Are Stem Cells the Next Frontier for Diabetes Treatment?
Charles A. Goldthwaite, Jr., Ph.D.
Diabetes is a devastating disease that affects millions of people worldwide. The major forms of the disease are type 1 and type 2 diabetes. In type 1 diabetes, the body's immune system aberrantly destroys the insulin-producing beta cells (b-cells) of the pancreas. Type 2 diabetes, the more common form, is characterized both by insulin resistance, a condition in which various tissues in the body no longer respond properly to insulin action, and by subsequent progressive decline in b-cell function to the point that the cells can no longer produce enough additional insulin to overcome the insulin resistance. Researchers are actively exploring cell replacement therapy as a potential strategy to treat type 1 diabetes, because patients with this disease have lost all or nearly all b-cell function. However, if a safe and cost-effective means for replenishing b-cells were developed, such a treatment strategy could also be useful for the larger population with type 2 diabetes. One of the major challenges of cell replacement therapy is the current insufficient supply of b-cells from human organ donors. This article focuses on stem cells as potential sources for deriving new b-cells.
Diabetes: A Critical Health Issue for the 21st Century
According to the International Diabetes Federation, diabetes currently affects 7% of the world's population — nearly 250 million individuals worldwide.1 This total is expected to rise to 380 million by 2025 as a result of aging populations, changing lifestyles, and a recent worldwide increase in obesity. Although projections for increases in diabetes prevalence suggest that the greatest percentage gains will occur in Asia and South America,2,3 all nations will experience a rising disease burden. According to the National Diabetes Fact Sheet, which was compiled using information from the Centers for.
According to the National Diabetes Fact Sheet, which was compiled using information from the Centers for Disease Control and Prevention and other Federal and non-Federal organizations, 20.8 million U.S. children and adults have diabetes (6.2 million of whom are currently undiagnosed).4 An estimated 54 million Americans have "pre-diabetes", a condition defined by blood glucose levels that are above normal but not sufficiently high to be diagnosed as diabetes. In 2005, 1.5 million new cases of diabetes were diagnosed in Americans aged 20 years or older.4 If present trends continue, 1 in 3 Americans (1 in 2 minorities) born in 2000 will develop diabetes in their lifetimes.5
Diabetes is currently the sixth leading cause of death in the U.S.4 It is associated with numerous health complications, including increased risk for heart disease, stroke, kidney disease, blindness, and amputations. In 2007, the total annual economic cost of diabetes was estimated to be $174 billion dollars.6 Direct medical expenditures account for the vast majority of this total ($116 billion), although lost productivity and other indirect costs approached nearly $58 billion. The American Diabetes Association estimates that one out of every 10 health care dollars currently spent in the U.S. is used for diabetes and its complications.6
While diabetes can be managed, at present it cannot be cured. As a result, it is a lifelong and often disabling disease that can severely impact the quality of life of those who are afflicted. Based on several recent discoveries, however, researchers have begun to ask if a new treatment approach is on the horizon — can stem cells that are derived from adult or embryonic tissues generate new pancreatic b-cells to replace those that have failed or been destroyed? Cell replacement therapy is one of many research avenues being pursued as a potential treatment strategy for type 1 diabetes. The strategy may also have implications for ameliorating type 2 diabetes. One of the key obstacles to advancing such therapy is the current inadequate supply of cadaveric donor pancreata as a source of cells for transplantation. Additionally, it is not currently possible to induce a patient's own cells to regenerate new b-cells within the body. Thus, researchers are actively investigating potential sources of new beta cells, including different types of stem cells. This article will focus on the various types of stem cells that are candidates for use in pancreatic regeneration and will discuss the challenges of using such cells as therapy for diabetes.
Defining Diabetes
Diabetes results from the body's inability to regulate the concentration of sugar (glucose) in the blood. Blood glucose concentration is modulated by insulin, a hormone produced by pancreatic b-cells and released into the bloodstream to maintain homeostasis. In healthy individuals, b-cells counteract sharp increases in blood glucose, such as those caused by a meal, by releasing an initial "spike" of insulin within a few minutes of the glucose challenge. This acute release is then followed by a more sustained release that may last for several hours, depending on the persistence of the elevated blood glucose concentration. The insulin release gradually tapers as the body's steady-state glucose concentration is reestablished. While postprandial insulin release is stimulated by factors other than blood glucose, the blood sugar concentration is the major driver. When the b-cells fail to produce enough insulin to meet regulatory needs, however, the blood glucose concentration rises. This elevated concentration imposes a metabolic burden on numerous body systems, dramatically increasing the risk of premature cardiovascular disease, stroke, and kidney failure. Moreover, the risk for certain diabetes-related complications increases even at blood glucose concentrations below the threshold for diagnosing diabetes.
At present, there is no cure for diabetes.b-cell failure is progressive7; once the condition is manifest, full function usually cannot be restored. Those with type 1 diabetes require daily insulin administration to survive. Persons with type 2 diabetes must control their elevated blood glucose levels through various means, including diet and exercise, oral antihyperglycemic (blood glucose-lowering) drugs, and/or daily insulin shots. Most people who live with type 2 diabetes for a period of time will eventually require insulin to survive.
As noted earlier, there are different forms of diabetes. Type 1 diabetes results when a person's immune system mistakenly attacks and destroys the b-cells. This type of diabetes was once referred to as "juvenile-onset diabetes," because it usually begins in childhood. Type 1 diabetes accounts for 5–10% of diabetes cases, and people with type 1 diabetes depend on daily insulin administration to survive.
By contrast, type 2 diabetes is a metabolic disorder that results from a decline in b-cell function combined with insulin resistance, or the inability to use insulin effectively in peripheral tissues such as the liver, muscles, and fat.8 Onset is associated with genetic factors and with obesity, and type 2 diabetes disproportionately affects certain minority groups. 3 Unlike type 1 diabetes, type 2 is largely preventable. Numerous studies have suggested that the environmental and behavioral factors that promote obesity (e.g., a sedentary lifestyle, a high-calorie diet) have profoundly influenced the recent rise in the prevalence of type 2 diabetes.9 This trend suggests that type 2 diabetes will continue to be a major health care issue.
The Case for Stem Cells
There is great interest in developing strategies to expand the population of functional b-cells. Possible ways to achieve this include physically replacing the b-cell mass via transplantation, increasing b-cell replication, decreasing b-cell death, and deriving new b-cells from appropriate progenitor cells.10 In 1990, physicians at the Washington University Medical Center in St. Louis reported the first successful transplant of donor-supplied pancreatic islet tissue (which includes b-cells; see below) in humans with type 1 diabetes.11 By the end of the decade, many other transplants had been reported using various protocols, including the widely-known "Edmonton protocol" (named for the islet transplantation researchers at the University of Alberta in Edmonton).12-14 This protocol involves isolating islets from the cadaveric pancreatic tissue of multiple donors and infusing them into the recipient's portal vein. However, the lack of available appropriate donor tissue and the strenuous regimen of immunosuppresive drugs necessary to keep the body from rejecting the transplanted tissue limit the widespread use of this approach. Moreover, the isolation process for islets damages the transplantable tissue; as such, 2–3 donors are required to obtain the minimal b-cell mass sufficient for transplantation into a single recipient.13 While these strategies continue to be improved, islet function declines relatively rapidly post-transplant. For example, a long-term follow-up study of Edmonton transplant patients indicated that less than 10% of recipients remained insulin-independent five years after transplant.15
These challenges have led researchers to explore the use of stem cells a possible therapeutic option. Type 1 diabetes is an appropriate candidate disease for stem cell therapy, as the causative damage is localized to a particular cell type. In theory, stem cells that can differentiate into b-cells in response to molecular signals in the local pancreatic environment could be introduced into the body, where they would migrate to the damaged tissue and differentiate as necessary to maintain the appropriate b-cell mass. Alternately, methods could be developed to coax stem cells grown in the laboratory to differentiate into insulin-producing b-cells. Once isolated from other cells, these differentiated cells could be transplanted into a patient. As such, stem cell therapy would directly benefit persons with type 1 diabetes by replenishing b-cells that are destroyed by autoimmune processes, although it would still be necessary to mitigate the autoimmune destruction of b-cells. The strategy would also benefit those with type 2 diabetes to a lesser extent by replacing failing b-cells, although the insulin resistance in peripheral tissues would remain present. As discussed in the following sections, however, debate continues about potential source(s) of pancreatic stem cells.
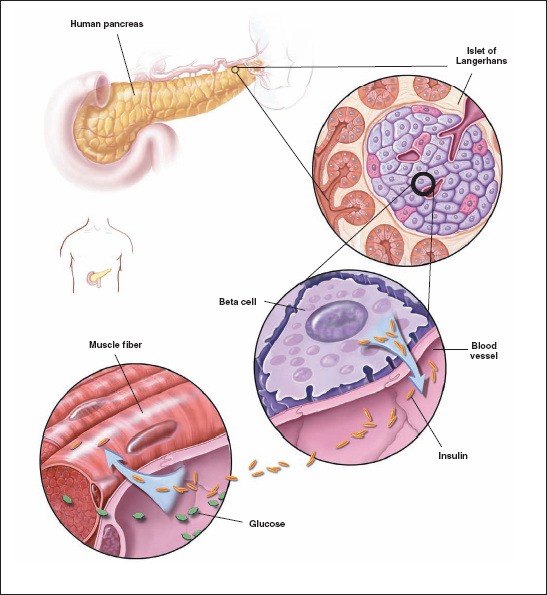
Figure 7.1.The pancreas is located in the abdomen, adjacent to the duodenum (the first portion of the small intestine). A cross-section of the pancreas shows the islet of Langerhans which is the functional unit of the endocrine pancreas. Encircled is the beta cell that synthesizes and secretes insulin. Beta cells are located adjacent to blood vessels and can easily respond to changes in blood glucose concentration by adjusting insulin production. Insulin facilitates uptake of glucose, the main fuel source, into cells of tissues such as muscle.
© 2001 Terese Winslow, Lydla Kibluk
Searching for the "Pancreatic Stem Cell"
The pancreas is a complex organ made up of many cell types. The majority of its mass is comprised of exocrine tissue, which contains acinar cells that secrete pancreatic enzymes into the intestine to aid in food digestion. Dispersed throughout this tissue are thousands of islets of Langerhans, clusters of endocrine cells that produce and secrete hormones into the blood to maintain homeostasis. The insulin-producing b-cell is one type of endocrine cell in the islet; other types include alpha cells (a-cells), which produce glucagon, gamma cells (g-cells), which produce pancreatic polypeptide, and delta cells (d-cells), which produce somatostatin.
Each of these cell types arises from a precursor cell type during the process of development. Therefore, the key step for using stem cells to treat diabetes is to identify the precursor cell(s) that ultimately give rise to the b-cell. However, generating these cells is more complex than simply isolating a hypothetical "pancreatic stem cell." Experiments have indicated that embryonic and adult stem cells can serve as sources of insulin-secreting cells,16 leading researchers to explore several avenues through which stem cells could feasibly be used to regenerate b-cells. However, many challenges must be addressed before a particular cell type will become established for this approach.
The human body has inherent mechanisms to repair damaged tissue, and these mechanisms remain active throughout life. Thus, there is reason to speculate that the adult pancreas may be aided by some type of regenerative system that replaces worn-out cells and repairs damaged tissue in response to injury. Such a system could theoretically be supported by precursor or stem cells, located in the endocrine pancreas or elsewhere, which could be coaxed to differentiate in response to select molecular or chemical stimuli. But do these cells exist? If so, how can they be recognized, isolated, and cultured for therapeutic use? How quickly could they produce sufficient numbers of b-cells to offset damage caused by diabetes processes? Alternately, what if cells that have the capability to regenerate b-cells exist in the body but are committed to differentiate into some other cell type? Could embryonic stem (ES) cell lines, which have the potential to develop into cells from all lineages, then be derived in vitro and be directed to differentiate into b-cells? These questions will be explored in the following sections, which review the types of candidate stem cells for diabetes.
Are Adult Pancreatic Stem Cells Present in the Pancreas?
Whether b-cell progenitors are present in the adult pancreas is a controversial topic in diabetes research. Several recent studies in rodents have indicated that the adult pancreas contains some type of endocrine progenitor cells that can differentiate toward b-cells.16 However, researchers have not reached consensus about the origin of the bona fide pancreatic stem cell (if it exists) or the mechanism(s) by which b-cells are regenerated.17 For example, a pivotal study by Dor and colleagues used genetic lineage tracing in adult mice to determine how stem cells contribute to the development of b-cells.18 Their analysis indicated that new b-cells arise from pre-existing ones, rather than from pluripotent stem cells, in adult mice. As such, the authors noted that b-cells can proliferate in vivo, thereby "cast[ing] doubt on the idea that adult stem cells have a significant role in beta-cell replenishment." Soon after this report was published, Seaberg and coworkers reported the identification of multipotent precursor cells from the adult mouse pancreas.19 These novel cells proliferated in vitro to form colonies that could differentiate into pancreatic α-, b-, and δ-cells as well as exocrine cells, neurons, and glial cells. Moreover, the beta-like cells demonstrated glucose-dependent insulin release, suggesting possible therapeutic application to diabetes. Several subsequent studies have also reported the existence of pancreatic stem/precursor cells in vitro or in vivo.20-22 One recent report suggests that such cells exist in the pancreatic ductal lining and can be activated autonomously in response to injury, increasing the b-cell mass through differentiation and proliferation.23
The study of pancreatic regeneration continues to evolve, and many claims have been made regarding cells believed to be involved in the process. In the last decade, reports have described various putative pancreatic stem cells embedded in the pancreatic islets,24,25 pancreatic ducts,23,26 among the exocrine acinar cells,20,21 and in unspecified pancreatic locales19,27 in rodent models, as well as from human adult pancreatic cell lines,28 islet tissue,29 and non-islet tissues discarded after islets have been removed for transplantation.30-32 These cells are identified by the presence of one or more cell-surface proteins, or markers, known to be associated with a particular stem cell lineage. However, these studies illustrate several challenges shared by all researchers who seek to identify the "pancreatic stem cell". First, all potential stem cell candidates identified to date are relatively rare; for instance, the precursor cells identified by Seaberg are present at the rate of 1 cell per 3,000–9,000 pancreaccells.19 Because there are so few of these putative stem cells, they can be difficult to identify. Additionally, the choice of marker can select for certain stem cell populations while possibly excluding others. Interestingly, the progenitor cells identified in the Seaberg study lacked some known b-cell markers such as HNF3b, yet they were able to generate b-cells. Thus, a hypothetical experiment that used only HNF3b as a marker for b-cell differentiation would likely not identify this stem cell population. Moreover, techniques used to study the pancreatic tissue, such as the genetic lineage technique of Dor,et.al. could possibly interfere with the generation of new b-cells from stem or precursor cells.33
As such, the possibility remains that b-cells could be regenerated by differentiation of endogenous stem cells, by proliferation of existing b-cells, or a combination of the two mechanisms.
Further research to elucidate conditions under which b-cells can proliferate may help to develop new therapeutic approaches. For example, several advances have recently been made from studies of pregnancy and pregnancy-related diabetes (gestational diabetes) in mice. During pregnancy, pancreatic islet cells normally expand in number to meet increased metabolic demands. Researchers have found that the protein HNF4-alpha helps increase b-cell mass, and that pregnancy-related decreases in levels of another protein, menin, also enable b-cell proliferation.34,35 Insights may also arise from research on another organ, the liver. Unlike the pancreas, the liver has an inherently high capacity for regeneration. New strategies for inducing pancreatic islet cell growth may emerge from knowledge of how liver cells develop from progenitor cells during early development such that the resulting adult organ retains substantial regenerative capacity.36 In another research avenue, scientists are exploring whether it may be possible to redirect adult pancreatic cells in the body to change from their original cell type into b-cells.
Other Potential Sources of Stem Cells Derived from Adult Cells
Furthermore, various reports have also described putative stem cells in the liver, spleen, central nervous system, and bone marrow that can differentiate into insulin-producing cells.17 While it is possible that such pathways may exist, these results are currently under debate within the research community. In another research avenue, scientists recently reported that differentiated cells, including adult human skin cells, can be genetically "reprogrammed" to revert to a pluripotent state, resembling that of embryonic stem (ES) cells.37 The researchers refer to these cells as induced pluripotent stem (iPS) cells. Their method involved introducing a defined set of genes into the differentiated cells. This approach may facilitate the establishment of human iPS cell lines from patients with specific diseases that could be used as research tools. This technique, or variations of it, may also one day allow patient-specific stem cells to be generated for use in stem cell-based therapies. However, the genes used for reprogramming were introduced into the cells using a virus-based method, which could have adverse clinical effects. If, however, safe alternate methods based on this research can be developed for reprogramming cells, then iPS cells may lead to novel, personalized therapies.
The challenges associated with identifying and isolating adult "pancreatic stem cells" has led some researchers to explore the use of ES cells as a source of insulin-producing cells. Several factors make ES cells attractive for this application.33 First, given the complexity of pancreatic tissue, identified b-cell precursors would likely be difficult to isolate from the adult pancreas. If isolated, the cells would then need to be replicated ex vivo while keeping them directed toward a b-cell lineage. Second, protocols to grow and expand mature b-cells in culture have met with technical challenges. ES cells, which are pluripotent cell lines (they can give rise to all cell types of the embryo) that can be induced to develop into various lineages based on culture conditions, may therefore represent a future option for b-cell regeneration.
To date, several human ES cells lines have been successfully derived.38-40 While these cell lines serve as resources for exploring the mechanisms of development, their potential use in a clinical setting is limited by several factors, most notably ethical concerns and the risk of teratoma development. (For a more detailed discussion of the scientific challenges associated with clinical application of ES cells, see Chapter 6, "Mending a Broken Heart: Stem Cells and Cardiac Repair," p.59). In addition, researchers are only beginning to unlock the myriad factors that come into play as a once-pluripotent cell differentiates into a unipotent cell, one that can contribute to only one mature cell type.41 For example, several recent reports indicate that mouse42 and human43 ES cells can be successfully differentiated into endodermal cells, the precursors of pancreatic cells. In addition, insulin-producing cells have been derived from mouse44,45 and human46 ES cells.
However, it should be noted that directed differentiation of ES cells toward the b-cell has not been reported. Beta cells appear relatively late during embryonic development, suggesting that their presence involves the temporal control of a considerable number of genes. Moreover, the creation of patient-specific, stem cell-derived b-cells for transplantation requires genetic matching to lessen the immune response. Generating immune-matched tissues requires the therapeutic cloning of human ES cells, which has not been accomplished to date. A fraudulent claim to the contrary in 2005 by South Korean researcher Woo Suk Hwang47 ignited international controversy within the scientific community48 and illustrated the scientific and ethical challenges of using ES cells as a source of transplant tissue. Despite current gaps in knowledge, researchers recognize the potential of ES cells as sources of specialized cells such as the b-cell, and the study of ES cells provides insight into the processes that govern differentiation and specialization.
Clinical Challenges
Clearly, using stem cells to treat diabetes will require additional knowledge, both in the laboratory and in the clinic. This section will suggest several envisioned approaches for stem-cell derived diabetes therapies and discuss key considerations that must be addressed for their successful application.
Contingent upon the development of appropriate protocols, stem cells could theoretically be used to treat diabetes through two approaches.49 Both strategies would require the isolation and in vitro expansion of a homogenous population of b-cell precursor cells from appropriate donor tissue. Once a population of these cells has been generated, they could either 1) be induced to differentiate into insulin-producing cells in vitro and then be transplanted into the diabetic patient's liver, or 2) be injected into the circulation along with stem cell stimulators, with the hope that the cells will "home in" to the injured islets and differentiate into a permanent self-renewing b-cell population.
Because type 1 diabetes is an autoimmune disease, controlling the autoimmune response is critical to the success of any potential stem cell-based therapy. Type 1 diabetes is characterized by the action of b-cell-specific, autoreactive T-cells. Even if the regenerative properties of the pancreas remain functional, the continued presence of these T-cells effectively counteracts any endogenous repair and would likely decimate populations of newly-regenerated or transplanted insulin-producing cells. However, the autoimmune response has been successfully averted in non-obese diabetic mice either by using anti-T-cell antibodies to eliminate the majority of the autoreactive cells50 or by transplanting bone marrow from a diabetes-resistant donor (with a sublethal dose of irradiation) into the diabetic animal.51-53 Both strategies appear to enable the replenishment of insulin-secreting cells and the eventual restoration of normal blood glucose levels, although the process requires weeks to months and may necessitate additional therapy. Other strategies being explored include altering the immune tolerance through the use of monoclonal antibodies,54 proteins,55 and oligonucleotides.56
Other clinical challenges, including safety, tracking of the stem cells, delivery of the cells to the targeted tissue within a clinically relevant time frame (for transplanted cells), identification of ways to promote long-term survival and functioning of regenerated b-cells, ease of obtaining the cells, and cost, parallel those encountered with all applications of stem cell-based regenerative therapy. These issues must be addressed once the "pancreatic stem cell" population has been identified conclusively. Given current debate on this issue, the routine clinical application of stem-cell based regenerative therapy for the treatment of diabetes remains a future goal, albeit one with great potential.
As an additional source of information, an extensive discussion of research challenges and strategies for achieving the goal of cell replacement therapy for Type 1 diabetes is presented in Advances and Emerging Opportunities in Type 1 Diabetes Research: A Strategic Plan, available on the NIH web site at http://www2.niddk.nih.gov/AboutNIDDK/ResearchAndPlanning/Type1Diabetes/.
Conclusions
The results discussed in this article demonstrate the many challenges that must be addressed before stem cells can be used to regenerate islet tissue in persons with diabetes. Debate continues on the identification of the "pancreatic stem cell," and at present it is difficult to ascertain which cell type has the greatest potential for diabetes therapy. Moreover, modulating the autoimmune response in type 1 diabetes remains a significant challenge regardless of the type of cell that is transplanted, and it will also be important to address the insulin resistance in type 2 diabetes, as well as factors that contribute to obesity. However, diabetes is a disease with a major deficiency in the functioning of one type of cell, and there is potential of stem cells to treat type 1 diabetes and to improve the quality of life for those with type 2 diabetes. As researchers learn more about the mechanisms that govern stem cell programming, differentiation, and renewal, their ability to identify, isolate, and culture candidate stem cells will continue to improve. While stem cells can be currently considered a frontier for diabetes therapy, they may one day become its basis..
References
- International Diabetes Federation. Facts & figures: diabetes prevalence. http://www.idf.org/home/index.cfm?node=264. Accessed September 15, 2007.
- King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414-1431.
- Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001;414:782-787.
- Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2005.http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2005.pdf. Accessed April 24, 2008.
- Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290:1884-1890.
- American Diabetes Association. Economic costs of diabetes in the U.S. In 2007. Diabetes Care. 2008;31:596-615.
- UK Prospective Diabetes Study Group. Overview of 6 years’ therapy of type II diabetes: a progressive disease (UKPDS 16). Diabetes. 1995;44:1249-1258.
- Ferranninni E. Insulin resistance versus insulin deficiency in non-insulin-dependent diabetes mellitus: problems and prospects. Endocr Rev. 1998;19:477-490.
- Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. 1998;280:1371-1374.
- Lipsett M, Finegood DT. Beta-cell neogenesis during prolonged hyperglycemia in rats. Diabetes. 2001;51:1834-1841.
- Scharp DW, Lacy PE, Santiago JV, et al. Insulin independence after islet transplantation into patient. Diabetes. 1990(39):515-518.
- Ryan EA, Lakey JR, Paty BW, et al. Successful islet transplantation: continued insulin reserve provides long-term glycemic control. Diabetes. 2002;51:2148-2157.
- Ryan EA, Lakey JR, Rajotte RV, et al. Clinical outcomes and insulin secretion after islet transplantation with the Edmonton protocol. Diabetes. 2001;50:710-719.
- Shapiro AM, Lakey JR, Ryan EA, et al. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N Engl J Med. 2000;343:230-238.
- Ryan EA, Paty BW, Senior PA, et al. Five-year follow-up after clinical islet transplantation. Diabetes. 2005;54:2060-2069.
- Soria B, Bedoya FJ, Martin F. Gastrointestinal stem cells: I. Pancreatic stem cells. Am J Physiol Gastrointest Liver Physiol. 2005;289:G177-G180.
- Zulewski H. Stem cells with potential to generate insulin-producing cells in man. Swiss Med Wkly. 2006;136:647-654.
- Dor Y, Brown J, Martinez OI, Melton DA. Adult pancreatic beta-cells are formed by self-duplication rather than stem-cell differentiation. Nature. 2004;429:41-46.
- Seaberg RM, Smukler SR, Kieffer TJ, et al. Clonal identification of multipotent precursors from adult mouse pancreas that generate neural and pancreatic lineages. Nat Biotechnol. 2004;22:1115-1124.
- Baeyens L, De Breuck S, Lardon J, Mfopou JK, Rooman I, Bouwens L. In vitro generation of insulin-producing beta cells from adult exocrine pancreatic cells. Diabetologia. 2005;48:49-57.
- Minami K, Okuno M, Miyawaki K, et al. Lineage tracing and characterization of insulin-secreting cells generated from adult pancreatic acinar cells. Proc Natl Acad Sci USA. 2005;102:15116-15121.
- Lee CS, De Leon DD, Kaestner KH, Stoffers DA. Regeneration of pancreatic islets after partial pancreatectomy in mice does not involve the reactivation of neurogenin-3. Diabetes. 2006;55:269-272.
- Xu X, D'Hoker J, Stangé G, et al. Beta cells can be generated from endogenous progenitors in injured adult mouse pancreas. Cell. 2008;132:197-207.
- Guz Y, Nasir I, Teitelman G. Regeneration of pancreatic beta cells from intra-islet precursor cells in an experimental model of diabetes. Endocrinology. 2001;142:4956-4968.
- Zulewski H, Abraham EJ, Gerlach MJ, et al. Multipotential nestin-positive stem cells isolated from adult pancreatic islets differentiate ex vivo into pancreatic endocrine, exocrine, and hepatic phenotypes. Diabetes. 2001;50:521-533.
- Oshima Y, Suzuki A, Kawashimo K, Ishikawa M, Ohkohchi N, Taniguchi H. Isolation of mouse pancreatic ductal progenitor cells expressing CD133 and c-Met by flow cytometric cell sorting. Gastroenterology. 2007;132:720-732.
- Raimya VK, Maraist M, Arfors KE, Schatz DA, Peck AB, Cornelius JG. Reversal of insulin-dependent diabetes using islets generated in vitro from pancreatic stem cells. Nat Med. 2000;6:278-282.
- Tsang WG, Zheng T, Wang Y, et al. Generation of functional islet-like clusters after monolayer culture and intracapsular aggregation of adult human pancreatic islet tissue. Transplantation. 2007;83:685-693.
- Abraham EJ, Leech CA, Lin JC, Zulewski H, Habener JF. Insulinotropic hormone glucagon-like peptide-1 differentiation of human pancreatic islet-derived progenitor cells into insulin-producing cells. Endocrinology. 2002;143:3152-3161.
- Todorov I, Nair I, Ferreri K, et al. Multipotet progenitor cells isolated from human adult pancreatic tissue. Transplant Proc. 2005;37:3420-3421.
- Todorov I, Omori K, Pascual M, et al. Generation of human islets through expansion and differentiation of non-islet pancreatic cells discarded (pancreatic discard) after islet isolation. Pancreas. 2006;32:130-138.
- Bonner-Weir S, Taneja M, Weir GC, et al. In vitro cultivation of human islets from expanded ductal tissue. Proc Natl Acad Sci USA. 2000;97:7999-8004.
- Trucco M. Regeneration of the pancreatic beta cell. J Clin Invest. 2005;115:5-12.
- Gupta RK, Gao N, Gorski RK, et al. Expansion of adult beta-cell mass in response to increased metabolic demand is dependent on HNF-4alpha. Genes Dev. 2007;21:756-769.
- Karnik SK, Chen H, McLean GW, et al. Menin controls growth of pancreatic beta-cells in pregnant mice and promotes gestational diabetes mellitus. Science. 2007;318:806-809.
- Zaret KS. Genetic programming of liver and pancreas progenitors: lessons for stem-cell differentiation. Nat Rev Genet. 2008;9:329-340.
- Park IH, Zhao R, West JA, et al. Reprogramming of human somatic cells to pluripotency with defined factors. Nature. 2008;451:141-146.
- Thomson JA, Itskovitz-Eldor J, Shapiro SS, et al. Embryonic stem cell lines derived from human blastocysts. Science. 1998;282:1145-1147.
- Shamblott MJ, Axelman J, Wang S, et al. Derivation of pluripotent stem cells from cultured human primordial germ cells. Proc Natl Acad Sci USA. 1998;95:13726-13731.
- Cowan CA, Klimanskaya I, McMahon J, et al. Derivation of embryonic stem-cell lines from human blastocysts. N Engl J Med. 2004;350:1353-1356.
- Wagers AJ, Weissman IL. Plasticity of adult stem cells. Cell. 2004;116:639-648.
- Yasunaga M, Tada S, Torikai-Nishikawa S, et al. Induction and monitoring of definitive and visceral endoderm differentiation of mouse ES cells. Nat Biotechnol. 2005;23:1542-1550.
- D'Amour KA, Agulnick AD, Eliazer S, Kelly OG, Kroon E, Baetge EE. Efficient differentiation of human embryonic stem cells to definitive endoderm. Nat Biotechnol. 2005;23:1534-1541.
- Lumelsky N, Blondel O, Laeng P, Velasco I, Ravin R, McKay R. Differentiation of embryonic stem cells to insulin-secreting structures similar to pancreatic islets. Science. 2001;292:1389-1394.
- Soria B, Roche E, Berna G, Leon-Quinto T, Reig JA, Martin F. Insulin-secreting cells from embryonic stem cells normalize glycemia in streptozotocin-induced diabetic mice. Diabetes. 2000;49:157-162.
- Seguev H, Fishman B, Ziskind A, Shulman M, Itskovitz-Eldor J. Differentiation of human stem cells into insulin-producing cell clusters. Stem Cells. 2004;22:265-274.
- Hwang WS, Roh SI, Lee BC, et al. Patient-specific embryonic stem cells derived from human SCNT blastocysts. Science. 2005;308:1777-1783.
- Chong AS, Normile D. Stem cells: how young Korean researchers helped unearth a scandal. Science. 2006;311:22-25.
- Lechner A, Habener JF. Stem/progenitor cells derived from adult tissues: potential for the treatment of diabetes mellitus. Am J Physiol Endocrinol Metab. 2003;284:E259-E266.
- Ogawa N, List JF, Habener JF, Maki T. Cure of overt diabetes in NOD mice by transient treatment with anti-lymphocyte serum and exendin-4. Diabetes. 2004;53:1700-1705.
- Ikehara S, Ohtsuki H, Good RA, et al. Prevention of type 1 diabetes in nonobese diabetic mice by allogenic bone marrow transplantation. Proc Natl Acad Sci USA. 1985;82:7743-7747.
- Li H, Kaufman CL, Boggs SS, Johnson PC, Patrene KD, Ildstad ST. Mixed allogeneic chimerism induced by a sublethal approach prevents autoimmune diabetes and reverses insulitis in nonobese diabetic (NOD) mice. J Immunol. 1996;156:380-388.
- Zorina TD, Subbotin VM, Bertera S, et al. Distinct characteristics and features of allogeneic chimerism in the NOD mouse model of autoimmune diabetes. Cell Transplant. 2002;11:113-123.
- Chatenoud L, Primo J, Bach J-F. CD3 antibody-induced dominant self tolerance in overtly diabetic NOD mice. J Immunol. 1997;158:2947-2954.
- Zheng XX, Sanchez-Fueyo A, Sho M, Domenig C, Sayegh MH, Strom TB. Favorably tipping the balance between cytopathic and regulatory T cells to create transplantation tolerance. Immunity. 2003;19:503-514.
- Machen J, Harnaha J, Lakomy R, Styche A, Trucco M, Giannoukakis N. Antisense oligonucleotides down-regulating costimulation confer diabetes-preventive properties to nonobese diabetic mouse dendritic cells. J Immunol. 2004;173:4331-4341.
 Chapter6 | Table of Contents | Chapter8
Chapter6 | Table of Contents | Chapter8 