Preterm Birth
Each year, preterm birth affects more than 500,000 babies—that's 1 of every 8 infants born in the United States. Preterm birth is the birth of an infant prior to 37 weeks gestation. It is the most frequent cause of infant death, the leading cause of long-term neurological disabilities in children, and costs the U.S. health care system more than $26 billion each year. Learn more about preterm birth.
The developing baby goes through important growth during the final weeks and months of pregnancy. Many organ systems, including the brain, lung, and liver, need the final weeks of pregnancy to fully develop. Even infants born slightly preterm are at greater risk than full-term infants, but the earlier the delivery, the more likely the risk of serious disability or even death. Adverse health outcomes related to preterm birth include cerebral palsy, developmental delay [PDF - 64KB], and vision [PDF - 118KB] and hearing impairment. Preterm births also may cause heavy emotional and economic burdens for families.
Causes and Risk Factors
The causes of preterm births are numerous, complex, and remain poorly understood. Psychosocial, biological, and clinical factors all affect a woman’s risk of preterm birth. In some cases, preterm birth occurs spontaneously, often without a known underlying cause. Other times, health care providers choose to deliver infants early to protect the health of the mother or the baby. CDC scientists, in collaboration with state health departments, university researchers, health care providers, and community organizations are working to understand the multiple reasons for preterm births and advance new strategies for prevention. Learn more about CDC’s preterm birth projects.
One of the most important risk factors for delivering a baby preterm is having had a baby born preterm before. This means that women who have had a preterm birth and are thinking about another pregnancy should discuss the pregnancy with their health care provider. In addition, having more than one baby at a time (i.e., twins or triplets or the use of Assisted Reproductive Technology) is associated with higher health risks for both mothers and infants, including higher rates of Caesarean section, prematurity, low birth weight, and infant disability or death.
Preterm births occur more often among certain racial and ethnic groups. Infants of non-Hispanic black mothers are at greater risk of being born preterm. They are more than 1.5 times more likely to be born preterm compared with infants of non-Hispanic white women. In addition, preterm-related infant mortality rates vary by maternal race and ethnicity. In 2007, preterm-related mortality rates were 3.4 times higher for infants of non-Hispanic black mothers (5.99 per 1,000 live births) than for non-Hispanic white mothers (1.78).
Total and Preterm-Related* Infant Mortality Rates by
Race and Ethnicity of Mother: United States, 2007
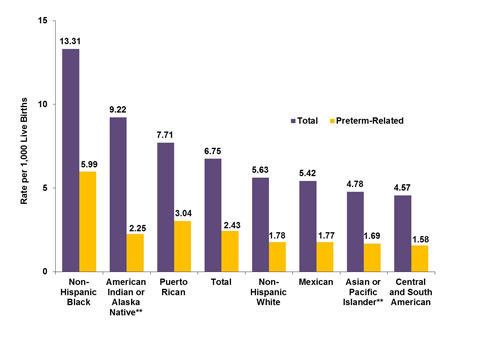
* Preterm-related deaths are those where the infant was born preterm (before 37 completed weeks of gestation) with the underlying cause of death assigned to one of the following ICD-10 categories: K550, P000, P010, P011, P015, P020, P021, P027, P070-P073, P102, P220-P229, P250-279, P280, P281, P360-P369, P520-P523, P77.
** Includes persons of Hispanic and Non-Hispanic origin.
Source: Infant mortality statistics from the 2007 period linked birth/infant death data set [PDF-750] NVSR. 2011;59(6).
A recent report from CDC’s National Center for Health Statistics [PDF-162MB] shows a small but encouraging drop in the preterm birth rate, from 12.8% in 2006 to 12.3% in 2008. While this is encouraging, levels remain higher than at any point in the 1980s and 1990s. Most of this increase has been among late preterm births (infants born between 34–36 weeks gestation). The problem of early preterm birth (< 32 weeks gestation) remains a public health challenge; more than 50% of all infant deaths in the United States were born < 32 weeks gestation. CDC continues to explore strategies to reduce the national burden of infant mortality and reduce racial and ethnic disparities. Ongoing reviews of infant death data by CDC researchers continue to demonstrate that preterm-related deaths account for more than 33% of all deaths during the first year of life, and more infants die from preterm causes than from any other cause.
Reduce the Risk
Preventing preterm birth remains a challenge; however, clinical research continues to identify ways to help women reduce the number of babies being born too early. For example, a progesterone medication (17-alpha hydroxyprogesterone caproate, or 17P) may prevent preterm birth among women who have had a prior preterm birth. The U.S. Food and Drug Administration (FDA) approved hydroxyprogesterone caproate injection (Makena™) to reduce the risk of preterm delivery in pregnant women with a history of delivering early. It is not intended for use in women carrying more than one baby or women with other risk factors for preterm birth. For more information on FDA’s approval, see their press announcement. Learn more about this and other drugs, including whether they are safe for use during pregnancy.
The Contribution of Preterm Birth to Infant Mortality Rates in the United States (Healthcare Providers and Consumers) Dr. William Callaghan describes the findings from a CDC study that sought to understand how preterm birth contributes to infant mortality rates in the United States. This study found that preterm birth was the leading cause of all infant deaths in 2002.
Contact Us:
- Centers for Disease Control and Prevention
1600 Clifton Rd
Atlanta, GA 30333 - 800-CDC-INFO
(800-232-4636)
TTY: (888) 232-6348 - New Hours of Operation
8am-8pm ET/Monday-Friday
Closed Holidays - cdcinfo@cdc.gov



