NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Agency for Health Care Policy and Research (US). AHCPR Consumer Guides. Rockville (MD): Agency for Health Care Policy and Research (US); 1992-1996.
This publication is provided for historical reference only and the information may be out of date.
Your Heart
The human heart is a remarkable organ that continuously pumps blood to nourish and provide energy to the body. As big as a fist, this powerful muscle uses its own electrical system to pump blood. It pumps 5 to 6 quarts of blood a minute during rest, but more than 20 quarts a minute during exercise.
Normally, the heart automatically adjusts to changing demands. As the body needs more nourishment and energy (for example, when climbing stairs), the heart responds. It should beat faster and more forcefully, causing more blood to circulate through the body. The blood will carry more oxygen and nourishment to muscles and organs and then return to the heart to begin the process again.
If you have heart failure, your heart is weak and its pumping power is reduced. Although it still beats normally, your heart cannot pump as much blood with each beat. Your symptoms will depend on how severe your heart failure is.
Purpose of This Booklet
If you have heart failure due to reduced pumping power of your heart (left-ventricular systolic dysfunction), this booklet is for you. Understanding your condition and following a few simple guidelines can improve the quality of your life.
This booklet is designed to help you and your family be active partners with your health care team-doctors, nurses, and other professionals. It is your guide to living with heart failure. Share it with your family and other caregivers.
This booklet will tell you how and why heart failure affects your body. It also tells how to respond to symptoms and what to expect from treatment. You need to know as much as you can to improve the quality of your life. Be involved in managing your condition.
What Is Heart Failure?
"Heart failure" simply means that your heart's pumping power is weaker than normal. Although it still beats, a weakened heart pumps too little blood rich with oxygen and nutrients to meet the body's needs. Walking, carrying groceries, or climbing stairs can be difficult. You may feel short of breath; the body is not getting all the oxygen it needs.
For most patients, heart failure is a chronic condition, which means it can be treated and managed, but not cured. If it is a complication of other medical conditions such as blocked coronary arteries or heart valve disease, surgery may help.
Causes of Heart Failure
The most common causes are:
Coronary artery disease, usually with previous heart attack (myocardial infarction [MI]).
Heart muscle disorder (cardiomyopathy).
High blood pressure (hypertension).
Heart valve disease.
Sometimes the exact cause of heart failure is not found. However, the actual cause is not as important as your heart's reduced pumping power and what can be done about it.
Symptoms
Check (X) your symptoms:
[ ]Difficulty breathing, especially with exertion or when lying flat in bed.
[ ]Waking up breathless at night.
[ ]Frequent dry, hacking cough, especially when lying down.
[ ]Fatigue, weakness.
[ ]Dizziness or fainting.
[ ]Swollen feet, ankles, and legs (edema).
[ ]Nausea, with abdominal swelling, pain, and tenderness.
Other medical problems can cause the same symptoms. A thorough physical exam and a complete health history, plus certain tests, are needed to diagnose heart failure and find its possible causes.
Causes of Symptoms
A healthy heart can increase how much oxygen-rich blood is pumped to vital organs and muscles as it is needed.
When a heart pumps with less power and force than normal, it cannot pump enough blood to organs and muscles. As a result, your body cannot do as much. Blood and fluids may collect or "pool" in the lungs. This can cause breathing problems when you lie down. Fluids can also collect in other parts of the body, swelling the feet, ankles, legs, and abdomen.
Your Health Care Team
Because heart failure is complex, a team of health care professionals is needed for special skills and expertise.
By working with your health care team in learning how to treat your condition, you may live longer and also improve the quality of your life.
Health care providers on the team may include:
Your primary care doctor-the doctor you normally see for health problems. General internists or family physicians normally provide primary care.
A cardiologist, if your primary care doctor believes a heart specialist is needed.
Other doctors, such as surgeons and other specialists, if needed and recommended by your primary care doctor or cardiologist.
Clinical nurse specialists and nurse practitioners, who care for you and are sources of information, education, and counsel.
Other health care professionals, including physician's assistants, nurses, dietitians, physical and occupational therapists, pharmacists, case managers, social workers, and other mental health professionals.
You and your family are important parts of this health care team. Before seeing other members of the health care team, write down your questions. Mark anything in this booklet you don't understand or would like to know more about. Using the list and this booklet, ask your health care provider questions. Tell him or her how you feel about your care.
Be involved in management of your condition.
How Your Heart's Chambers and Valves Work
Understanding how your heart works will help you understand the reasons behind the treatment plan your health care team designs for you. The more you know, the more you can be involved.
Blood moves through four chambers (two atriums and two ventricles) in the heart before circulating through the body (see Figure 1). With each heartbeat, blood returns from the body through the veins, enters one of the chambers-the right atrium-and moves through the valve into the right ventricle below it. At the same time, blood from the lungs that is rich in oxygen enters the left atrium on the other side of the heart. From the left atrium, the blood passes through a valve into the left ventricle.
Figure
Figure 1. Blood Flow to Heart Chambers.
Next, the right ventricle contracts after getting blood from the right atrium, sending blood to the lungs to get oxygen ( Figure 2). At the same time, the left ventricle contracts after getting blood from the left atrium. When the left ventricle contracts, it pumps blood through the aorta to arteries in all parts of the body.
Figure
Figure 2. Blood Flow from Heart Chambers.
The heart has four valves. Two prevent blood from flowing back between the atriums and ventricles. The other two valves prevent blood from flowing backward from the arteries and into the ventricles.
Normally, the left ventricle pumps one-half or more of the blood in it with each beat. With heart failure, the left ventricle cannot contract strongly enough, pumping two-fifths or less of the blood in it with each beat.
Diagnosis and Evaluation
Your health care team will want to know:
About your symptoms and how long you've had them.
If you have ever had a heart attack, a heart murmur, or other heart problems. If so, how are these problems being treated?
About your general health history and status. What other health problems do you have, and how are they being treated? Are your diet, activities, or exercise restricted? Have family members had heart problems?
About your lifestyle and health habits. What is your daily life like? What do you do to prevent health problems?
If you use tobacco, alcohol, or illegal drugs.
Be honest and candid. Information you share with health care providers is confidential. Evaluating, treating, and managing heart failure depends on accurate information, including facts that only you and your family can provide.
A health history, physical exam, chest x-ray, and electrocardiogram (called ECG or EKG) help diagnose heart failure.
Based on your symptoms and first test results, a test is needed to measure the amount of blood pumped from the heart with each beat (the ejection fraction). Patients with suspected heart failure should undergo echocardiography or radionuclide ventriculography to measure the ejection fraction.
Echocardiography uses sound waves to make images of the heart and its chambers. The procedure is safe and does not require entering the body with any instruments or devices.
Radionuclide ventriculography is a special test that tracks very low doses of a radioactive substance as it travels through the heart. The radioactive substance is safe and completely leaves the body.
A normal heart pumps one-half (50 percent) or more of the blood in the left ventricle with each heartbeat. With heart failure, the weakened heart may pump two-fifths (40 percent) or less, and less blood is pumped with less force to all parts of your body.
Managing Heart Failure
To manage heart failure, follow the instructions of your health care team. You may reduce symptoms and improve how you feel if you take medicines as prescribed and change how you live.
Work with your health care team to make the best choices and set goals to keep life interesting and enjoyable.
Your management plan consists of:
Medicines.
Diet.
Daily activities.
Exercise.
Lifestyle and health habits.
Family support.
If you do not want to change how you live or take medicines as prescribed, tell your health care provider. Explain your reasons to your health care provider.
Work with your health care team to learn how to treat your condition.
Medicines
Importance
Taking medicine every day is vital to treating heart failure. Depending on your symptoms and diagnosis, your doctor may start treatment by prescribing one medicine and then adding others later. Sometimes, treatment will begin with two or more medicines.
It may take several days or weeks to find the right doses of prescribed medicines. Be patient as you and your health care provider work together to find:
The right medicines for you.
The right amount of each one.
The best time of day to take each medicine.
The benefits of these medicines will be lost or reduced if you do not take your medicines as prescribed. Skipping doses or not refilling a medicine's prescription can cause serious problems. Do not take more than the prescribed dose of any medicine.
Be sure to tell your health care provider about other health conditions you have and other medicines you take. These medicines include nonprescription medicines such as aspirin, antacids, and cold remedies.
Side Effects
Any medicine can have unplanned results. If you have any side effects, tell your health care provider right away. He or she can work with you to lessen bothersome effects. If the first medicines prescribed do not work as expected, others are available.
Ask your health care team about side effects caused by taking prescribed medicines with:
Other prescribed medicines.
Medicines you can buy without a doctor's prescription (such as aspirin, antacids, and cold remedies).
Certain foods.
Always report side effects to your health care provider. He or she will know what to do about side effects.
Common Kinds of Medicines
Medicines commonly prescribed for treating heart failure include:
ACE inhibitors (angiotensin-converting enzyme inhibitors) to make it easier for the heart to pump.
Diuretics, or "water pills," to help remove excess fluid and salt from the body.
Digitalis to strengthen each heartbeat, allowing more blood to be pumped.
When other heart or health problems exist with heart failure, your doctor may prescribe additional medicines, such as drugs to lower blood pressure.
ACE inhibitors
ACE inhibitors have been shown to help heart failure patients live longer and feel better. The drugs relax blood vessels and make it easier for the heart to pump. For some people, it may take weeks before they feel better from taking the medicine.
Depending on your initial diagnosis and evaluation, an ACE inhibitor may be the first medicine prescribed. Based on your symptoms, a diuretic and digitalis may be prescribed with the ACE inhibitor or added later.
Captopril, enalapril, lisinopril, and quinapril are generic names for ACE inhibitors now being used for heart failure. Others may be used in the future.
Although most patients take an ACE inhibitor without problems, some patients have side effects. They include:
Cough.
Dizziness.
Skin rash.
Tell your health care provider if any of these symptoms occur.
ACE inhibitors may also produce high potassium levels and affect kidney function. Blood tests are needed to monitor these actions.
If you have any side effects, tell your health care provider right away.
Diuretics
By making you urinate more often, diuretics keep fluid from collecting in your feet, ankles, legs, and abdomen. Skipping doses can cause swelling in these parts of the body and shortness of breath when lying down or during physical activity.
The most commonly used diuretics are hydrochlorothiazide and furosemide (Lasix).
Regular use of some diuretics can lead to the body losing too much potassium and to other imbalances. Blood tests are needed to monitor these levels.
To replace lost potassium, you may have to:
Eat more foods rich in potassium, including bananas and raisins, and drink orange juice and other citrus juices.
Take a prescribed potassium supplement.
Diuretics may also cause:
Leg cramps.
Dizziness or lightheadedness.
Incontinence (accidental urine leakage).
Gout (a type of arthritis).
Skin rash.
Tell your health care provider if you have any of these symptoms. (Urinating more often is not a side effect. It is caused by the diuretic.)
Digitalis
Digitalis helps the heart pump more effectively and may improve your ability to exercise. Prescribed as digoxin or Lanoxin, digitalis is taken daily by many heart patients.
Digitalis has been proven safe for most patients. If too much digitalis is in your body, you may have:
Nausea, loss of appetite.
Mental confusion.
Blurred or yellow-colored vision.
Rapid, forceful heartbeat (palpitations).
Tell your health care provider right away if you have these side effects. Do not stop taking digitalis unless told to do so by your health care provider.
Keeping Track of Your Medicines
Having a system can help tell you when to take medicines, especially if you take several each day. Use the form in the back of this booklet each day to remind you:
Which medicines to take each day.
What each pill looks like.
When to take them.
When each medicine was taken.
Make copies of the blank form in the back for future use.
Always carry with you a list giving the doses of each medicine you take. In an emergency, this information can help medical workers help you.
Cost of Medicines
The retail cost of medicines varies greatly among different pharmacies. If cost is a problem, ask your health care provider or pharmacist if there is a lower cost and acceptable generic form of your medicine. You can also compare prices of different pharmacies and mail-order prescription services.
If needed, financial assistance may be available through social service agencies where you live. You also may qualify for help through programs established by drug companies.
Let your health care provider know if the cost of medicines is a problem. Your health care team can help you apply for assistance.
Diet
In addition to taking medicines, you must change and then monitor your diet. Because salt (sodium) causes fluid to build up in the body, you must restrict salt intake. If you do not, your feet, ankles, legs, and abdomen may swell, and you may find it hard to breathe. If severe, these symptoms may require hospital treatment.
Your health care provider will tell you how much salt, if any, can be in your diet. You and your family may be asked to see a dietitian, nurse specialist, or other health educator for special diet instructions and counseling. They may also suggest new ways to prepare foods and how to modify family recipes. For example, lemon juice and many spices and herbs can add flavor to unsalted foods.
Be especially aware of foods with "hidden" salt such as frozen or canned foods, cheeses, and processed meats. Foods such as hot dogs, salami, and canned soups often contain a lot of salt. Check the nutrition labels for salt content.
If you drink alcoholic beverages, you may have to stop or have only one drink per day. One drink means a glass of beer or wine, or a mixed drink or cocktail containing no more than 1 ounce of alcohol.
Changing your diet can be complicated and confusing. The goal is to reduce salt, and possibly fat, in your food without sacrificing the pleasure of eating. If you have trouble changing your diet, ask your health care team for help.
Watch your weight. Obtain an accurate scale and weigh yourself each morning after urinating, but before eating breakfast or dressing.
If you gain 3 to 5 pounds since last visiting your health care provider, tell him or her promptly. The weight gain may mean your body is retaining fluid.
Daily Activities
How heart failure affects you depends on how severe it is. Mild heart failure may have little effect on work or recreation. Severe heart failure may restrict what used to be easy. Talk to your health care team about:
Work. Can you still work? Full time or part time?
Recreation. Can you go hiking, play golf, swim, and attend sporting events?
Leisure. Can you travel, work in the garden, and do volunteer work?
Sex. Can you have sexual intercourse?
Involve your family members in discussions about activities. They need to know how to support and help you. This is especially true when what you can do changes over time. Some activities (such as work or recreation) may become more difficult while others do not change.
Do not be afraid of discussing private aspects of your life. Your health care team must rely on what you say to help reduce symptoms and improve the quality of your life.
Heart failure means you may have to change your lifestyle and health habits.
As you learn to live with heart failure, you may discover new satisfactions and pleasures. Changes to daily life can be positive and rewarding. Work restrictions may lead to interesting and enjoyable leisure activities. Recreation may become a valuable part of daily life. Sexual relations can be very enjoyable as you and your partner discover less demanding ways to express and share affection.
Exercise
Exercise regularly within your doctor's guidelines. Many people with heart failure say they feel better when they exercise regularly. Usually you can exercise safely at home or in a supervised rehabilitation setting such as a hospital, health club, recreation center, YMCA, or YWCA.
Exercise includes:
Walking.
Cycling.
Swimming.
Low-impact aerobic routines.
Your health care provider will advise you about the right kind and amount of exercise. Find out before starting. You may be asked to see a cardiac rehabilitation specialist to help plan and monitor an exercise program. Also, you may need an exercise stress test to see how much you can do safely.
Lifestyle and Health Habits
Your lifestyle reflects attitudes and values. Health habits involve what you do to reduce chances of illness or injury. Heart failure means you may have to change your lifestyle and health habits.
Examine your lifestyle and health habits. The following changes can reduce the symptoms of heart failure and improve the quality of your life:
Lose weight if you are overweight.
Do not smoke or chew tobacco.
Eliminate or reduce alcohol.
Do not use illegal drugs.
You should also:
Avoid exercise that exceeds your exercise guidelines.
Avoid coming in contact with people who have colds.
Get a flu and pneumonia shot.
You may want to make other changes too, such as learning how to reduce stress. Work with your health care team to decide which choices are best.
Family Support
Your family can be a great source of support and encouragement. As much as possible, include family members in all decisions that affect you. These decisions involve your lifestyle and your ability to work and earn a living. Support by family members can be especially important as you adjust to lifestyle changes and if you face emotional difficulties. Let family members know how they can help.
Family members can help you:
Keep track of medicines.
Prepare special meals.
Exercise.
Find more information on treating heart failure.
Join a support group.
The diagnosis of heart failure may affect your family as much as you. Family support can help you change your lifestyle and health habits.
Chest Pain (Angina)
Some people have chest pain (angina) in addition to heart failure symptoms. Angina is caused by blockage in the coronary arteries. When angina is a symptom, a test called cardiac angiography (heart catheterization with angiography) may be needed.
In this diagnostic procedure, fluid is injected into the coronary arteries through a long, thin tube called a catheter. Special x-rays show where and how much arteries are blocked. Ask your health care provider about expected benefits and risks of the procedure before agreeing to it.
The results of cardiac angiography are usually used to help health care providers plan your care. Treatment may include surgery. Cardiac angiography may not be needed if you do not want heart surgery. Ask your health care provider how information from the procedure will affect your care.
Heart Surgery
If a heart valve problem or coronary artery disease is suspected as the cause of your heart failure, you may be asked to consider heart surgery. Detailed information should be provided. You should know what may result from heart surgery. You should know its:
Benefits.
Risks, including the risks of doing nothing.
Alternatives, including their benefits and risks.
Total cost and how much is paid by insurance.
Before deciding to have surgery, ask for a second opinion from another health care provider. Health insurance often requires a second opinion before surgery.
If heart surgery is a realistic choice for you, seek an experienced surgeon and hospital for the surgery. Ask for information about their success rates and costs before selecting a surgeon and hospital.
Heart Valve Surgery
Repairing or replacing one or more heart valves may be needed if heart failure is caused by heart valve problems. This surgery is common and has proven to be successful in many cases.
Coronary Artery Bypass Graft Surgery and Angioplasty
Coronary artery bypass graft (CABG) surgery is major surgery. In it, veins or arteries from other parts of the body are used to bypass blocked coronary arteries on the heart to restore more normal blood flow to the heart. As a muscle, the heart needs its own blood supply for nourishment so it can pump blood throughout the body.
An alternative to CABG surgery is angioplasty (or PTCA, percutaneous transluminal coronary angioplasty). In this major procedure, a catheter (long, thin tube) is inserted into the arteries on the heart. Inflating the small balloon on the catheter's tip expands the coronary artery and crushes the blockage, restoring blood flow.
Current research indicates that CABG surgery may benefit many people with angina (chest pain) and worsening heart failure resulting from coronary artery disease. The long-term benefits of angioplasty for such patients have not been established by research.
After heart surgery, you must follow a plan for managing and monitoring your heart health.
Heart Transplant Surgery
Heart transplantation is considered only in cases of very severe heart failure. Heart transplants are only performed in specialized centers.
Monitoring Your Progress
Managing heart failure requires keeping track of symptoms and monitoring how well you follow instructions of your health care team. Report changes in your health to your health care provider.
Your Responsibilities
As part of your health care team, you should:
Monitor your general health and report any changes in how you feel.
Report changes in your symptoms.
Take medicines as prescribed and report any side effects.
Follow your guidelines for activities and exercise, and report when you are not able to do an activity or exercise easily.
Follow a prescribed diet.
Report any sudden weight changes.
Family Responsibilities
Your family is part of your health care team. Ask family members for help in monitoring your condition. They should know when to report new symptoms, or a change in symptoms, to your health care provider if you do not.
When calling the health care provider's office, your family should:
Say you are being treated for heart failure.
Describe your symptoms.
Describe what has already been done to bring relief or comfort.
Give the names and amounts of medicines you take.
The Future
Ask your primary care doctor to explain how heart failure is likely to affect your life. Many people adjust to limits imposed by heart failure and still head active live.
Although a sudden change in symptoms is not expected, certain activities may become harder because you are tired and short of breath. If your symptoms do change suddenly, call your health care provider right away.
Emergencies
In an emergency, such as if your heart or breathing stops, acceptance of medical care and treatment is assumed. However, you have a right to accept or refuse any medical care and treatment in advance. You can direct that you do not want emergency medical workers to restore the heartbeat or use special equipment to breathe for you.
Specific instructions for family members and others may be needed so they will know how to react in a medical emergency. A legal document called an advance directive lets others know what to do in a medical emergency. This document states what lifesaving measures you want taken if you cannot think clearly or speak for yourself.
Advance directives include these legal documents:
Living wills.
Medical durable power of attorney.
No cardiopulmonary resuscitation" (CPR) instructions.
Substitute decisionmakers (medical proxies).
If you do not have an advance directive, discuss your medical care and treatment wishes with your family and health care team before preparing one. Ask your health care team or attorney for more information about advance directives. These decisions may be difficult. Your health care team will help you understand how these decisions may affect you. Individual State laws govern the content and use of advance directives.
Support Groups and Counseling
Diagnosis of heart failure can generate a wide range of feelings. You and your family should express these feelings to your health care team. Seek help in dealing with feelings that cause problems.
In addition to professional counseling, local support groups can be a source of help. These groups offer the chance for you to talk about your feelings with other heart patients and families during regular meetings. Support groups may also offer educational programs about heart problems.
Ask your health care team about support groups where you live. If no support group exists, your health care team may help you start one.
Many people adjust to limits imposed by heart failure and still lead active lives.
For more information about support groups for heart patients and their families, contact:
The Mended Hearts, Inc.
7272 Greenville Avenue
Dallas, TX 75231
(214) 706-1442
The Coronary Club, Inc.
9500 Euclid Avenue, E-37
Cleveland, OH 44195
(216) 444-3690
How To Use Your Weekly Medicine Record
Use the weekly medicine record to keep track of what medicines to take every day, when to take them, and when you took them.
Write your name and the date, starting on Sunday, at the top of the record.
Each numbered row is for one medicine. Write the name and dose (amount) of each medicine under the first column. For example: Lanoxin .25 mg. The medicine's name and dose appear on the label of the medicine container.
In the second column, write the size, shape, and color of the pill. For example: Small, round, white pill.
In the third column, write when to take the medicine. For example: Before breakfast.
When you take a medicine, place an x in the column for the day of the week. If you take a medicine more than once a day, mark it each time.
Make copies of the form. Use it every day.
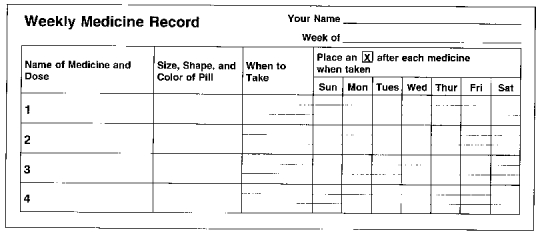
Figure 3. Weekly Medicine Record
Additional Resources
If you want more information about heart failure and its treatment, bookstores and your local public library have helpful books and articles about the subject. Hospitals and health care providers may also have booklets, brochures, videotapes, and audiotapes about heart failure for patients. You may also contact:
The American Heart Association
7272 Greenville Avenue
Dallas, TX 75231-4596
(800) AHA-USA1 (242-8721)
National Heart, Lung, and Blood Institute Information Center Public Health Service
P.O. Box 30105
Bethesda, MD 20824
(301) 251-1222
For More Information
Information in this booklet was taken from Heart Failure: Evaluation and Care of Patients With Left-Ventricular Systolic Dysfunction. Clinical Practice Guideline. The guideline was developed by a private, non-Federal expert panel of physicians, nurses, pharmacists, and consumers. Development of the guideline was sponsored by the Agency for Health Care Policy and Research (AHCPR), an agency of the U.S. Public Health Service. Other guidelines on common health problems have been issued and are under development for release in the future.
For more information on guidelines and to receive more copies of this booklet, call toll free (800) 358-9295 or write to:
AHCPR Publications Clearinghouse
P.O. Box 8547
Silver Spring, MD 20907
AHCPR Publication No. 94-0614.
National Library of Medicine DOCLINE Information: CAT/9436359
- Your Heart
- Purpose of This Booklet
- What Is Heart Failure?
- Your Health Care Team
- How Your Heart's Chambers and Valves Work
- Diagnosis and Evaluation
- Managing Heart Failure
- Chest Pain (Angina)
- Heart Surgery
- Monitoring Your Progress
- The Future
- How To Use Your Weekly Medicine Record
- Additional Resources
- For More Information
-
Living with Heart Disease: Is It Heart Failure? - AHCPR Consumer Guides
Living with Heart Disease: Is It Heart Failure? - AHCPR Consumer GuidesBookshelf
-
Lung-Volume Reduction Surgery for End-Stage Chronic Obstructive Pulmonary Diseas...
Lung-Volume Reduction Surgery for End-Stage Chronic Obstructive Pulmonary Disease - AHCPR Health Technology AssessmentsBookshelf
-
You Can Quit Smoking: Patient Guide - AHCPR Consumer Guides
You Can Quit Smoking: Patient Guide - AHCPR Consumer GuidesBookshelf
-
Magnetic Resonance Angiography: Vascular and Flow Imaging - AHCPR Health Technol...
Magnetic Resonance Angiography: Vascular and Flow Imaging - AHCPR Health Technology AssessmentsBookshelf
-
Minnesota Health Technology Assessments
Minnesota Health Technology AssessmentsBookshelf
Your browsing activity is empty.
Activity recording is turned off.
See more...