- Home
- Search for Research Summaries, Reviews, and Reports
EHC Component
- EPC Project
Full Report
- Research Review Jun. 1, 2012
Related Products for this Topic
- Research Protocol Dec. 6, 2010
- Clinician Summary Nov. 20, 2012
- La Guías Sumaria de los Consumidores Feb. 7, 2013
- Executive Summary Apr. 24, 2012
Related Links for this Topic
Consumer Summary – Nov. 20, 2012
Medicines for Rheumatoid Arthritis: A Review of the Research for Adults
Formats
- View PDF (PDF) 305 kB
- Download Audio (MP3) 11.4 MB
- En Español
- Help with Viewers, Players, and Plug-ins
Table of Contents
- Is This Information Right for Me?
- Understanding Your Condition
- Understanding Your Options
- Making a Decision
- Source
Is This Information Right for Me?
Yes, this summary is for you if:
- Your doctor* has told you that you have rheumatoid (pronounced ROOM-ah-toyd) arthritis (RA).
- Your doctor has suggested that you take one or more disease-modifying anti-rheumatic drugs (DMARDs, pronounced DEE-mardz) to treat your RA.
- Abatacept (Orencia®)
- Adalimumab (Humira®)
- Anakinra (Kineret®)
- Certolizumab pegol (Cimzia®)
- Etanercept (Enbrel®)
- Golimumab (Simponi®)
- Hydroxychloroquine (Plaquenil®)
- Infliximab (Remicade®)
- Leflunomide (Arava®)
- Methotrexate (Folex®, Rheumatrex®, Trexall®)
- Rituximab (Rituxan®)
- Sulfasalazine (Azulfidine EN-Tabs®, Sulfazine®)
- Tocilizumab (Actemra®)
- Your doctor has suggested you take a corticosteroid together with a DMARD to treat your RA.
- Methylprednisolone (Depo Medrol®, Medrol®, Solu-Medrol®)
- Prednisolone (Delta-Cortef ®, Econopred®, Orapred®, Pediapred®, Prelone®)
- Prednisone (Deltasone®, Liquidpred®, Sterapred®)
- You want to know what research says about the benefits and side effects of these medicines.
* In this summary, the term “doctor” refers to all the health care professionals who may take care of you, including your physician, rheumatologist, nurse practitioner, or physician assistant.
This summary is not for you if:
- You have a type of arthritis other than RA, such as osteoarthritis.
- Your doctor has not suggested that you take DMARDs or corticosteroids for your RA.
- You are under age 18. This information is from research on adults.
What will this summary tell me?
This summary will tell you about two types of medicine to treat RA: DMARDs and corticosteroids. It will explain what research has found about how well DMARDs work when taken alone or with corticosteroids to treat RA. It will also tell you what research says about the side effects of these medicines. You can use this summary to talk with your doctor about whether one of these medicines may be right for you.
Where does the information come from?
Researchers funded by the Agency for Healthcare Research and Quality (AHRQ), a Federal Government research agency, reviewed 211 studies on medicines for RA published between January 1990 and January 2011. The report was reviewed by clinicians, researchers, experts, and the public. You can read the report at www.effectivehealthcare.ahrq.gov/dmardsra.cfm.
Understanding Your Condition
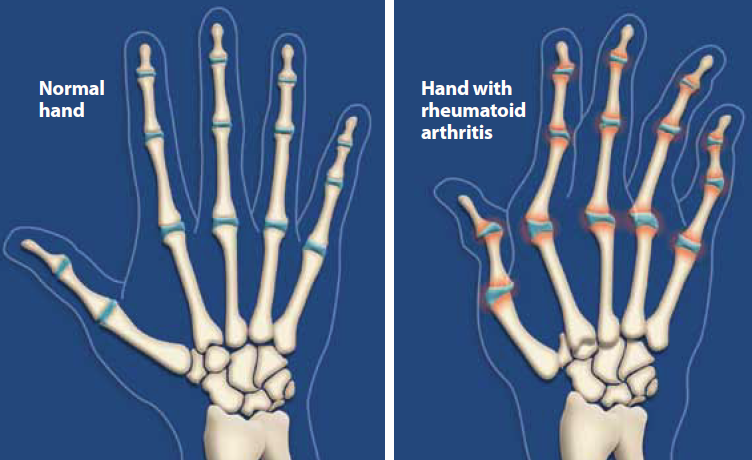
What is rheumatoid arthritis?
Rheumatoid arthritis (RA) is a disease that causes pain, swelling, and stiffness in the joints. In some people, it can also cause the joints to become damaged and deformed.
- Although it can affect any joint in the body, RA is most commonly found in the hands, wrists, feet, and knees. Usually, if it is found in one hand, it will appear in the other as well.
- Sometimes RA can cause problems with body parts other than your joints such as your heart, lungs, eyes, or mouth.
- RA usually lasts many years or an entire lifetime. For some people, RA can last for only a few months to a few years with treatment, although this is rare.
- The symptoms of RA (pain, swelling, stiffness) can get worse for some periods of time (called a “flareup”) and then get better for some periods of time.
What causes RA?
The cause of RA is unknown, but researchers think the condition may be passed down in families. The pain and symptoms of RA happen when your immune system (the system of the body that helps defend you from germs) attacks the healthy lining of your joints. Doctors are not sure why the immune system in some people attacks their joints.
How common is RA?
- RA is less common than other kinds of arthritis such as osteoarthritis.
- More than 1 million people in the United States have RA.
- Women are more likely to have RA than men. About 7 out of every 10 people with RA are women.
- Although RA can happen at any age, it usually develops between ages 30 and 50.
How can treatment help?
Although there is no cure for RA, treatment can:
- Relieve pain and swelling
- Slow down or stop joint damage
- Help lower the number of symptom “flareups” (times when pain or swelling is the worst)
- Improve your ability to do daily activities such as bathing, getting dressed, doing chores, reaching, and lifting
What medicines are used to treat RA?
RA is treated with several different types of medicines, including:
- Pain relievers: Over-the-counter medicines such as aspirin, acetaminophen (Tylenol®), ibuprofen (Advil®, Motrin®), or naproxen (Aleve®)
- Corticosteroids: Medicines that can relieve RA pain and swelling for a little while
- Disease-modifying anti-rheumatic drugs (DMARDs): Medicines that can decrease symptoms, slow or stop joint damage, and improve your ability to do daily activities
Sometimes DMARDs and corticosteroids are taken together to treat RA. This summary looks at the research on how well DMARDs work when taken alone or with corticosteroids.
Understanding Your Options
What are DMARDs?
DMARDs are a family of medicines that stop the body’s immune system from attacking and destroying joints. If you have severe RA symptoms or are not getting enough relief from pain relievers or corticosteroids, your doctor may suggest a DMARD. DMARDs may be taken with each other or together with pain relievers and corticosteroids.
There are two kinds of DMARDs: nonbiologic and biologic.
Nonbiologic DMARDs
Like most medicines, nonbiologic DMARDs are produced from chemicals. They are usually taken daily or weekly as pills, but some can also be given as shots. Nonbiologic DMARDs include:
- Hydroxychloroquine (Plaquenil®)
- Leflunomide (Arava®)
- Methotrexate (Folex®, Rheumatrex®, Trexall®)
- Sulfasalazine (Azulfidine EN-Tabs®, Sulfazine®)
Biologic DMARDs
Biologic DMARDs are proteins similar to those made in your body, but these proteins are created in laboratories. Biologic DMARDs must be given as shots or through an IV (intravenous) tube into a vein in your arm. Biologic DMARDs include:
- Abatacept (Orencia®)
- Adalimumab (Humira®)
- Anakinra (Kineret®)
- Certolizumab pegol (Cimzia®)
- Etanercept (Enbrel®)
- Golimumab (Simponi®)
- Infliximab (Remicade®)
- Rituximab (Rituxan®)
- Tocilizumab (Actemra®)
Some biologic DMARDs such as infliximab (Remicade®), rituximab (Rituxan®), and tocilizumab (Actemra®) need to be given through an IV tube at a doctor’s office or clinic. This could take up to 2 hours. Other biologic DMARDs come in injection pens that you can use at home.
Most biologic DMARDs are given once a month, once every other week, or once a week. Your doctor may change your schedule depending on how well you are doing.
What are the possible side effects of nonbiologic and biologic DMARDs?
Because nonbiologic and biologic DMARDs work in different ways, they have different side effects, some of which are serious.
| Nonbiologic DMARDs | Biologic DMARDs |
|---|---|
| This information comes from the U.S. Food and Drug Administration (FDA) labels of these medicines. | |
|
|
| Possible Serious Side Effects | |
|
|
What are corticosteroids?
Corticosteroids are a kind of medicine that works like a certain type of hormone in your body. Corticosteroids can help reduce swelling and stop the body’s immune system from attacking healthy joints. Corticosteroids are taken as pills, liquids, or shots and include:
- Methylprednisolone (Depo Medrol®, Medrol®, Solu-Medrol®)
- Prednisolone (Delta-Cortef ®, Econopred®, Orapred®, Pediapred®, Prelone®)
- Prednisone (Liquidpred®, Deltasone®, Sterapred®)
What are the possible side effects of corticosteroids?
Possible side effects of corticosteroids listed by the U.S. Food and Drug Administration (FDA) include:
- Swelling in the lower legs
- Weight gain
- Increased blood pressure
- Mood swings
- Increased pressure in the eyes
Possible side effects from taking corticosteroids for longer than a few days or weeks include:
- High blood sugar, which can cause or worsen diabetes
- Increased risk of infections
- Loss of calcium from bones, which can make it easier to break a bone
- Irregular menstrual periods
- Thin skin that bruises easily
- Longer time for wounds to heal
What does research say about nonbiologic DMARDs?
How well they work to treat RA:
- Methotrexate (Folex®, Rheumatrex®, Trexall®) and sulfasalazine (Azulfidine EN-Tabs®, Sulfazine®) work about the same to reduce symptoms, reduce the number of joints affected, improve the ability to do daily activities, and slow down or stop joint damage.
- Leflunomide (Arava®) appears to work about as well as methotrexate, but there is not enough research to know this for certain.
Side effects:
- All nonbiologic DMARDs appear to cause about the same amount of side effects, but there is not enough research to know this for certain.
What does research say about biologic DMARDs?
How well they work to treat RA:
- Biologic DMARDS work to decrease or completely stop symptoms, improve the ability to do daily activities, and slow down or stop joint damage.
Side effects:
- Taking a biologic DMARD increases the risk of developing serious infections.
- Taking biologic DMARDs for long periods of time does not increase the risk of having serious side effects.
What does research say about combining medicines?
How well they work to treat RA:
- If treatment with one DMARD does not relieve symptoms, taking a biologic DMARD together with the nonbiologic DMARD methotrexate works better than taking only one to improve the ability to do daily activities and slow down or stop joint damage.
- Adding a corticosteroid to treatment with a nonbiologic DMARD improves the ability to do daily activities more than taking a nonbiologic DMARD alone. Adding a corticosteroid may also slow down or stop joint damage more than taking a nonbiologic DMARD alone, but there is not enough research to know this for certain.
- For people who have had RA for less than 3 years, taking two or three nonbiologic DMARDs plus a corticosteroid works better than taking only one nonbiologic DMARD.
- For people who have had RA for less than 3 years, taking the nonbiologic DMARD methotrexate together with a biologic DMARD decreases or completely stops symptoms and slows down or stops joint damage in people whose RA was quickly getting worse.
- For people who have had RA for a long time without any improvement, taking three nonbiologic DMARDs together reduces symptoms and the number of joints affected more than taking one or two nonbiologic DMARDs.
Side effects:
- Taking a nonbiologic DMARD with a biologic DMARD does not cause more side effects than taking the biologic DMARD alone.
- Taking two or more biologic DMARDs together can cause more serious side effects than taking only one.
- Taking a corticosteroid together with a nonbiologic DMARD does not make treatment more difficult to tolerate.
- In people who have had RA for less than 3 years, taking two or three nonbiologic DMARDs plus a corticosteroid does not make treatment more difficult to tolerate than taking only a nonbiologic DMARD.
What does research say about how nonbiologic and biologic DMARDs compare to each other?
How well they work to treat RA:
- The biologic DMARDs adalimumab (Humira®) and etanercept (Enbrel®) help decrease symptoms about the same as the nonbiologic DMARD methotrexate.
Side effects:
- There is not enough research to know if certain side effects happen more often with nonbiologic or biologic DMARDs.
Making a Decision
What should I think about when deciding?
More research is needed to know which RA medicines might work best for different people. There are several things to consider when choosing a medicine to treat your RA:
- The trade-offs between the possible benefits and side effects for each medicine
- Which medicine best fits your lifestyle, what is important to you (your values), and your preferences
- You may want to think about how comfortable you are with taking pills, getting shots, or taking the medicine through an IV tube. You may also want to consider how often you are able to go to the doctor’s office or clinic and how much time you are able to spend there.
- The cost of each medicine
What are the trade-offs?
Only you and your doctor can decide whether taking a DMARD for your RA is worth the risk of possible side effects. You and your doctor should discuss:
- The amount of pain or joint damage you have and whether treatment with a DMARD can help
- The risk of serious side effects from DMARDs
- Signs to look for to help you notice serious side effects so they can be treated or so your medicine can be changed
- Whether adding a corticosteroid to your treatment with DMARDs might help
- Other options besides DMARDs that might help your RA
What are the costs?
The costs to you for nonbiologic and biologic DMARDs and corticosteroids depend on:
- Your health insurance plan
- The amount (dose) you need
- Whether you take the medicine as a pill, as a shot, or through an IV tube
- Whether a generic form of the medicine is available
- Whether the company that makes the medicine offers financial help to lower the cost
Corticosteroids can be taken for short periods of time (30 days) or longer, depending on your specific needs. The cost for corticosteroids is around $3 to $15 a month. The cost to you depends on how much of the medicine you need and how long you will need to take it.
| Drug Name | Brand Name | Price per Month* | Form | Dose |
|---|---|---|---|---|
| * Prices are the average wholesale prices from RED BOOK Online® rounded to the nearest $5. Generic prices are the middle value in the range of prices listed from different manufacturers. The actual prices of the medicines may be higher or lower than the prices listed here, depending on your health insurance and the manufacturer used by your pharmacy. IV = intraveneous |
||||
| Nonbiologic DMARDs | ||||
| Hydroxychloroquine | Generic | $35–$75 | Tablet | 200–400 mg daily |
| Plaquenil® | $110–$215 | |||
| Leflunomide | Generic | $490 | Tablet | 20 mg daily |
| Arava® | $910 | |||
| Methotrexate | Generic | $45–$90 | Tablet | 7.5–15 mg weekly |
| Folex®, Rheumatrex®, Trexall® | $125–$140 | |||
| Sulfasalazine | Generic | $40 | Tablet | 2,000 mg daily |
| Azulfidine EN-Tabs® | $120 | |||
| Sulfazine® | $30 | |||
| Biologic DMARDs (Generic versions of these medicines are not available.) | ||||
| Abatacept | Orencia® | $1,430–$2,860 | IV | 500–1,000 mg monthly |
| $2,530 | Shot | 125 mg weekly | ||
| Adalimumab | Humira® | $2,450 | Shot | 40 mg twice a month |
| Anakinra | Kineret® | $2,760 | Shot | 100 mg daily |
| Certolizumab pegol | Cimzia® | $2,360 | Shot | 400 mg monthly |
| Etanercept | Enbrel® | $2,475 | Shot | 50 mg weekly |
| Golimumab | Simponi® | $2,650 | Shot | 50 mg monthly |
| Infliximab | Remicade® | $3,725–$9,300 | IV | 200–500 mg twice a month (depending on your weight) |
| Rituximab | Rituxan® | $15,180 | IV | 1,000 mg twice a month |
| Tocilizumab | Actemra® | $1,660–$3,320 | IV | 400–800 mg monthly (depending on your weight) |
Ask your doctor
- Do you think a DMARD could help my RA?
- What serious side effects should I look for?
- Would adding a corticosteroid to a DMARD help my RA?
- How long will it take until I start to feel better?
- Is there a less expensive medicine that I could take?
- What else can I do to help my RA?
- Are there specific lifestyle changes you can suggest that might help?
Source
The information in this summary comes from the report Drug Therapy for Rheumatoid Arthritis in Adults: An Update, April 2012.
The report was produced by the RTI International–University of North Carolina Evidence-based Practice Center through funding by the Agency for Healthcare Research and Quality (AHRQ). For a copy of the report or for more information about AHRQ and the Effective Health Care Program, go to www.effectivehealthcare.ahrq.gov/dmardsra.cfm. Additional information came from the MedlinePlus® Web site, a service of the National Library of Medicine and the National Institutes of Health. This service is available at www.nlm.nih.gov/medlineplus.
This summary was prepared by the John M. Eisenberg Center for Clinical Decisions and Communications Science at Baylor College of Medicine, Houston, TX. It was written by Amelia Williamson Smith, M.S., Thomas Workman, Ph.D., John Gomez, M.D., and Michael Fordis, M.D. People with rheumatoid arthritis reviewed this summary.
Return to Top of Page
 E-mail Updates
E-mail Updates