Two Drugs and One Target: Women with HER2+ Breast Cancer
Molecular Targets for Breast Cancer
Scientists have uncovered molecular and genetic approaches to identify specific genes, proteins, and molecular pathways that are important for cancer development, growth, and survival. Understanding these biological mechanisms and how they relate to cancer has been a key factor in the development and delivery of new biologic cancer therapies, especially for breast cancer, which is the most frequently diagnosed form of cancer in women worldwide. Knowing a tumor’s genetic profile allows clinicians to select the best treatment for a patient without exposing them to drugs that will not be effective against their cancer [See 2006 BenchMarks issue on TAILORx at http://benchmarks.cancer.gov/2006/05/cancer-diagnostics-informing-the-development-of-tailored-cancer-therapy/]. Targeting therapies to cellular pathways specific to cancer also results in less toxicity to healthy cells in the body. This may allow clinicians to treat patients for longer periods of time, if necessary, to prevent the cancer from recurring.
Many pathways are regulated through cell receptors — proteins on the surface or within a cell that usually bind with a specific molecule (a ligand), resulting in a signal that tells the cell to take action. These signals travel along pathways from the outer surface of the cell, carrying a message to the cell’s nucleus. Cell signaling is a critical activity that regulates cell activities and ensures that cells act in a coordinated, controlled manner. However, signals can be altered at many points along the pathways, causing cells to function abnormally. In cancer, many of the altered pathways are related to cell growth, proliferation, and survival.
Developing Targeted Drugs
Identifying signaling pathways that play a role in the development of cancer has allowed researchers to develop drugs that fight cancer by targeting these pathways in cancer cells. Estrogen is known to play an important role in the development of breast cancer and about 70 percent of all breast cancers are estrogen-receptor positive; blocking the flow of the hormone estrogen to the receptor can help starve the tumor. Tamoxifen, which has been used for more than 20 years to treat breast cancer, was developed to block the estrogen receptor.
The HER2 gene is another factor that can influence tumor growth and aggressiveness in breast cancer, so scientists have been investigating drugs that target the HER2 receptor for over a decade. Trastuzumab (Herceptin ®), first approved by the FDA in 1998, was the first molecular-based targeted treatment for metastatic breast cancer, and has since been approved for adjuvant treatment (used in addition to other types of therapy such as surgical excision or radiation) of early breast cancer. Trastuzumab is only effective in HER2+ breast cancer cells. Lapatinib (Tykerb ®) was approved in 2007 for treatment of advanced, metastatic breast cancer in combination with the chemotherapy drug capecitabine (Xeloda ®). It acts on a number of proteins including the HER2 receptor. Both trastuzumab and lapatinib disrupt cell signaling pathways, inhibiting tumor growth.
Mechanisms of Action against HER2
Normal breast cells contain two copies of the HER2 gene and produce appropriate amounts of HER2 receptors to enable normal cell growth and division. Some breast tumor cells, however, contain many more copies of the HER2 gene and in turn produce too many HER2 receptors — the receptors are overexpressed. Approximately 20 to 25 percent of breast cancers overexpress HER2. In addition to being more aggressive, tumors overexpressing HER2 are more likely to recur than tumors that do not express HER2.
The HER2 receptor is a member of the family of cell surface receptors known as HER/ErbB or human epidermal growth factors (EGFR). The four primary members of the HER family include HER1/EGFR, HER2, HER3, and HER4. These are receptor tyrosine kinases, which are receptors for molecules such as growth factors, cytokines, and hormones.
HER receptors have three components: an extracellular ligand-binding domain receptor that is located outside the cell, a transmembrane domain that crosses the cell membrane, and an intracellular tyrosine kinase domain that is inside the cell. When a ligand, such as a growth factor, binds to a HER receptor’s extracellular domain, it causes the following cascade of effects:
- Each HER receptor partners, or dimerizes, with a second receptor. HER receptors can combine with the same type of receptor, such as HER1 to HER1, forming a homodimer, or with another member of the HER family, such as HER1 to HER2, forming a heterodimer.
- Dimerization activates the intracellular receptor kinase, which adds a phosphate molecule to the tyrosine in the intracellular domain.
- This addition of the phosphate molecule activates signaling pathways important in cell proliferation and survival.
HER2, however, does not appear to have a ligand that promotes the formation of HER2 homodimers, but overexpression of HER2 can lead to HER2 homodimers, which may result in signaling without the presence of a ligand. In addition, HER2 is the preferred partner of other HER receptors so it may be a co-receptor for many different ligands. The type of partners in a heterodimer is important, because it affects signal strength. Heterodimers containing HER2 generate stronger signals and prolonged activation of signaling pathways compared to heterodimers without HER2. Overactivity of HER receptors plays a role in the growth of many cancers and in their resistance to cancer therapy.
Evolving knowledge about the HER2 receptor in the development of breast cancer and its pathways has been instrumental in the development of trastuzumab and lapatinib. Although these two drugs are aimed at the HER2 receptor, they work in different ways. Trastuzumab blocks the HER2 receptor’s actions from outside the cell, while lapatinib works on the inside of the cell. This difference may explain why lapatinib works in some women for whom trastuzumab is no longer effective.
How Trastuzumab and Lapatinib Work
Trastuzumab is a monoclonal antibody. Antibodies are proteins made by the body’s immune system that are directed against antigens, which are molecular components of foreign and infectious agents. Monoclonal antibodies are created in the laboratory from a single cell and are engineered to bind to a certain target. Trastuzumab is believed to fight cancer through several mechanisms of action. The primary mechanisms are thought to be trastuzumab’s effects on cell signaling pathways and on immune cells.
When trastuzumab binds with the HER2 receptor, it downregulates, or suppresses, the HER2 gene causing fewer HER2 receptors to be expressed. This decreases HER2 dimerization and the formation of heterodimers with other HER receptors, which interferes with cell signaling pathways. Disruption at any point in a signaling pathway can have an effect on each subsequent step. Two enzymes in particular are often affected. The mitogen-activated protein kinase (MAPK) and phosphatidylinositol 3-kinase (PI3K)-AKT pathways are thought to be the most affected by trastuzumab. These are complex signaling pathways in which a series of kinases activate subsequent kinases in response to the addition of phosphate molecules:
- MAPK is important for many cellular processes such as gene expression, division, and cell survival.
- The PI3-K/AKT signaling pathway has been linked to a diverse array of cellular functions — most notably cell proliferation and survival.
The activity of these pathways contributes to cellular events that lead to the development of cancer.
Trastuzumab is thought to kill tumor cells not only by its direct action on tumor cell signaling but also indirectly by attracting the body’s own immune cells to help destroy the cancer cells. When trastuzumab binds to tumor cells, it attracts and activates immune cells called natural killer cells. These immune cells attach to the bound trastuzumab molecule and release enzymes and factors that kill the tumor cell. Studies have indicated that when trastuzumab is present, immune cells preferentially target HER2 overexpressing cancer cells compared with cancer cells that do not overexpress HER2.
Trastuzumab has been an important option for many women with HER2+ breast cancer, but because cancer can mutate, it may eventually become resistant. Therefore, scientists have looked for other drugs that can widen that target by inhibiting HER receptors through different mechanisms.
Lapatinib is a dual tyrosine kinase inhibitor that targets two of the four HER family receptors — HER1 and HER2. Like trastuzumab, it disrupts signaling in the MAPK and PI3K-AKT pathways, but lapatinib stops HER signals from within a cell. Lapatinib competes with ATP for its binding site on the tyrosine kinase domain of the receptor. When lapatinib binds to the ATP-binding site, it blocks receptor phosphorylation and activation. This prevents subsequent signaling events along the MAPK and PI3K/Akt pathways.
Difference Between Lapatinib and Trastuzumab
Both lapatinib and trastuzumab have shown progress as breast cancer treatments, but small molecule dual kinase inhibitors have distinct mechanistic differences from large monoclonal antibodies. Small molecules can be taken as a pill so they may be more convenient for patients, especially working women who manage breast cancer as a chronic disease. Trastuzumab is a large protein and must be administered intravenously.
About one-third of women with HER2 breast cancer develop brain metastases. Treatment with trastuzumab does not seem to be as effective against advanced disease of this type. It may be too big to cross the blood-brain barrier. However, lapatinib may be small enough to cross the blood-brain barrier and enter brain tissues, which may make it effective in treating brain tumors and metastasis.
Monoclonal antibodies are very specific to the targets to which they bind. They bind to the outside of the cell by recognizing certain molecular structures at the binding site. If these structures are not present, they cannot bind. In some tumors, the HER 1 and HER2 receptors lack the portion of the molecule that sticks out above the cell’s membrane. Trastuzumab does not recognize these altered HER receptors, so it does not bind to them. After a time, some women quit responding to treatment with trastuzumab and the disease progresses. Trastuzumab resistance can be mediated, at least in part, through expression of such a modified HER2 receptor.
Tyrosine kinase inhibitors lack this specificity. These molecules exert their effect by entering the cell and interfering with signaling pathways. Dual tyrosine kinase inhibitors such as lapatinib can target cancer cells with more than one type of HER receptor, which gives more options for inhibiting the development of cancer and may be more useful in a wider range of patients. Additionally, inhibiting heterodimers containing both HER1 and HER2 may be more effective than targeting either HER1 or HER2 alone.
Since trastuzumab and lapatinib inhibit HER receptors by different methods, researchers are investigating the efficacy of treating patients with these drugs simultaneously. In preclinical trials, these drugs have been shown to have a synergistic effect against HER2+ breast cancer cells and lapatinib was effective against cells that were resistant to trastuzumab. In an early phase study, patients whose breast cancer had progressed while receiving trastuzumab responded, at least partially, to treatment with lapatinib.
ALTTO (Adjuvant Lapatinib and/or Trastuzumab Treatment Optimization trial), currently underway in North America and Europe, is studying the efficacy of lapatinib, trastuzumab, their sequence and combination in HER2+ early stage breast cancer. This international trial plans to enroll 8,000 women and is conducted jointly by the Breast International Group and the North Central Cancer Treatment Group, which is supported by the NCI. It is hoped that this trial will yield an answer as to how effective these drugs may be in different combinations by the end of the decade.
Animation/Video
|
|||||
Photos/Stills
Breast cancer cell, photographed by a scanning electron microscope, showing the overall shape of the cell's surface at a very high magnification. A scanning electron microscope can show how cells respond in changing environments and can show mapping distribution of binding sites of hormones and other biological molecules.

Breast cancer treatment facility in a low income country
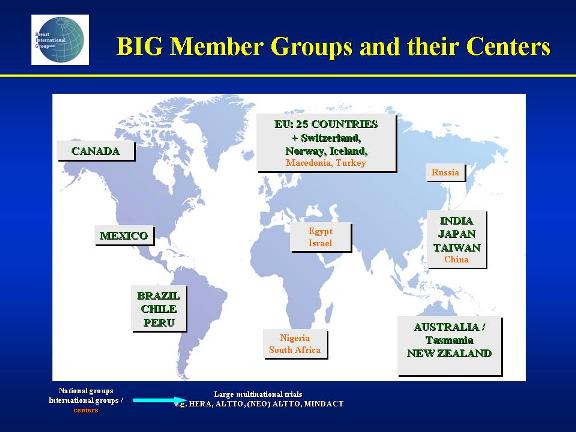
Breast International Group (BIG) member groups and their centers
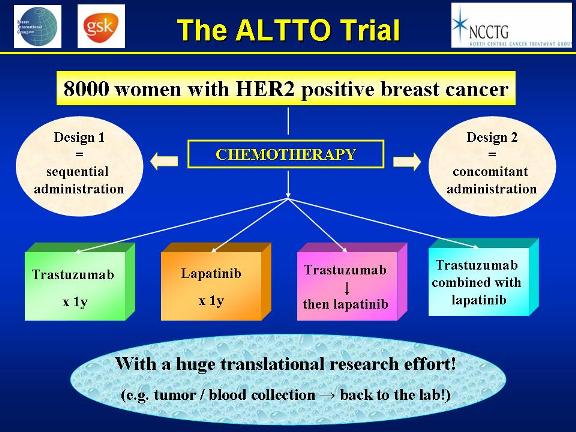
Randomization schema for patients on the ALTTO trial
 NCI NewsCenter
NCI NewsCenter NCI Budget Data
NCI Budget Data Visuals Online
Visuals Online NCI Fact Sheets
NCI Fact Sheets Understanding Cancer Series
Understanding Cancer Series