Collaboration Primer:
Establishing HAI Prevention Collaboratives
Partnerships. Cooperation. Shared ideas. Teamwork. Collective efforts.
Collaboration is the cornerstone for increasing success in the elimination of healthcare-associated infections. Effective collaboration will magnify the reach of ARRA funds. Each agency and entity involved in HAI prevention brings its unique knowledge and talent to share; bringing us closer to our shared mission toward elimination of HAIs.
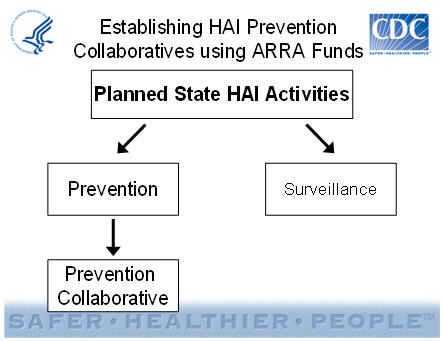
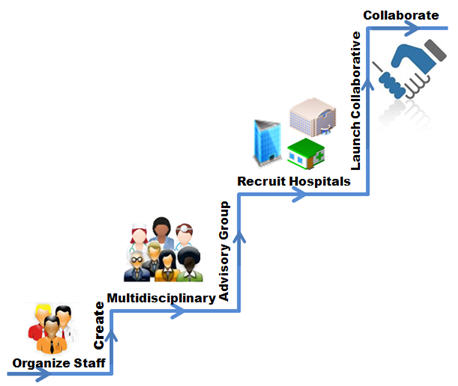
Planning a collaboration
There are many building blocks on the way to assembling a successful collaborative. A successful HAI collaborative begins with staffing. With staff in place, create and convene a multidisciplinary advisory group and recruit healthcare facilities to participate. Develop communication strategies to expand the reach of HAI prevention. Implement methods to measure success of the overall efforts to guide in planning for future success.
Staffing
Staff should consist of an on-staff Project Coordinator in addition to available, or on-staff, experts in infection control and prevention with experience in multicenter collaborative improvement projects.
The Project Coordinator, preferably an internal staffer with previously established relationships, should be the first person hired. This full-time coordinator will manage logistics; coordinate meetings and communications; track progress; oversee day-to-day program operations; and troubleshoot when needed.
Infection prevention and clinical expertise can be provided by a staffer or consultants that may be available on an as-needed basis. When hiring to fill this role, review the literature from expert(s) in your state and be certain to have experts who are passionate and committed to infection prevention and suitable for championing concepts. Contact the local Association for Professionals in Infection Control and Epidemiology (APIC) chapters and consult with academic partners and experts in healthcare epidemiology at local hospitals and/or universities (i.e., Society for Healthcare Epidemiology of America [SHEA] members.
Bring in someone from CDC with clinical and infection control expertise. Provide facilities with suggestions for performing tasks and assist with data validation. Ensure that facilities use the same criteria and data elements. Train hospital staff on data elements and criteria. Help guide facilities in information sharing sessions. Encourage discussion of what is working, and what is not, to improve prevention activities. Involve front-line hospital personnel in finding solutions to problems.
The best approach to success is to bring aboard those knowledgeable and experienced in multicenter collaborative improvement projects (i.e., recruitment, training, communication). You may have these persons internally or need to reach out for external consultation services (*available from groups such as: Institute for Healthcare Improvement (IHI) or Fieldstone Alliance.
*These links do not constitute an endorsement of these organizations or their programs by CDC or the federal government, and none should be inferred.
Multidisciplinary Advisory Group
Assemble a multidisciplinary advisory group. When building an advisory group, keep in mind the responsibilities and commitment required from each member. Your advisory group will need a shared vision and focus to make important decisions, such as which infections to target. This group will determine the needs of the state/hospitals and consult with your CDC subject matter expert. This process requires getting letters of commitment from steering group members, face-to-face meetings, selection of targets for your prevention collaborative, selection of specific goals, and relaying the outcomes to the steering group.
States may use different terms for their advisory groups, such as Steering Groups, Advisory Council, State HAI Advisory Council, or Prevention Working Group. Different prevention projects may require different stakeholders. Select people that are the best fit for your state's needs. This group will be important in guiding the HAI efforts. The group will provide project leadership, guidance, and oversight. They will need to have a high level of commitment and agree to the purpose of the collaboration and the goals of all the partners.
Consider appointing a Chair and Co-chair to assist in creating aims, content, and measurement strategies. These appointees may delegate functions to working groups, individuals, or subcommittees.
Good candidates representing various entities with diverse expertise make the most successful advisory groups. Consider formalizing the group's structure (i.e., a charter or a memorandum of understanding)—including leadership (Chair, Co-Chair), operating rules, other policies (e.g., conflicts of interest, financial relationships), etc.
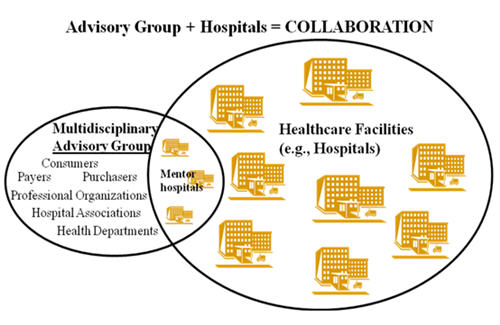
*Not all hospitals participating in the Collaborative should be part of the Multidisciplinary Advisory Group – just the 2-3 mentor hospitals
The more people involved in an advisory group, the greater the number of communications and coordination needed. Weigh the advantages of adding members to your group; maintain a group large enough to provide broad views, but small enough to be manageable. The average advisory group ranges from eight to twelve members, depending on the structure and resources available.
Larger Group:
- More resources
- More knowledge
- More connections
- More ideas
Smaller Group:
- Easier to manage
- Easier to reach consensus
- Less conflict
Suggestions for defining what is expected from the advisory group's members and their needed degree of commitment:
- Lay out the mission and purpose of collaboration
- Discuss milestones and appropriate timelines
- Review members’ roles and contributions
- Set norms for:
- Participation
- Communication
- Decision-making
- Meetings
Get things in writing:
Example commitment letter templates:
(Insert organization name) is pleased to support (the XX Collaborative) in its mission to prevent healthcare-associated infections. We want the Collaborative to build on individual strengths, where all members may participate as appropriate, and where collective efforts knit together to achieve the desired outcomes. (Insert organization name) understands that this will take time, and we agree to support the planning and subsequent implementation activities needed to make the Collaborative successful.
(Insert name of person or office title) will serve as a representative to the (Collaborative, Interim Committee, Subcommittee, etc.). In this capacity, (insert name of person or office title) can devote (anticipated # of hours/month or % of time) to these activities. As the Collaborative representative, (insert name of person or office title) is authorized to act on behalf of (insert organization name) to (list areas of authority for making decisions, committing resources, etc. Note limits, if any).
As a collaborator, (insert organization name) also commits the following resources (include some or all of these listed – or others – as appropriate) to the success of this endeavor:
- Connections/Networks
- Expertise
- Funds
- Committee or project leadership
- In-kind administrative support
- In-kind technical support
(Insert organization name) looks forward to working with the Collaborative and our other colleagues in this important prevention effort.
Develop a strategy to identify, recruit, and enroll participating hospitals. Initial contact may be with administration or hospital leadership (i.e., CEO, CMO).
Present the facts in order to obtain hospital buy-in. The positives:
- The prevention of HAIs are best pursued and served through a collaboration, rather than through individual efforts.
- HAI prevention provides immediate and long-range results for the public, government, and other beneficiaries.
- The hospital's participation is likely to have significant impact because of the collaboration effort.
Participating Healthcare Facilities
Ensure that participating healthcare facilities share in your commitment. Participating Healthcare Facilities:
- Should be committed and enthusiastic about prevention and able to identify local champion(s).
- Encourage active support and engagement from hospital leadership (e.g., CEO, CMO, CNO, CQO).
- Seek and support ideas from all sources (e.g., housekeeping, transport).
- Be willing to communicate and share ideas, including a willingness to participate in the measurement system and share data with a central coordinator.
- Must be able to provide letters of support and permission to use data.
Letters of support:
We at ABC Hospital are pleased to register our support for the XX Collaborative. This Collaborative represents a key opportunity for prevention of healthcare-associated infections (specify infection target here) in our community. As a participating hospital, we agree to… X, Y, Z… Thank you for your active pursuit of these goals.
We at ABC Hospital agree to be active participants in the XX Collaborative… to learn from each other…to:
- Designate a primary (and alternate) point of contact
- Appoint/elect a clinical champion (passionate about XX infection target)
- Obtain executive/leadership commitment
- Devote necessary resources for participation
- Help develop an intervention package to prevent (specify) infections and implement it in our facility
- Identify setting-specific barriers and challenges to implementation
- Identify workable and practical solutions to those barriers
- Use the National Healthcare Safety Network (NHSN) to uniformly collect outcomes
- Report (specify) infection rates and other data to NHSN
- Participate in all learning activities of the Collaborative, including face to face meetings, regular conference calls and online discussions, and share experiences and questions about infection prevention
The Collaborative should, at a minimum, include core prevention strategies. Supplemental prevention strategies also may be used. Hospitals should not be excluded from participation if they already have ongoing interventions using supplemental prevention strategies. Project Coordinators should carefully track which prevention strategies are being used by participating facilities.
Core Prevention Strategies
- High levels of scientific evidence
- Demonstrated feasibility
Supplemental Prevention Strategies
- Some scientific evidence
- Variable levels of feasibility
Meetings
Bring the entire team together to meet about the significant events in the ongoing collaboration. Before each meeting, keep the following things in mind:
Begin with a clearly defined purpose:
Decide on goals.
- Have a decision-making process that the group will use.
- Devise a means for meeting measurement (i.e. agenda development, meeting facilitation, minutes, etc.).
- Anticipate resources needed and who will provide them.
Share learning/communication and feedback:
- Send out notice of meetings (with reminders 1 week and, followed by 24-hours, in advance.
- Include agenda in pre-meeting communications, if possible.
- Record and distribute meeting notes soon after the meeting, preferably within 1 week (including a review of action items, assignments, and due dates; times/schedule for the next meeting, etc.).
You will need to consider the following factors and how each may apply specifically to your needs:
- Frequency (weekly, monthly, quarterly, annual)
- Format (face-to-face, web, teleconference – let form follow function)
Advisory Group
- Quarterly meetings (more in the beginning to facilitate engagement and progress)
- Face-to-face at first with alternating formats as appropriate/needed
Participating Healthcare Facilities (e.g., Hospitals)
- Weekly/bi-weekly at first, monthly to follow; continue with bi-weekly meetings if group can commit time and resources
- Face-to-face at first with alternating formats as appropriate/needed
- Try to eliminate meeting overlap if possible
Measurement
Measurement allows us to see what we’ve accomplished as well as what may be improved so that we can develop next steps.
Collaboration Metrics:
- Select measurement system (e.g., NHSN)
- Demonstrate willingness of facilities to participate in measurement system and share data with a central coordinator (i.e., letters of commitment)
- Demonstrate regular feedback of outcome data to participating facilities, to include a comparison of their individual performance to aggregate performance of others
If you choose to use NHSN, consistency with NHSN definitions is required. Evaluate prevention practices using core questions from CDC (infection toolkits). You must conduct surveys at designated time periods/intervals (i.e., baseline and 6-12 months into collaboration). Communicate the results of all feedback in order to share all lessons learned.
Goals, Objectives, and Action Steps
"The goal is where you want to be. The objectives are the steps needed to get there."
- Be "SMART": Specific – Measurable – Attainable – Relevant – Timely
- Evaluate using standardized questions and tools (i.e., NHSN and CDC toolkits)
- If possible, begin by conducting a needs assessment as a tool for planning
- Identify goals and targets
- Define the "who", "what", "when", "why", and "how"
- Evaluate both process and outcome measures
- Process: how have specific prevention measures been implemented (i.e., compliance with hand hygiene, insertion practices – available in NHSN)
- Outcome: what was the impact of the program and what were the program effects (i.e., a reduction in infection rates using NHSN)
Communicate and provide the results of feedback (shared learning) – Project Coordinators also should keep track of participating hospitals’ progress (i.e., changes in policies/procedures).
Communication Strategy: How to sustain momentum
Collaboration Metrics:
- Demonstrate face-to-face meetings
- Demonstrate regularly scheduled teleconferences between face-to-face meetings
- Demonstrate other supportive communication infrastructure for regular sharing between participants
Multimodal communication is best and information can be provided by a variety of means:
- Instant messaging/group chats
- Listservs
- Web (i.e., centrally managed site/bulletin boards)
- Newsletters
- Meeting minutes
- Memos/letters/faxes
- Teleconference/Videoconference
- Face-to-face meetings
Successful prevention collaboratives are dependent upon mechanisms to facilitate sharing of information and data among participating facilities. Real-time communication via multiple channels is recommended. Provide feedback of data/results as soon as available. There should be many options for feedback using NHSN as standardized tool.
Successful prevention collaboratives have standardized and uniform outcome measures that allow sharing of progress among participants and tracking aggregate group progress. Demonstrate regular feedback of outcome data to participating facilities, to include a comparison of their individual performance to aggregate performance of others. NHSN data can be exported to various other programs for review, analysis, and sharing.
Effective communication strategies require innovation but not re-invention. Spend your time wisely. Use proven methods to achieve communication goals. Maintain ongoing measurement and provide relevant and continuous feedback. Measure over time. Test many times and ways before implementation. Provide transparency. (See www.ihi.org/IHI)
Twenty Factors Influencing Collaboration Success*
Factors Related to the ENVIRONMENT
- History of collaboration or cooperation in the community
- Collaborative group seen as a legitimate leader in the community
- Favorable political and social climate
Factors Related to MEMBERSHIP CHARACTERISTICS
- Mutual respect, understanding, and trust
- Appropriate cross section of members
- Members see collaboration as in their self-interest
- Ability to compromise
Factors Related to PROCESS and STRUCTURE
- Members share a stake in both process and outcome
- Multiple layers of participation
- Flexibility
- Development of clear roles and policy guidelines
- Adaptability
- Appropriate pace of development
Factors Related to COMMUNICATION
- Open and frequent communication
- Established informal relationships and communication links
Factors Related to PURPOSE
- Concrete, attainable goals and objectives
- Shared vision
- Unique purpose
Factors Related to RESOURCES
- Sufficient funds, staff, materials, and time
- Skilled leadership
*From Collaboration: What Makes It Work, by Paul Mattessich, PhD, Marta Murray-Close, BA, & Barbara Monsey, MPH.
Four Keys to Collaboration Success by Carol Lukas and Rebecca Andrews
Additional Resources:
Quality Improvement Collaboratives Are Popular "There's no need to re-create the wheel."
Health Disparities Collaborative (HRSA)
Institute for Clinical Systems Improvement
Institute for Healthcare Improvement Breakthrough Collaboratives
Northern New England Cardiovascular Disease Study Group
Pittsburgh Regional Healthcare Initiative
Vermont-Oxford Neonatal Network
Wisconsin Collaborative on Healthcare Quality
Steps for Success
Summary
This Collaboration Primer is a framework for collaboration— focus and flexibility are key. Not every state/hospital is going to do the same thing—the more you can harmonize the collaboration, the richer the shared learning.
States should learn from one another and share their experiences.
For more information:
www.cdc.gov/hai/recoveryact e-mail: DHQPHAIARRA@cdc.gov
Contact Us:
- DHQP
NCPDCID
Mailstop A-07
Centers for Disease Control and Prevention
Atlanta, GA 30333 - Telephone: (404) 639-4000
- DHQPHAIARRA@cdc.gov


