NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Agency for Health Care Policy and Research (US). AHCPR Consumer Guides. Rockville (MD): Agency for Health Care Policy and Research (US); 1992-1996.
This publication is provided for historical reference only and the information may be out of date.
Facts About Cancer Pain Treatment
If you are being treated for cancer pain, you may have concerns about your medicine or other treatments. Here are some common concerns people have and the facts about them.
Concern: I can only take medicine or other treatments when I have pain.
Fact: You should not wait until the pain becomes severe to take your medicine. Pain is easier to control when it is mild than when it is severe. You should take your pain medicine regularly and as your doctor or nurse tells you. This may mean taking it on a regular schedule and around-the-clock. You can also use the other treatments, such as relaxation and breathing exercises, hot and cold packs (see pages 8 and 17), as often as you want to.
Concern: I will become "hooked" or "addicted" to pain medicine.
Fact: Studies show that getting "hooked" or "addicted" to pain medicine is very rare. Remember, it is important to take pain medicine regularly to keep the pain under control.
Concern: If I take too much medicine, it will stop working.
Fact: The medicine will not stop working. But sometimes your body will get used to the medicine. This is called tolerance. Tolerance is not usually a problem with cancer pain treatment because the amount of medicine can be changed or other medicines can be added. Cancer pain can be relieved, so don't deny yourself pain relief now.
Concern: If I complain too much, I am not being a good patient.
Fact: Controlling your pain is an important part of your care. Tell your doctors and nurses if you have pain, if your pain is getting worse, or if you are taking pain medicine and it is not working. They can help you to get relief from your pain.
You may have concerns about your treatment that were not discussed here. Talk to your doctor or nurse about your concerns.
Purpose of This Booklet
This booklet is about cancer pain and how it can be controlled. Not everyone with cancer has pain. But those who do can feel better with proper pain treatment.
Reading this booklet should help you to:
Learn why pain control is important to you.
Work with your doctors and nurses to find the best method to control your pain.
Talk to your doctors and nurses about your pain and how well the treatment is working for you.
Why Pain Should Be Treated
Pain can affect you in many ways. It can keep you from being active, from sleeping well, from enjoying family and friends, and from eating. Pain can also make you feel afraid or depressed.
When you are in pain or uncomfortable, your family and friends may worry about you.
With treatment, most cancer pain can be controlled. When there is less pain, you will probably feel more active and interested in doing things you enjoy.
If you have cancer and you are feeling pain, you need to tell your doctor or nurse right away. Getting help for your pain early on can make pain treatment more effective.
What Causes Cancer Pain?
There are many causes of cancer pain. Most of the pain of cancer comes when a tumor presses on bone, nerves, or body organs. Cancer treatment can cause pain, too.
You may also have pain that has nothing to do with your illness or its treatment. Like everyone else, you can get headaches, muscle strains, and other aches and pains. Because you may be taking medicine for cancer treatment or pain, check with your doctor or nurse on what to take for these everyday aches and pains.
Other conditions, such as arthritis, can cause pain, too. Pain from these other conditions can be treated along with cancer pain. Again, talk to your doctors and nurses about your medical history. They will be able to tell you how each condition can be treated and what is best for you.
Treating Cancer Pain
Cancer pain is usually treated with medicine. But surgery, radiation therapy, and other treatments can be used along with medicine to give even more pain relief (these treatments are listed on page 8). Ask your doctor or nurse how the other treatments can help you.
Choosing the Right Medicine
Pain treatments work differently for different people. Even when a doctor or nurse uses the right medicines and treatments in the right way, you may not get the pain relief you need. While you are being treated for your pain, tell your doctors and nurses how you feel and if the treatments help. The information you give them will help them to help you get the best pain relief.
Your doctors and nurses will work to find the right pain medicine and treatments for you. You can help by talking with them about:
Pain medicines you have taken in the past and how well they have worked for you.
Medicines and other treatments (including health foods, vitamins, and other "nonmedical" treatments) you are taking now. Your doctor or nurse needs to know about other treatments you are trying and other medicines you take. This is important because some treatments and medicines do not work well together. Your doctors and nurses can find medicines that can be taken together.
Allergies that you have, including allergies to medicines.
Fears and concerns that you have about the medicine or the treatment.Talk to your doctors and nurses about your fears and concerns. They can answer your questions and help you to understand your pain treatment.
Types of Pain Medicine
Many medicines are used to treat cancer pain, and your doctor may give you one or more of them to take. The list below describes the different types of medicine that you may be taking and the kind of pain they work on. Ask your doctor or nurse to tell you more about the medicine you are taking.
Do not start to take a new medicine without checking with your doctor or nurse first. Even aspirin can be a problem in some people who are taking other medicines or having cancer treatment.
For mild to moderate pain --
Nonopioids: Acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen. You can buy many of these over-the-counter (without a prescription). Others need a prescription.
For moderate to severe pain --
Opioids: Morphine, hydromorphone, oxycodone, and codeine. A prescription is needed for these medicines. Nonopioids may also used along with opioids for moderate to severe pain.
For tingling and burning pain --
Antidepressants: Amitriptyline, imipramine, doxepin, trazodone. A prescription is needed for these medicines. Taking an antidepressant does not mean that you are depressed or have a mental illness.
Anticonvulsants: Carbamazepine and phenytoin. A prescription is needed for these medicines. Taking an anticonvulsant does not mean that you are going to have convulsions.
For pain caused by swelling --
Steroids: Prednisone, dexamethasone. A prescription is needed for these medicines.
(For more information on pain medicines, see pages 14-15.)
About Side Effects
All medicines can have some side effects, but not all people get them. Some people have different side effects than others. Most side effects happen in the first few hours of treatment and gradually go away. Some of the most common side effects of pain medicines are:
Constipation(not being able to have a bowel movement). The best way to prevent constipation is to drink lots of water, juice, and other liquids, and to eat more fruits and vegetables. Exercise also helps to prevent _constipation. Your doctor or nurse may also be able to give you a stool softener or a laxative.
Nausea and vomiting.When this happens, it usually only lasts for the first day or two after starting a medicine. Tell your doctors and nurses about any nausea or vomiting. They can give you medicine to stop these side effects.
Sleepiness.Some people who take opioids feel drowsy or sleepy when they first take the medicine. This usually does not last too long. Talk to your doctor or nurse if this is a problem for you.
Slowed breathing.This sometimes happens when the dose of medicine is increased. Your doctor or nurse can tell you what to watch for and when to report slowed breathing.
More serious side effects of pain medicines are rare. As with the more common side effects, they usually happen in the first few hours of treatment. They include trouble breathing, dizziness, and rashes. If you have any of these side effects, you should call your doctor or nurse right away.
How Pain Medicine is Taken
Most pain medicine is taken by mouth (orally). Oral medicines are easy to take and usually cost less than other kinds of medicine. Most oral medicines are in tablet form, but sometimes they are liquids that you drink. If it is hard for you to swallow and you cannot take a tablet or liquid for some other reason, there are other ways to get these medicines. These include:
Rectal suppositories(medicine that dissolves in the rectum and is absorbed by the body).
Patches that are filled with medicine and placed on the skin(transdermal patches).
Injections.There are many kinds of injections to give pain relief. Most injections use a tube or needle to place medicine directly into the body. These include:
Subcutaneous injection -- medicine is placed just under the skin using a small needle.
Intravenous injection -- medicine is placed directly into the vein through a needle that stays in the vein.
Epidural or intrathecal injections -- medicine is placed directly into the back using a small tube. Most of these injections give pain relief that lasts for many hours.
Subdermal and intramuscular injections -- commonly known as "shots," are injections that are placed more deeply into the skin or muscle using a needle. These injections are not recommended for long-term cancer pain treatment. Constantly having shots into the skin and muscle can be painful. Also, shots take longer to work, and you have to wait for them.
When To Take Your Pain Medicine
To help your pain medicine work best:
Take your medicine on a regular schedule (by the clock). Taking medicine regularly and as your doctor tells you will help to keep pain under control. Do not skip a dose of medicine or wait for the pain to get worse before taking your medicine.
Ask your doctor or nurse how and when to take extra medicine. If some activities make your pain worse (for example, riding in a car), you may need to take extra doses of pain medicines before these activities. The goal is to PREVENT the pain. Once you feel the pain, it is harder to get it under control.
Treating pain is important, and there are many medicines and treatments that can be used. If one medicine or treatment does not work, there is another one that can be tried. Also, if a schedule or way that you are taking the medicine does not work for you, changes can be made. Talk to your doctors and nurses because they can work with you to find the pain medicine that will help you the most.
It may be helpful for you to keep a record of how the medicine is working. Keeping a record like the one on pages 18-19 and sharing it with your doctor or nurse will help to make your treatment more effective.
Other Treatments
Your doctor or nurse may recommend that you try other treatments along with your medicine to give you even more pain relief. Relaxation exercises (see page 17) help reduce pain. Many people find that cold packs, heating pads, massage, and rest help to relieve pain. Music or television may distract you from the pain. Your family members may want to help you to use these treatments. These treatments will help to make your medicines work better and relieve other symptoms, but they should not be used instead of your medicine.
Nondrug Treatments of Pain
Here are a few examples of treatments that can help to relieve your pain. You may use these treatments along with your regular medicine:
Biofeedback.
Breathing and relaxation.
Imagery.
Massage, pressure, vibration.
Transcutaneous electrical nerve stimulation (TENS).
Distraction.
Hot or cold packs.
Rest.
Talk to your doctors and nurses about these treatments. They will be able to give you more information. Also, the counseling and support groups listed on page 16 may be able to tell you more.
When Medicine Is Not Enough
Some patients have pain that is not relieved by medicine. In these cases other treatments can be used to reduce pain:
Radiation therapy.This treatment reduces pain by shrinking a tumor. A single dose of radiation may be effective for some people.
Nerve blocks.Pain medicine is injected directly around a nerve or into the spine to block the pain.
Neurosurgery.In this treatment pain nerves (usually in the spinal cord) are cut to relieve the pain.
Surgery.When a tumor is pressing on nerves or other body parts, operations to remove all or part of the tumor can relieve pain.
Talk to your doctor about other pain treatments that will work for you.
The First Step
The key to getting the best pain relief is talking with your doctors and nurses about your pain. They will want to know how much pain you feel, where it is, and what it feels like. Answering the questions below may help you describe your pain. You may wish to write your answers in the space after each question.
Where is the pain?You may have pain in more than one place. Be sure to list all of the painful areas.
What does the pain feel like?Does it Ache? Throb? Burn? Tingle? You may wish to use other words to describe your pain.
How bad is the pain?You can also use a number scale and rate your pain from 0 to 10: 0 means no pain and 10 means the worst pain. You may want to use the pain intensity scale on page 19 to put a number to your pain. You can also describe your pain with words like none, mild, moderate, severe, or worst possible pain.
What makes the pain better or worse?You may have already found ways to make your pain feel better. For example, using heat or cold, or taking certain medicines. You may have also found that sitting or lying in certain positions or doing some activities affects the pain.
If you are being treated for pain now, how well is the treatment working? You may want to describe how well the treatment is working by saying how much of the pain is relieved all, almost all, none, etc.
Has the pain changed?You may notice that your pain changes over time. It may get better or worse or it can feel different. For example, the pain may have been a dull ache at first and has changed to a tingle. It is important to report changes in your pain. Changes in pain do not always mean that the cancer has come back or grown. Describe how the pain was before and how it is now.
After talking with you about your pain, your doctor or nurse may want to examine you or order x-rays or other tests.
These tests will help the doctor or nurse find the cause of your pain.
Having a Plan
You can work with your doctor or nurse to write a pain control plan to meet your needs. In a pain control plan, you and your doctor or nurse plan your pain control activities. This will include when to take your medicine, how and when to take extra medicine, and other things you can do to ease and prevent your pain. Your doctor or nurse may also list the medicines and other treatments you can use to help you with any side effects or other aches and pains, such as headaches. A sample pain control plan that you can use is on pages 20-21.
Making the Plan Work
Some people find that the first pain control plan does not work for them. You and your doctor or nurse can change your pain control plan at any time. Here are some questions to ask yourself about the pain plan:
Is the pain plan hard to follow?
Is there any part of the plan that is hard to understand?
Are you pleased with the pain control?
Are you having trouble getting the medicine?
Are you having trouble taking the medicine?
Are you having side effects from the medicine?
Is the medicine or the treatment causing a problem for you or your family?
Are the nondrug treatments working for you?
Write any other questions you have for your doctor or nurse below.
Benefits and Risks of Treatment
This booklet talks about many different treatments for cancer pain. It also talks about side effects of medicines. Information about benefits and risks (side effects) of medicines may also be important to you. The list below describes the benefits and risks of the different types of medicines described on pages 4-5.
Nonopioids
Benefits: Control mild to moderate pain. Some can be bought without a prescription.
Risks: Some of these medicines can cause stomach upset. They can also cause bleeding in the stomach, slow blood clotting, and cause kidney problems. Acetaminophen does not cause these side effects, but high doses of it can hurt the liver.
Opioids
Benefits:These medicines control moderate to severe pain and do not cause bleeding.
Risks:May cause constipation, sleepiness, nausea and vomiting. Opioids sometimes cause problems with urination or itching. They may also slow breathing, especially when they are first given, but this is unusual in people who take opioids on a regular basis for pain.
Antidepressants
Benefits:Antidepressants help to control tingling or burning pain from damaged nerves. They also improve sleep.
Risks:These medicines may cause dry mouth,sleepiness,and constipation. Some cause dizziness and lightheadedness when standing up suddenly.
Anticonvulsants
Benefits:Help to control tingling or burning from nerve injury.
Risks:May hurt the liver and lower the number of red and white cells in the blood. It is important to have regular blood tests to check for these effects.
Steroids
Benefits:Help relieve bone pain, pain caused by spinal cord and brain tumors, and pain caused by inflammation. Steroids also increase appetite.
Risks:May cause fluid to build up in the body. May also cause bleeding and irritation to the stomach. Confusion is a problem for some patients when taking steroids.
Counseling and Peer Support
Pain can make you feel many emotions. You may feel sad, helpless, vulnerable, angry, depressed, lonely, isolated, or other emotions. Lots of people feel these things when they are in pain. Often, when the pain is successfully treated, these feelings lift. Many people who have had cancer feel that counseling, religious, and other support groups have helped them to get back a sense of control and well being.
To find out more about support groups and to receive books and pamphlets about cancer pain, call or write to:
National Cancer Institute
Cancer Information Service
800-4-CANCER
Ask for the booklet Questions and Answers About Pain Control.
American Cancer Society
800-ACS-2345
The booklet Questions and Answers About Pain Control is also available from this group.
Wisconsin Cancer Pain Initiative
Medical Science Center, Room 3675
University of Wisconsin
Medical School
1300 University Avenue
Madison, WI 53706
608-262-0978
For adults, ask for Cancer Pain Can Be Relieved.
For children with cancer pain, ask for Children's Cancer Pain Can Be Relieved.For adolescents with cancer pain, ask for Jeff Asks About Cancer Pain.
Slow Rhythmic Breathing For Relaxation
Deep breathing exercises can help relax you. These exercises may work along with your medicine to lessen or relieve your pain.
Breathe in slowly and deeply.
As you breathe out slowly, feel yourself beginning to relax; feel the tension leaving your body.
Now breathe in and out slowly and regularly, at whatever rate is comfortable for you.
To help you focus on your breathing and breathe slowly and rhythmically: (a) breathe in as you say silently to yourself, "in, two, three"; (b) breathe out as you say silently to yourself, "out, two, three." or Each time you breathe out, say silently to yourself a word such as "peace" or "relax."
Do steps 1 through 4 only once or repeat steps 3 and 4 for up to 20 minutes.
End with a slow deep breath. As you breathe out say to yourself "I feel alert and relaxed."
Pain Control Record
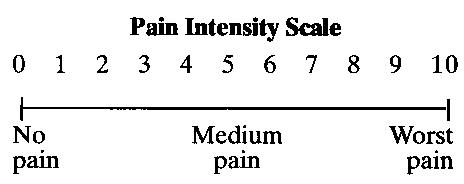
You can use a chart like this to rate your pain and to keep a record of how well the medicine is working. Write the information in the chart. Use the pain intensity scale to rate your pain before and after you take the medicine.
Pain Control Plan
Pain control plan for
______________________________________________
At home, I will take the following medicines for pain control:
Medicine How to take How many How often Comments
_________ ___________ ________ _________ _______________
_________ ___________ ________ _________ _______________
_________ ___________ ________ _________ _______________
Medicines that you may take to help treat side effects:
Medicine How to take How many How often Comments
_________ ___________ ________ _________ _______________
_________ ___________ ________ _________ _______________
_________ ___________ ________ _________ _______________
Constipation is a very common problem when taking opioid medications.
When this happens, do the following:
- Increase fluid intake (8 to 10 glasses of fluid per day).
- Exercise regularly.
- Increase fiber in the diet (bran, fresh fruits, vegetables).
====================================================
Use a mild laxative, such as milk of magnesia,
if no bowel movement in 3 days.
====================================================
Take ____________________every day at______________(time) with a full
glass of water.
Use a glycerin suppository every morning (this may help make a bowel
movement less painful).
Nondrug pain control methods:
______________________________________________
______________________________________________
______________________________________________
Additional instructions:
______________________________________________
______________________________________________
______________________________________________
Important phone numbers:
Your doctor_________________________________
Your nurse _________________________________
Your pharmacy_______________________________
Emergencies_________________________________
Call your doctor or nurse immediately if your pain increases or if you
have new pain. Also call your doctor early for a refill of pain medicines.
Do not let your medicines get below 3 or 4 days' supply.
For Further Information
The information in this booklet was taken from the Clinical Practice Guideline on Management of Cancer Pain. The guideline was written by a panel of private-sector experts sponsored by the Agency for Health Care Policy and Research. Other guidelines on common health problems are being developed.
To order a single copy of this booklet call the National Cancer Institute, Cancer Information Service at: 800-4-CANCER
or write to:
Cancer Pain Guideline
AHCPR Publications Clearinghouse
P.O. Box 8547
Silver Spring, MD 20907
AHCPR Publication No. 94-0595.
National Library of Medicine DOCLINE Information: CAT9423489
- Facts About Cancer Pain Treatment
- Purpose of This Booklet
- Why Pain Should Be Treated
- What Causes Cancer Pain?
- Treating Cancer Pain
- Choosing the Right Medicine
- Types of Pain Medicine
- About Side Effects
- How Pain Medicine is Taken
- When To Take Your Pain Medicine
- Other Treatments
- Nondrug Treatments of Pain
- When Medicine Is Not Enough
- The First Step
- Having a Plan
- Making the Plan Work
- Benefits and Risks of Treatment
- Counseling and Peer Support
- Slow Rhythmic Breathing For Relaxation
- Pain Control Record
- Pain Control Plan
- For Further Information
-
Managing Cancer Pain - AHCPR Consumer Guides
Managing Cancer Pain - AHCPR Consumer GuidesBookshelf
-
Computed Tomographic Scanning of the Brain - NIH Consensus Statements
Computed Tomographic Scanning of the Brain - NIH Consensus StatementsBookshelf
-
Polysomnography and Sleep Disorder Centers - AHCPR Health Technology Assessments
Polysomnography and Sleep Disorder Centers - AHCPR Health Technology AssessmentsBookshelf
-
Depression in Primary Care: Detection, Diagnosis, and Treatment - AHCPR Quick Re...
Depression in Primary Care: Detection, Diagnosis, and Treatment - AHCPR Quick Reference GuidesBookshelf
-
Supportive Therapy in Burn Care - NIH Consensus Statements
Supportive Therapy in Burn Care - NIH Consensus StatementsBookshelf
Your browsing activity is empty.
Activity recording is turned off.
See more...