Introduction
Purpose of This Toolkit
Improving the care for the chronically ill is one of the most pressing health needs of our time.
The Institute of Medicine's report, Crossing the Quality Chasm, made clear that there were no
easy roads to improvement. Healthcare organizations must redesign their systems of care to
better address the needs of their patients with depression, asthma, diabetes, and other chronic
conditions. America's safety net providers have led the way. Today, 10 years after the
development of the Chronic Care Model and the initial implementation of the Health Disparities
Collaboratives, the lessons learned, tools developed, and strategies used by these vanguard
teams provide the foundation for the next wave of improvement in chronic illness care.
To help more safety net organizations implement the Chronic Care Model (CCM) effectively
and sustainably, the Agency for Healthcare Research and Quality (AHRQ) asked Group Health's
MacColl Institute in Seattle, RAND, and the California Health Care Safety Net Institute
(SNI) to develop and test a toolkit and a practice coaching approach. The toolkit provides a
step-by-step practical approach to guide teams through quality improvement. A companion
Practice Coaching Manual that outlines our approach and provides orientation to other
national efforts is also available.
This Toolkit:
- Sequences and describes the specific practice changes involved in Chronic
Care Model implementation.
- Integrates business strategies to address the financial and operational
barriers to quality improvement.
- Links more than 60 tools commonly used for quality improvement with the
relevant changes.
- Includes example stories from practices that have made quality improvement pay.
Return to Contents
Need To Improve Chronic Illness Care
Chronic diseases such as heart disease, stroke, cancer and diabetes are among the most
prevalent, costly, and preventable health problems facing1
For the more than 100 million
people in the United States living with at least one chronic disease, quality of life can be low
and medical expenses, high. In fact, the treatment for individuals with chronic illness
accounts for more than three quarters of national healthcare expenditures.2
According to the
Institute of Medicine's Crossing the Quality Chasm report, about 50 percent of these
Americans are not receiving good chronic illness care.3 For those living without health
insurance, the situation is even more drastic. Most people now agree that the poor quality of
care in this country is a result of healthcare that is misaligned, unplanned, and fragmented.
Return to Contents
The Chronic Care Model as a Guide for Change
With funding from the Robert Wood Johnson Foundation, the MacColl Institute developed
and tested a quality improvement approach based both on evidence and experience of how
to effectively care for chronically ill people. This work led to the development of the Chronic
Care Model, a visual guide to the comprehensive, integrated reorganization of care delivery
needed to improve important patient outcomes.4,5 The diagram below illustrates the Chronic Care Model:
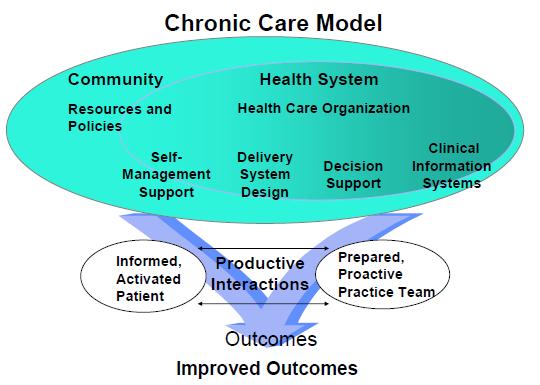
Redesigning health systems to align with the Chronic Care Model emphasizes the central role
of patients and their relationship with an organized practice team to achieve optimal health
outcomes. It changes the healthcare system's focus from reacting to the acute care needs of
individuals to taking a proactive approach to engaging a population of patients. The Chronic
Care Model puts the patient's long-term health goals, needs, and competencies at the center
of the healthcare system. It challenges the notion of specialized knowledge resting solely with
the physician in favor of a broader approach where every member of the care team, including
the patient, brings expertise to the table.
The Chronic Care Model includes six essential elements of a health care system that when
integrated encourage high-quality chronic disease care:
- Community resources.
- Health system.
- Self-management support.
- Delivery system design.
- Decision support.
- Clinical information systems.
To achieve real improvements in the quality of care as indicated by process and outcome
measures, attention should be paid to each of these six elements. For more detailed
information about the evidence base for the Chronic Care Model and a discussion of how the
need for this toolkit and coaching methodology arose, please go to Appendix A.
Return to Contents
Making Changes in Practice
Implementing changes across all six elements of the Chronic Care Model can sound
intimidating. In years of working with practices across the country, we have often been asked:
Where do I start? This toolkit is designed, in part, to answer this question. Although all six
elements of Chronic Care Model will be taught, experience suggests that practice changes can
and should be made sequentially.
The Toolkit Describes Four Main Phases:
Phase 1 to Phase 4 include all of the Chronic Care Model Elements.
Phase 1: Getting Started
Phase 2: Assess Data & Set Priorities for Improvement
Phase 3: Redesign Care and Business Systems
Phase 4: Continuously improve performance and work to make changes sustainable
The goal of the Chronic Care Model is to improve health outcomes by optimizing the
individual practice team's interaction with patients, but it is clear that changes need to be
made at all levels of the organization to support this work. The tools in this kit are generally
focused on changes at the physician practice level. However, changes in both clinical and
business practices, like those discussed below, require involvement and support from leaders
and staff in financial and managerial departments. Depending on the structure of your
organization, effective practice redesign efforts need to ensure that the decision-makers at
all levels of the organization are involved.
Return to Contents
The Business Case for Quality Improvement
One of the first questions that financial and administrative leaders ask is: what is the business
case for this new initiative? In addition to serving the business of healthcare by improving
the very core of our work—improving patients' health, implementing the Chronic Care Model
has the potential to:
- Improve staff satisfaction and retention.
- Enhance patient satisfaction and loyalty.
- Position clinics to capture pay-for-performance and quality
improvement bonuses and grants.
- Streamline workflow and maximize the use of staff.
- Improve efficiency.
The first step to making the business case for any new quality initiative in health care is to
understand your organization's unique financing structure. Examine your payer mix and learn
what types of practice activities generate revenue. For example, if you are reimbursed
primarily on a fee-for-service basis, you may generate more revenue by ensuring that all of
your diabetic patients have the recommended number of Hemoglobin A1c tests. If you are
paid primarily on a capitated basis, then ensuring that your patients are taught how best to
manage their illness and avoid specialist or emergency room visits will likely provide a more
robust financial return.
This toolkit provides strategies and tools to improve your financial performance while
improving your clinical performance. Because the business of healthcare is to deliver the
highest quality care to patients, improving clinical performance is the driving focus of our
toolkit. However, understanding and responding to the reality of financial pressures through
increased efficiency and enhanced revenue capture is what makes clinical changes possible
and sustainable.
Because the financial landscape differs among organizations and even practices within
organizations, we emphasize financial tools that are broadly applicable. We have also
integrated text advice tailored to three financial tracks marked as Track 1, 2, or 3. Which
track of tools you use will be based on where your organization falls in the flowchart below.
Financial Track Identification Tool

Track 1 is designed for practices that are reimbursed primarily on a capitated
basis. In general, track 1 focuses on tools that increase efficiency, primarily by optimizing the
care team and using process mapping to reduce waste. Certainly practices that are at risk for
emergency department admissions, hospitalizations, or pharmaceutical utilization will want
to focus on areas that help to contain these costs.
Track 2 is designed for practices that are reimbursed primarily on a fee-for-service
basis and that are not generally reimbursed services provided by ancillary,
nonphysician, providers. In these practices, a physician must be involved in the delivery of
care to receive reimbursement. Services provided by other professionals such as Licensed
Clinical Social Workers or Certified Diabetes Educators are not reimbursable. In addition to
efficiency tools applicable to the capitated group, Track 2 practices will use tools focused on
increasing revenue by examining billing practices. Each visit in the track 2 practices should be
designed to include physician time.
Track 3 practices are those that are reimbursed based primarily on a fee-forservice
structure and for which providers can receive payment for ancillary services. These
practices will be directed toward the efficiency tools in tracks 1 and 2, and the revenue
enhancement tools in track 2. In addition, track 3 practices will focus on further optimizing the care team by making use of non-physician specialists for patient education and self-management
support functions with billable.
Admittedly, primary care practices are faced with many different payers and many different
and sometimes conflicting financial incentives. The goal of this toolkit is not to be overly
prescriptive. Rather, we encourage you to examine the financial structure of your practice
and to take advantage of those financial elements that support and might be rewarded by
your quality improvement efforts.
Finally, revenues are only one side of the equation. Reducing costs benefits all practices,
regardless of payer source, and therefore applies to all user tracks. Additional cost-cutting
tools are included under "Advanced Topics."
This toolkit provides you with specific clinical and business key changes that you can put to
use in your practice. The clinical changes are paramount, and the business change processes
are important to the extent that they facilitate clinical improvements. Therefore, we have
purposely omitted many potentially worthwhile business tools that are not explicitly linked to
improving clinical care. Many of those concepts, such as improving your collections policy, are
valuable strategies that teams might want to undertake after implementing the Chronic Care
Model. While we certainly encourage efficiency in the business as well as clinical realm, our
focus here is guided by the clinical changes.
Return to Contents
How To Use This Toolkit
This toolkit is meant to be explicit enough to be used as a standalone document, but our
experience suggests that real change is rarely achieved unless information and tools are
linked to an organized quality improvement effort. You can read about quality improvement
techniques on the Web at sites such as IHI.org if you want to be self-directed. Alternatively,
you can use expertise, such as a practice coach or facilitator to aid in implementing the
toolkit. A companion Practice Coaching Manual was developed and tested in conjunction
with this toolkit. The Practice Coaching Manual also provides orientation to other national
efforts using practice coaching and aids organizations in recruiting a coach to guide clinical
quality improvement.
With or without the use of a facilitator, orientating yourself to the structure and layout of
the toolkit before getting started will be helpful. As mentioned above, the toolkit is broadly
organized into four phases.
Within each phase there are several "key changes" to put into practice. The key changes are
not necessarily meant to be tackled chronologically. In fact, many practices may have already
addressed the content and tools presented in a given key change. If so, teams should skip that
key change and move to the next one. Practices should ensure that they have a handle on the
content of each key change, even if they do not need to do any work in that section. Key
changes are denoted by two numbers, such as: Key Change 1.2. The first number indicates
the phase, the second, the key change. In this example, you are looking at the second key
change within the first phase.
Each key change section is organized the same way, so you know what to expect as you move
through the toolkit. The first page starts with a header that includes the phase locator icon
and the number and title of the key change. Following the header, introductory content about
the key change is presented.
Financial track icons are woven throughout the introductory content. These icons are a tool to
help you navigate the toolkit, locating specific business advice for each track. Once you've
identified which financial track you're on, keep your eye out for that icon.
Following the introductory content and specific financial track information (if applicable),
there is a table with specific action steps and associated tools.
Each tool has been reviewed or created by staff at the MacColl Institute and represents what
we think is one of the best examples of a given type of tool available in the public domain.
This is not meant to be an all inclusive list.
Appendix B includes access to all tools. Tool cover sheets list relevant
Key Change(s), tool name, URL linking to online location, and suggested citation.
After the action and tool table, additional resources are listed. Unlike the tools, physical
copies of these resources are not included in the toolkit unless indicated by hyperlink text.
In most cases, these resources are not available for free or require specific technology (such
as a DVD player), but we thought they were worthwhile to include for those interested in
learning more. Not all key change sections will have additional resources.
In developing the toolkit we recognize that each practice will be at a different point in
their quality improvement work, and will approach this effort with different strengths and
challenges. Feel free to pick the tools, and the improvement method that will be of the
most help to you.
Return to Contents
Proceed to Next Section


