
July, 2009
Insight
What Started in Space Pays Off for Patients
New Cataract Early Detection Tool
By Allyson T. Collins, M.S.
NEI Science Writer/Editor

View an interview with NEI researcher Manuel Datiles, M.D.
The researchers are a seemingly unlikely match: an ophthalmologist from the National Eye Institute (NEI) and a physicist from the National Aeronautics and Space Administration (NASA).
They work hundreds of miles apart, one on the National Institutes of Health campus in Bethesda, Md., and the other at the NASA Glenn Research Center in Cleveland. But the distance between their research sites is even greater--one studies patients in eye care clinics on Earth, and the other analyzes technology in satellites orbiting Earth.
Nevertheless, a blinding eye condition, a fiber-optic probe, and a collaborative research agreement brought together NEI researcher Manuel Datiles, M.D., and NASA scientist Rafat Ansari, Ph.D., in 1994. Their partnership recently resulted in the creation of a new cataract early-detection tool that goes where no space probe has gone before.
Taking the first steps

A cataract clouds the center of this patient's lens.
In the 1980s, NASA's Ansari became intrigued by a physical technique known as dynamic light scattering (DLS), which means that moving particles in a solution scatter light at different intensities. When measured, these intensities can be used to determine the size of the dissolved particles.
Ansari's DLS experiments were conducted in preparation for the zero-gravity space environment, where particles such as proteins can grow bigger and better than on Earth without gravity holding them back.
While his initial studies were designed for space, "the human body has more than 100,000 different proteins, and when you try to treat any disease, you have to study protein structure," Ansari notes.
Still, Ansari's experiments stayed in orbit until he learned that his father had become one of the 20 million Americans diagnosed with a cataract. This clouding of the eye's lens accounts for nearly half of blindness around the world.
The news sent Ansari to medical libraries, where his literature search revealed that cataracts are caused by lens proteins that cluster abnormally, a process similar to what he was studying in space. With this knowledge, he turned to a rather unconventional laboratory for his next experiments--his kitchen.
"My daughter was in high school at the time, and she was dissecting cow eyes," Ansari explains. He brought a few home and asked her to remove the lenses. Then at his kitchen table, he conducted tests with a hand-held DLS probe to see whether the made-for-space technology could detect protein changes in the lenses.
Seeing the invisible
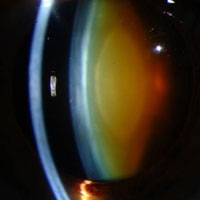
Side view: an amber-colored cataract blocks the center of the lens.
Datiles had been studying cataracts since the late 1970s during his ophthalmology training. When he joined the NEI, he participated in research involving non-surgical cataract treatments and new lens imaging methods.
While Datiles and other scientists searched for a tool that was accurate enough to detect lens protein changes in the clinic, other biochemical studies showed that alpha-crystallin, a major protein in the lens, serves as a molecular chaperone. This means that it binds to damaged lens proteins to prevent them from bunching together to form a cataract.
However, the amount of bound alpha-crystallin increases as a person ages, leaving less unbound alpha-crystallin available to prevent the protein bunching process. The bound alpha-crystallin also tends to scatter light more and participate in cataract formation.
"By the time the lens appears cloudy from a cataract, it is too late to reverse or medically treat this process," Datiles explains. "The time to start treating is actually before you run out of unbound alpha-crystallin, so a cataract will never appear in the first place."
During this search for a method to measure lens proteins, Ansari contacted NEI researchers about his DLS probe. Datiles was initially skeptical, so he and Ansari began experiments to find out if it worked.
In a head-to-head competition between Ansari's device and another imaging tool, the DLS probe won the battle to detect changes in lens proteins, including alpha-crystallin. "So I said, 'Okay, I'm convinced. Let's build a clinical device,'" Datiles says.
Moving to the clinic
First, scientists used animal lenses to verify that the DLS probe could detect alpha-crystallin's particular light scattering ability, so they could gauge the amount remaining in the lens. Then, they incorporated Ansari's miniaturized DLS probe into a clinical eye instrument with a three-dimensional aiming ability. With this tool, low-power laser light from the probe can be focused safely, accurately and repeatedly on specific locations in the lens.
The resulting device works like this: First, a patient rests his chin on the instrument. Next, a medical technician aims the probe at the center of the lens. Then, a light sensor measures the amount of laser light scattered by the lens over a five-second period. Finally, a statistician uses this information to determine the amount of unbound alpha-crystallin remaining in the lens.

In the NEI clinic, Dr. Datiles uses the DLS device to measure alpha-crystallin in a patient's lens.
In a recent study, Datiles and Ansari used the device on 380 eyes of patients in the clinic to determine the relationship between alpha-crystallin and lens cloudiness. As expected, they found that as the amount of unbound alpha-crystallin decreased--meaning that the lenses had less protection from cataracts--the cloudiness of the lenses increased.
The unbound alpha-crystallin amount also decreased as the patients' ages increased, even when the lenses were still clear. This may indicate that a cataract could form in the near future. These age-related, pre-cataract changes are not detected by currently available imaging tools.
Finding new applications
Before this device was created, clinicians had no way of confirming that outside influences affected cataract formation, though they believed that the environment, medications and certain surgeries played a role.
"It's like going on vacation and getting sick when you return home," Datiles explains. "It is hard to prove that you caught something on the trip, even though you believe it to be the case."
With this device, researchers may be able to pinpoint factors that cause cataract formation. They could also use it as an early alarm system to warn patients about lens damage. By detecting subtle protein changes before cataracts develop, doctors could advise patients to make simple lifestyle changes such as quitting smoking, decreasing sun exposure, stopping certain medications, and controlling diabetes to reduce their risk of developing cataracts.
Though the device is not yet available to the general public, Ansari is adapting it for the space program, so it can monitor the effects of cosmic radiation on the lens from within an astronaut's helmet. At the same time, Datiles and other vision researchers will use the current device in clinical trials to look at long-term lens changes related to aging and certain eye surgeries.
Datiles predicts that the technology could also prove valuable in medical specialties other than ophthalmology. Many doctors are concerned with the effects of oxidative stress, a process that damages cells and has been linked to aging, cancer and other diseases.
"Unlike most other organs, the eye is readily accessible to testing," Datiles says. "If researchers could use this test to measure oxidative stress in the eye, then it could help reflect the status of the other, inaccessible organs, such as the kidneys and the heart."
Ansari agrees that the eye could serve as an entry point for studying other organs. "By understanding the role of protein changes in cataract formation, we can use the lens not just to look at eye disease, but also as a window into the whole body."
Reference:
Datiles MB III, Ansari RR, Suh KI, Vitale S, Reed GF, Zigler JS, Ferris FL III (2008). Clinical Detection of Precataractous Lens Protein Changes Using Dynamic Light Scattering. Arch Ophthalmol, 126, 1687-1693.

