage the inner layers of the arteries. These factors include:
- Smoking
- High amounts of certain fats and cholesterol in the blood
- High blood pressure
- High amounts of sugar in the blood due to insulin resistance or
diabetes
When damage occurs, your body starts a healing process. The healing may cause plaque to build up where the arteries are damaged.
Eventually, a section of plaque can rupture (break open), causing a blood clot to form at the site. The buildup of plaque or blood clots can severely narrow or block the arteries and limit the flow of oxygen-rich blood to your body.
Who Is at Risk for Peripheral Arterial Disease?
Peripheral arterial disease (P.A.D.) affects millions of people in the United States. The disease is more common in African Americans than any other racial or ethnic group.
The major risk factors for P.A.D. are smoking, older age, and having certain diseases or conditions.
Smoking
Smoking is the main risk factor for P.A.D. Your risk of P.A.D. increases four times if you smoke or have a history of smoking.
On average, people who smoke and develop P.A.D. have symptoms 10 years earlier than people who don't smoke and develop P.A.D.
Quitting smoking slows the progress of P.A.D. Smoking even one or two cigarettes a day can interfere with P.A.D. treatments. People who smoke and people who have diabetes are at highest risk for P.A.D. complications, such as gangrene (tissue death) in the leg from decreased blood flow.
Older Age
Older age also is a risk factor for P.A.D. Plaque builds up in your arteries as you age. About 1 in every 20 Americans over the age of 50 has P.A.D. The risk continues to rise as you get older.
Older age combined with other risk factors, such as smoking or diabetes, also puts you at higher risk for P.A.D.
Diseases and Conditions
Many diseases and conditions can raise your risk of P.A.D., including:
- Diabetes. About 1 in 3 people older than 50 who has diabetes also has P.A.D.
- High blood pressure or a family history of it.
- High blood cholesterol or a family history of it.
- Coronary heart disease (CHD) or a family history of it.
- Stroke or a family history of it.
- Metabolic syndrome (a group of risk factors that raise your risk of CHD and other health problems, such as P.A.D., stroke, and diabetes).
What Are the Signs and Symptoms of Peripheral Arterial Disease?
Many people who have peripheral arterial disease (P.A.D.) don't have any signs or symptoms. Others may have many signs and symptoms.
Even if you don't have signs or symptoms, ask your doctor whether you should get checked for P.A.D. if you're:
- Aged 70 or older
- Aged 50 or older and have a history of smoking or diabetes
- Younger than 50 and have diabetes and one or more risk factors for atherosclerosis
Intermittent Claudication
People who have P.A.D. may have symptoms when walking or climbing stairs. These symptoms may include pain, numbness, aching, or heaviness in the leg muscles.
Symptoms also may include cramping in the affected leg(s) and in the buttocks, thighs, calves, and feet. Symptoms may ease after resting.
These symptoms are called intermittent claudication. During physical activity, your muscles need increased blood flow. If your blood vessels are narrowed or blocked, your muscles won't get enough blood, which will lead to symptoms. When resting, the muscles need less blood flow, so the symptoms will go away.
About 10 percent of people who have P.A.D. have claudication. This symptom is more likely in people who also have atherosclerosis in other arteries.
Other Signs and Symptoms
Other signs and symptoms of P.A.D. include:
- Weak or absent pulses in the legs or feet
- Sores or wounds on the toes, feet, or legs that heal slowly, poorly, or not at all
- A pale or bluish color to the skin
- A lower temperature in one leg compared to the other leg
- Poor nail growth on the toes and decreased hair growth on the legs
- Erectile dysfunction, especially among men who have diabetes
How Is Peripheral Arterial Disease Diagnosed?
Peripheral arterial disease (P.A.D.) is diagnosed based on your medical and family histories, a physical exam, and test results.
P.A.D. often is diagnosed after symptoms are reported. A correct diagnosis is important because people who have P.A.D. are at higher risk for coronary heart disease (CHD), heart attack, stroke, and transient ischemic attack ("mini-stroke"). If you have P.A.D., your doctor also may want to check for signs of these diseases and conditions.
Specialists Involved
Primary care doctors, such as internists and family doctors, may treat people who have mild P.A.D. For more advanced P.A.D., a vascular specialist may be involved. This is a doctor who specializes in treating blood vessel diseases and conditions.
A cardiologist also may be involved in treating people who have P.A.D. Cardiologists treat heart problems, such as CHD and heart attack, which often affect people who have P.A.D.
Medical and Family Histories
Your doctor may ask:
- Whether you have any risk factors for P.A.D. For example, he or she may ask whether you smoke or have diabetes.
- About your symptoms, including any symptoms that occur when walking, exercising, sitting, standing, or climbing.
- About your diet.
- About any medicines you take, including prescription and over-the-counter medicines.
- Whether anyone in your family has a history of heart or blood vessel diseases.
Physical Exam
During the physical exam, your doctor will look for signs of P.A.D. He or she may check the blood flow in your legs or feet to see whether you have weak or absent pulses.
Your doctor also may check the pulses in your leg arteries for an abnormal whooshing sound called a bruit (broo-E). He or she can hear this sound with a stethoscope. A bruit may be a warning sign of a narrowed or blocked artery.
Your doctor may compare blood pressure between your limbs to see whether the pressure is lower in the affected limb. He or she also may check for poor wound healing or any changes in your hair, skin, or nails that may be signs of P.A.D.
Diagnostic Tests
Ankle-Brachial Index
A simple test called an ankle-brachial index (ABI) often is used to diagnose P.A.D. The ABI compares blood pressure in your ankle to blood pressure in your arm. This test shows how well blood is flowing in your limbs.
ABI can show whether P.A.D. is affecting your limbs, but it won't show which blood vessels are narrowed or blocked.
A normal ABI result is 1.0 or greater (with a range of 0.90 to 1.30). The test takes about 10 to 15 minutes to measure both arms and both ankles. This test may be done yearly to see whether P.A.D. is getting worse.
Ankle-Brachial Index
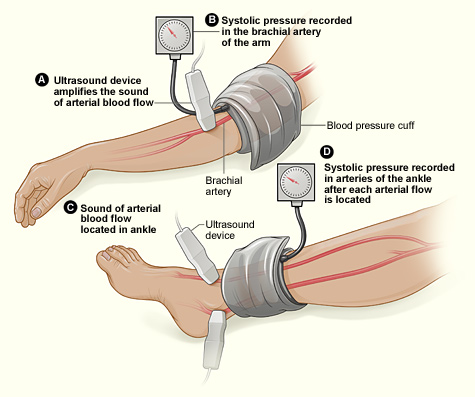
The illustration shows the ankle-brachial index test. The test compares blood pressure in the ankle to blood pressure in the arm. As the blood pressure cuff deflates, the blood pressure in the arteries is recorded.
Doppler Ultrasound
A Doppler ultrasound looks at blood flow in the major arteries and veins in the limbs. During this test, a handheld device is placed on your body and passed back and forth over the affected area. A computer converts sound waves into a picture of blood flow in the arteries and veins.
The results of this test can show whether a blood vessel is blocked. The results also can help show the severity of P.A.D.
Treadmill Test
A treadmill test can show the severity of symptoms and the level of exercise that brings them on. You'll walk on a treadmill for this test. This shows whether you have any problems during normal walking.
You may have an ABI test before and after the treadmill test. This will help compare blood flow in your arms and legs before and after exercise.
Magnetic Resonance Angiogram
A magnetic resonance angiogram (MRA) uses magnetic and radio wave energy to take pictures of your blood vessels. This test is a type of magnetic resonance imaging (MRI).
An MRA can show the location and severity of a blocked blood vessel. If you have a pacemaker, man-made joint, stent, surgical clips, mechanical heart valve, or other metallic devices in your body, you might not be able to have an MRA. Ask your doctor whether an MRA is an option for you.
Arteriogram
An arteriogram provides a "road map" of the arteries. Doctors use this test to find the exact location of a blocked artery.
For this test, dye is injected through a needle or catheter (tube) into one of your arteries. This may make you feel mildly flushed. After the dye is injected, an x ray is taken. The x ray can show the location, type, and extent of the blockage in the artery.
Some doctors use a newer method of arteriogram that uses tiny ultrasound cameras. These cameras take pictures of the insides of the blood vessels. This method is called intravascular ultrasound.
Blood Tests
Your doctor may recommend blood tests to check for P.A.D. risk factors. For example, blood tests can help diagnose conditions such as diabetes and high blood cholesterol.
How Is Peripheral Arterial Disease Treated?
Treatments for peripheral arterial disease (P.A.D.) include lifestyle changes, medicines, and surgery or procedures.
The overall goals of treating P.A.D. include reducing symptoms, improving quality of life, and preventing complications. Treatment is based on your signs and symptoms, risk factors, and results from a physical exam and tests.
Lifestyle Changes
Treatment often includes making long-lasting lifestyle changes, such as:
- Quitting smoking. Your risk of P.A.D. increases four times if you smoke. Smoking also raises your risk for other diseases, such as coronary heart disease (CHD). Talk with your doctor about programs and products that can help you quit smoking. Also, try to avoid secondhand smoke.
- Lowering blood pressure. This lifestyle change can help you avoid the risk of stroke, heart attack, heart failure, and kidney disease.
- Lowering high blood cholesterol. Lowering cholesterol can delay or even reverse the buildup of plaque in your arteries.
- Lowering blood glucose (sugar) levels if you have diabetes. A hemoglobin A1C test can show how well you have controlled your blood sugar level over the past 3 months.
- Being physically active. Talk with your doctor about taking part in a supervised exercise program. This type of program has been shown to reduce P.A.D. symptoms.
Follow a healthy eating plan that's low in total fat, saturated fat, trans fat, cholesterol, and sodium (salt). Include fruits, vegetables, and low-fat dairy products in your diet. If you're overweight or obese, work with your doctor to create a reasonable weight-loss plan.
Two examples of healthy eating plans are Therapeutic Lifestyle Changes (TLC) and Dietary Approaches to Stop Hypertension (DASH).
Medicines
Your doctor may prescribe medicines to:
- Treat unhealthy cholesterol levels and high blood pressure
- Prevent blood clots from forming due to low blood flow
- Help ease leg pain that occurs when you walk or climb stairs
Surgery or Procedures
Bypass Grafting
Your doctor may recommend bypass grafting surgery if blood flow in your limb is blocked or nearly blocked. For this surgery, your doctor uses a blood vessel from another part of your body or a man-made tube to make a graft.
This graft bypasses (that is, goes around) the blocked part of the artery. The bypass allows blood to flow around the blockage.
This surgery doesn't cure P.A.D., but it may increase blood flow to the affected limb.
Angioplasty and Stenting
Your doctor may recommend angioplasty (AN-jee-oh-plas-tee) to restore blood flow through a narrowed or blocked artery.
During this procedure, a catheter (thin tube) with a balloon at the tip is inserted into a blocked artery. The balloon is then inflated, which pushes plaque outward against the artery wall. This widens the artery and restores blood flow.
A stent (a small mesh tube) may be placed in the artery during angioplasty. A stent helps keep the artery open after angioplasty is done. Some stents are coated with medicine to help prevent blockages in the artery.
Atherectomy
Atherectomy (ath-eh-REK-to-me) is a procedure that removes plaque buildup from an artery. During the procedure, a catheter is used to insert a small cutting device into the blocked artery. The device is used to shave or cut off plaque.
The bits of plaque are removed from the body through the catheter or washed away in the bloodstream (if they're small enough).
Doctors also can do atherectomy using a special laser that dissolves the blockage.
Other Types of Treatment
Researchers are studying cell and gene therapies to treat P.A.D. However, these treatments aren't yet available outside of clinical trials.
For more information about clinical trials, go to the "Clinical Trials" section of this article or the Health Topics Clinical Trials article.
How Can Peripheral Arterial Disease Be Prevented?
Taking action to control your risk factors can help prevent or delay peripheral arterial disease (P.A.D.) and its complications.
Know your family history of health problems related to P.A.D. If you or someone in your family has the disease, be sure to tell your doctor.
If you smoke, quit. Smoking is the main risk factor for P.A.D. Your risk of P.A.D. increases four times if you smoke or have a history of smoking. Talk with your doctor about programs and products that can help you quit smoking. Also, try to avoid secondhand smoke.
The Health Topics Smoking and Your Heart article and the National Heart, Lung, and Blood Institute's (NHLBI's) "Your Guide to a Healthy Heart" both include information about how to quit smoking.
Follow a healthy diet that includes a variety of fruits, vegetables, and whole grains. A healthy diet also includes lean meats, poultry, fish, beans, and fat-free or low-fat milk or milk products. A healthy diet is low in saturated fat, trans fat, cholesterol, sodium (salt), and added sugar.
The National Heart, Lung, and Blood Institute's (NHLBI's) Therapeutic Lifestyle Changes (TLC) and Dietary Approaches to Stop Hypertension (DASH) are two programs that promote healthy eating.
If you're overweight or obese, work with your doctor to create a reasonable weight-loss plan. Also, try to be physically active. Physical activity can improve your fitness level and your health. Talk with your doctor about the types of activity that are safe for you.
The Health Topics Physical Activity and Your Heart article and the NHLBI's "Your Guide to Physical Activity and Your Heart" include information about physical activity. Although these resources focus on heart health, they also apply to general health and well-being.
The lifestyle changes described above can reduce your risk of P.A.D. These changes also can help prevent and control conditions that can lead to P.A.D., such as diabetes, high blood pressure, high blood cholesterol, coronary heart disease, and stroke.
Living With Peripheral Arterial Disease
If you have peripheral arterial disease (P.A.D.), you're more likely to also have coronary heart disease (CHD), heart attack, stroke, and transient ischemic
attack ("mini-stroke"). However, you can take steps to treat and control P.A.D. and lower your risk for these other conditions.
Living With Peripheral Arterial Disease Symptoms
If you have P.A.D., you may feel pain in your calf or thigh muscles after walking. Try to take a break and allow the pain to ease before walking again. Over time, this may increase the distance that you can walk without pain.
Talk with your doctor about taking part in a supervised exercise program. This type of program has been shown to reduce P.A.D. symptoms.
Check your feet and toes regularly for sores or possible infections. Wear comfortable shoes that fit well. Maintain good foot hygiene and have professional medical treatment for corns, bunions, or calluses.
Ongoing Health Care Needs and Lifestyle Changes
See your doctor for checkups as he or she advises. If you have P.A.D. without symptoms, you should still see your doctor regularly. Take all medicines as your doctor prescribes.
Lifestyle changes can help prevent or delay P.A.D. and other related problems, such as CHD, heart attack, stroke, and transient ischemic attack. Lifestyle changes include quitting smoking, controlling risk factors, being physically active, and following a healthy diet.
For more information about lifestyle changes, go to "How Can Peripheral Arterial Disease Be Treated?"
Clinical Trials
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. For example, this research has uncovered some of the causes of various diseases and conditions, as well as ways to prevent, diagnose, or treat them.
The NHLBI continues to support research aimed at learning more about various diseases and conditions, including peripheral arterial disease (P.A.D.). For example, NHLBI-supported research on P.A.D. includes studies that:
- Explore whether group walking sessions increase physical activity in people who have P.A.D.
- Compare how effective certain exercise programs are at reducing leg pain in people who have P.A.D.
- Examine how inflammation and insulin resistance affect people who have P.A.D.
Much of this research depends on the willingness of volunteers to take part in clinical trials. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions.
For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they're widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don't directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You'll learn about treatments and tests you may receive, and the benefits and risks they may pose. You'll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you'll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to P.A.D., talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
- http://clinicalresearch.nih.gov
- www.clinicaltrials.gov
- www.nhlbi.nih.gov/studies/index.htm
- www.researchmatch.org
Links to Other Information About Peripheral Arterial Disease
NHLBI Resources
- Atherosclerosis (Health Topics)
- DASH Eating Plan (Health Topics)
- "Facts About P.A.D." (also available in Spanish)
- "Facts About P.A.D. for African Americans"
- Keep the Beat™ Deliciously Healthy Eating
- Physical Activity and Your Heart (Health Topics)
- Smoking and Your Heart (Health Topics)
- Stay in Circulation: Take Steps to Learn About P.A.D.
- "Stay in Circulation: Take Steps to Learn About P.A.D. Wallet Card"
- "Your Guide to Lowering Your Blood Pressure With DASH"
- "Your Guide to Lowering Your Cholesterol With TLC"
Non-NHLBI Resources
- Peripheral Arterial Disease (MedlinePlus)
Clinical Trials
- Clinical Trials (Health Topics)
- Current Research (ClinicalTrials.gov)
- NHLBI Clinical Trials
- NIH Clinical Research Trials and You (National Institutes of Health)
- ResearchMatch (funded by the National Institutes of Health)
____________
™ Keep the Beat is a trademark of the U.S. Department of Health and Human Services













