NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Agency for Health Care Policy and Research (US). AHCPR Quick Reference Guides. Rockville (MD): Agency for Health Care Policy and Research (US); 1992-1996.
This publication is provided for historical reference only and the information may be out of date.
Attention Clinicians:
The Clinical Practice Guideline on which this Quick Reference Guide for Clinicians is based was developed by an interdisciplinary, non-Federal panel comprised of health care professionals and a consumer representative. Panel members were:
A. John Rush, MD (Chair)
William E. Golden, MD
Gladys Walton Hall, PhD, MSW
Col. Moses Herrara, MD
Artie Houston
Roger Kathol, MD
Wayne Katon, MD
Catherine L. Matchett, MD
Frederick Petty, PhD, MD
Herbert C. Schulberg, PhD
G. Richard Smith, Jr., MD
Gail Wiscarz Stuart, PhD, RN, CS
For a description of the guideline development process and information about the sponsoring agency (Agency for Health Care Policy and Research), see the Clinical Practice Guideline, Depression in Primary Care: Volume 1. Detection and Diagnosis (AHCPR Publication No. 93-0550) and Volume 2. Treatment of Major Depression (AHCPR Publication No. 93-0551). To receive additional copies of the Clinical Practice Guideline, Quick Reference Guide for Clinicians (AHCPR Publication No. 93-0552) and a patient booklet (AHCPR Publication No. 93-0553), call toll free 800-358-9295 or write the AHCPR Publications Clearinghouse, P.O. Box 8547, Silver Spring, MD 20907.
The panel's inferences as to what is optimal patient care are not expected to apply to all patients or situations. Knowledge developed through research can only provide a starting point for approaching a particular patient. Algorithms and flow charts are not applicable in every case. They do, however, provide coarse road maps for managing certain patients. Practitioners must use their own judgment in adapting guidelines to particular patients.
Note: This Quick Reference Guide for Clinicians contains excerpts from the Clinical Practice Guideline, Vols. 1 and 2. It was not designed to stand on its own. Practitioners should review the Clinical Practice Guideline carefully to become familiar with the diagnosis, differential diagnoses, and treatment options for patients with major depressive disorder and then use the Quick Reference Guide to help them remember the major decision points in diagnosing and treating major depressive disorder. If the information contained in these documents is insufficient to evaluate the condition of a particular patient, the practitioner is advised to seek a consultation.
Purpose and Scope
A depressed (sad) mood is a normal reaction to disappointments or losses. A sad mood is not to be confused with major depressive disorder, one of several forms of clinical depression, which is a serious medical condition with major public health consequences. About 15 percent of the general public will suffer from major depressive disorder sometime in their life, but the disorder will be accurately diagnosed and treated in fewer than one in three. A person with major depressive disorder suffers intense mental, emotional, and physical anguish, and substantial disability. The depression disrupts family, job, and social functioning. Depression worsens the prognosis for other general medical illnesses. The worst consequence of untreated major depressive disorder is suicide.
Depression is viewed by many patients and the lay public as evidence of a character defect or lack of will power. Thus, those with major depressive disorder must endure the additional burden of having an illness that society views as the reflection of an inherent personal weakness or fault. The practitioner should be sensitive to these issues, provide support, and become a patient advocate. In many cases, the diagnosis and treatment of major depressive disorder can be successfully accomplished by primary care practitioners. When psychotherapy is called for, it may be conducted in either a primary care or specialized setting, depending on the availability of a trained, competent therapist. The primary care practitioner should emphasize to the patient, who is already suffering inappropriate guilt, that major depression is a medical condition that can be successfully treated. Guideline Highlights
The following step-wise process can assist primary care practitioners in detecting, diagnosing, and treating major depression.
Guideline Highlights
1. Maintain a high index of suspicion and evaluate risk factors
Surveys consistently show that 6 to 8 percent of all outpatients in primary care settings have major depressive disorder; women are at particular risk for depression. Although sadness is frequently a presenting sign of depression, not all patients complain of sadness, and many sad patients do not have major depression. Common complaints of patients in primary care settings with major depressive disorder include:
Pain--including headaches, abdominal pain, and other body aches.
Low energy--excessive tiredness, lack of energy or a reduced capacity for pleasure or enjoyment.
A mood of apathy, irritability, or even anxiety rather than, or in addition to, any overt sadness may be present.
Sexual complaints--problems with sexual functioning or desire.
The clinician should be doubly alert to the likelihood of depression in individuals under age 40.
Additional clinical clues that raise the likelihood of a major depressive disorder include:
Prior episodes of depression.
A family history of major depressive or bipolar disorder.
A personal or family history of suicide attempt(s).
Concurrent general medical illnesses.
Concurrent substance abuse.
Symptoms of fatigue, malaise, irritability, or sadness.
Recent stressful life events and lack of social supports. (Stress should not be used to "explain away" depression; stress may precipitate a depression in some cases.)
2. Detect depressive symptoms with a clinical interview
Major depressive disorder is a syndrome consisting of a constellation of signs and symptoms that are not normal reactions to life's stress. A sad or depressed mood is only one of the several possible signs and symptoms of major depressive disorder. The clinician may find it useful to provide the patient with a written list of depressive symptoms (pages 3 and 4) and ask the patient to indicate any symptoms experienced. This patient self-report can increase the likelihood of detecting major depression.
Diagnosis
Diagnostic criteria for major depressive disorder
For major depressive disorder, at least five of the following symptoms are present during the same time period, and at least one of the first two symptoms must be present. In addition, symptoms must be present most of the day, nearly daily, for at least 2 weeks.
Depressed mood most of the day, nearly every day.
Markedly diminished interest or pleasure in almost all activities most of the day, nearly every day (as indicated either by subjective account or observation by others of apathy most of the time).
Significant weight loss/gain.
Insomnia/hypersomnia.
Psychomotor agitation/retardation.
Fatigue (loss of energy).
Feelings of worthlessness (guilt).
Impaired concentration (indecisiveness).
Recurrent thoughts of death or suicide.
All depressed patients should be assessed for the risk of suicide by direct questioning about suicidal thinking, impulses, and personal history of suicide attempts. Patients are reassured by questions about suicidal thoughts and by education that suicidal thinking is a common symptom of the depression itself and not a sign that the patient is "crazy." Table 1 lists the risk factors associated with completed suicide.
Table
Table 1. Suidice risk Factors.
If suicide is a distinct risk (specific plans, or significant risk factors exist), consult a mental health specialist immediately. The patient may need specialized care or hospitalization.
Bipolar illness
A small percentage of patients with major depressive disorder have bipolar illness. These patients experience mood cycles with discrete episodes of depression and mania. In between episodes, they may feel perfectly normal.
Diagnostic criteria for mania
For mania, at least four of the following symptoms, including the first one listed, must be present for a period of at least 1 week.
A distinct period of abnormally and persistently elevated, expansive, or irritable mood
Less need for sleep.
Talkative or feeling pressure to keep talking.
Distractibility.
Flight of ideas.
Increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation.
Inflated self-esteem or grandiosity.
Excessive involvement in pleasurable activities which have a high potential for painful consequences (buying sprees, sexual indiscretions, or foolish business investments).
3. Diagnose the mood disorder using clinical history and interview
Many patients are aware of only some symptoms and may minimize their disability. Interviewing someone who knows the individual well (a spouse, close friend, or relative) can be extremely valuable in obtaining an accurate picture of the patient's symptoms, degree of disability, and course of illness.
4. Evaluate patients with a complete medical history and physical examination
The patient's initial complaints should be evaluated thoroughly with a medical review of systems and a physical examination. If no cause or associated factors can be found for the initial presenting medical complaint, diagnose the patient for a primary mood syndrome.
5. Identify and treat potential known causes (if present) of mood disorder
Approximately 10-15 percent or more of major depressive conditions are caused by general medical illnesses or other conditions (See Figure 2). Generally, the principle is to treat the associated condition first. If the depression persists after treatment of the associated condition, major depressive disorder should be diagnosed and treated.
Figure
Figure 2. Conditions associated with mood symptoms of major depressive episodes.
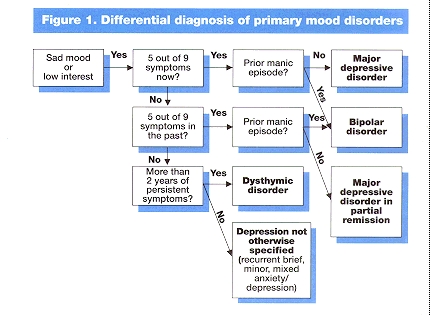
Figure 1. Differential diagnosis of primary mood disorders
Potential associated conditions include
Substance abuse
Too much alcohol, use of illicit drugs, or abuse of prescription medicines can cause or complicate a major depressive episode. In most cases, once the substance has been discontinued, the depression lifts (Figure 3).
Figure
Figure 3. Relationship between major depressive and other current psychiatric disorders.
Concurrent medication
Depression may be an idiosyncratic side effect of many medications. However, the clinician should be aware that this effect is uncommon and usually occurs within days to weeks of starting the medication. Current evidence clearly implicates only reserpine, glucocorticoids, and anabolic steroids with the de novo development of depression as a potential side effect of the drug. Changing to a different medication often relieves the depression (Figure 4).
Figure
Figure 4. Relationship between major depressive and other current general medical disorders.
General medical disorders
Depression can occur in the presence of another general medical condition (Figure 4) (most commonly, autoimmune, neurologic, metabolic, infectious, oncologic, and endocrine disorders, among others). There are several possibilities in such cases:
The general medical disorder biologically causes or triggers a depression; for example, hypothyroidism can be accompanied by depressive symptoms. In this case, treat the general medical disorder first.
The general medical disorder psychologically results in depression; for example, a patient with cancer may become clinically depressed as a reaction to the prognosis, pain, or incapacity, although most patients with cancer do not suffer a major depressive episode. In this case, treat the depression as an independent disorder.
The general medical disorder and the mood disorder are not causally related. In this case, treat the depression.
Other causal nonmood psychiatric disorders
These generally include eating disorders, obsessive-compulsive disorder, and some cases of panic disorder (Figure 3).
When generalized anxiety disorder co-exists with major depression, treatment should be directed toward the major depression first.
If panic disorder is present only during major depressive episodes, the major depression is treated first.
If panic disorder and major depression are both present and the panic disorder has been present without episodes of major depression in the past, the clinician must judge which is the most significant condition (e.g., by family history, the level of current disability attributable to each, and the prior course of illness) and treat that condition Figure 3. Relationship between major depressive and other current psychiatric disorders.
If a "personality disorder" is suspected, the major depressive disorder is treated first, whenever feasible.
Grief reaction
It is important to differentiate a normal grief reaction from depression. A normal grief reaction persists for 2 to 6 months and improves steadily without specific treatment. Most grief reactions do not meet criteria for a major depressive episode. Grief reactions are usually seen by patients as normal and appropriate. While unpleasant, they rarely cause significant and prolonged impairment in work or other functions. Some individuals experience symptoms of depression along with the grief reaction. If the major depressive episode persists for more than 2 months after the loss, a major depressive disorder should be diagnosed and treated.
6. Reevaluate for mood disorders
If the depression persists after treatment of the associated psychiatric general medical, or substance abuse disorders, the depression should be diagnosed and treated.
7. Develop a treatment plan with the patient
If the mood disorder is still present, or if associated conditions do not exist, work with the patient to treat the primary mood disorder.
Treatment of depression consists of three phases (Figure 5):
Acute treatment (6 to 12 weeks) aims at remission of symptoms. A partial response (not a complete remission) is associated with a poorer prognosis.
Continuation treatment (4 to 9 months) aims at prevention of relapse. During this phase, medication should be continued at the full dosage. Continuation phase psychotherapy may be helpful for selected individuals.
Maintenance treatment aims at prevention of recurrence in patients with prior episodes. Only maintenance medication prevents a new episode (recurrence). Maintenance psychotherapy may delay the next episode
Figure
Figure 5. Phases of treatment for major depression.
The objective of treatment is for the patient to reach a sustained asymptomatic state. Figure 6 presents a flow diagram for the treatment of depression. These principles apply no matter what treatment is selected. The essential features of this plan include:
Patient education prior to treatment (page 10).
Regular monitoring for side effects.
Regular monitoring of the patient's depressive symptoms.
Adjustment or changes in the treatment plan if response is not timely or complete.

Figure
Figure 6. Overview of treatment for depression.
Patient Education
The effectiveness of any treatment rests on a cooperative effort by patient and practitioner. The patient should be told of the diagnosis, prognosis, and treatment options, including costs, duration, and potential side effects. In presenting patient and family education in the clinical management of depression, it is useful to present the following information:
Depression is a medical illness, not a character defect or weakness.
Recovery is the rule, not the exception.
Treatments are effective, and there are many options for treatment. An effective treatment can be found for nearly all patients.
The aim of treatment is complete symptom remission, not just getting better, but getting and staying well.
The risk of recurrence is significant: 50 percent after one episode, 70 percent after two episodes, 90 percent after three episodes.
Patient and family should be alert to early signs and symptoms of recurrence and seek treatment early if depression returns.
8. Select the most appropriate acute phase treatment
The aim of acute phase treatment is symptom remission. Treatment of depression in the primary care setting includes:
Medication.
Psychotherapy.
Combined treatment of medication and psychotherapy.
The choice of treatment modality is based primarily on the history of illness and the severity of the major depressive episode. The following general definitions may be helpful in determining an appropriate treatment:
Severe depression is present when a person has nearly all of the symptoms of depression, and the depression almost always keep them from doing their regular day-to-day activities.
Moderate depression is present when a person has many symptoms of depression that often keep them from doing things that they need to do.
Mild depression is present when a person has some of the symptoms of depression, and it takes extra effort to do the things they need to do.
Medication
Scientific evidence indicates that over 50 percent of depressed outpatients who begin treatment with antidepressant medication experience marked improvement or complete remission of their depressive symptoms. Considerations for acute phase treatment with medication are:
More severe symptoms.
Chronicity.
Recurrent episodes (two prior episodes indicate treatment with medication.)
Presence of psychotic features (hallucinations or delusions).
Presence of melancholic symptoms.
Family history of depression.
Prior response to medication treatment.
Incomplete response to psychotherapy alone.
Patient preference.
Psychotherapy
Scientific evidence indicates that several forms of short-term psychotherapy (cognitive, interpersonal, or behavioral) are effective in treating most cases of mild or moderate depression. Other types of psychotherapy may also be helpful in the treatment of major depressive disorder, although their efficacy has not been evaluated fully, if at all. In individuals with mild to moderate depressions, time-limited psychotherapies appear equal in efficacy to antidepressant medications.
Considerations for acute phase treatment with psychotherapy alone include:
Less severe depression.
Less recurrent, chronic, or disabling depression.
Absence of psychotic symptoms.
Patient preference.
Prior positive response to psychotherapy.
Incomplete response to medication alone.
Chronic psychosocial problems.
Medication contraindicated or refused.
Psychotherapy requires the availability of an experienced mental health specialist, such as a psychiatrist, psychologist, social worker, psychiatric nurse, or other professional trained in psychotherapy.
Combined treatment
Combined treatment (medication plus formal psychotherapy) should be considered in various situations, including:
More severe depression
Recurrent depression with poor interepisode recovery.
Incomplete therapeutic response to either medication or psychotherapy.
Evidence of a significant personality disorder, usually evidenced by prior poor interepisode recovery, partial response to medication, or marked adherence problems.
Patient preference.
9. If medication is used, select the type and dose best suited to the patient
Primary care providers will find it useful to become familiar with one drug with minimal side effects from each of the major classes of antidepressants (Tables 2 and 3).
Table
Table 2. Side-effect profiles of antidepressant medications.
Table
Table 3. Pharmacology of antidepressant medications.
Medications should be individualized to the patient in order to optimize treatment benefit and lower risk. Factors to be considered include:
Possibility of short- and long-term side effects.
History of response or nonresponse.
Consideration of possible drug interactions.
Presence of other psychiatric and general medical conditions.
Patient age. Elderly patients are at much higher risk for concomitant general medical disorders and should, therefore, receive a more thorough medical evaluation prior to treatment.
Patients at risk of experiencing adverse drug interactions or with other medical illnesses may need lower than recommended dosages. Geriatric patients often require lower dosages of medication, and dosage increments should be made slowly.
Bipolar disorder
Treatment of patients with bipolar disorder while they are in the depressed phase should be done with knowledge of the risk of inducing mania with antidepressant medications. Consultation with a psychiatrist may be considered if there is suspicion of bipolar illness.
Psychotic depression
Treatment of the patient with psychotic symptoms (hallucinations, delusions) often involves hospitalization, neuroleptics, or electroconvulsive therapy. A consultation or referral to a mental health specialist is recommended.
10. Evaluate treatment response
Whether medication, psychotherapy, or a combination are used, evaluate the patient's response to treatment.
Medication
Adequate response—
Many patients will respond to an adequate trial of the first drug tried.
Inadequate response --
Figure 7 summarizes the steps in managing partial or nonresponse to medication. If inadequate response is a problem, the following steps may be taken:
Reevaluate the diagnosis.
Evaluate for side effects.
Inquire about medication adherence.
Determine the need for increased dosing. For tricyclic agents, the primary cause of inadequate response is insufficient dosing. In selected cases, it may be useful to obtain blood drug levels to gauge dosing. (Minimal therapeutic blood levels have been fairly well documented for nortriptyline, desipramine, imipramine, and amitriptyline.)
Change medication. Patients who do not respond to the initial medication trial are likely to respond to an alternate drug from a different class. If the patient still does not respond after a trial on a second drug, consultation with a mental health specialist should be strongly considered (Figure 7).
Add or change to psychotherapy. Patients who cannot tolerate medication or who have only a partial response (with residual cognitive symptoms) in mild to moderate depression may benefit from time-limited psychotherapy (Figure 7).
Figure
Figure 7. Six-week evaluation: partial or nonresponders to medication.
Psychotherapy
A significant number (50 percent) of patients with mild to moderate forms of depression obtain substantial symptom relief with psychotherapy. Many patients begin to feel the effects of psychotherapy in the first few weeks. Full remission rather than improvement is the objective of treatment. If there is no symptom improvement at all within 6 weeks, the choice of treatment modality should be reevaluated. For patients who improve but who are still symptomatic after 12 weeks, treatment with medication is a strong consideration.
11. Proceed to continuation phase treatment
Once the patient has responded to acute phase treatment with medication, continuation treatment is indicated. If acute phase psychotherapy alone was effective, continuation treatment with psychotherapy may be useful in selected cases. The aim of continuation treatment is to prevent the return of the most recent depressive episode (a relapse). The following principles apply:
If the acute phase treatment included medication, continuation medication is always called for (Figure 8). The dosage is the same as that used in acute treatment. Medication visits can be extended to once every 2 to 3 months for most patients.
If psychotherapy alone constituted acute treatment, the patient remitted, and psychosocial function was restored, psychotherapy may not be needed as a continuation treatment. While two studies are suggestive that continuation psychotherapy may reduce the relapse rate in those who respond to acute phase psychotherapy, the indications for continuation phase psychotherapy are unclear.
If combined acute phase treatment was used, psychotherapy may be continued, or it may be discontinued if the patient is in remission and psychosocial function has been restored.
Figure
Figure 8. Six-week evaluation: responders to medication.
12. Evaluate the need for maintenance phase treatment
The goal of maintenance treatment is prevention of a recurrence of a major depressive episode. The efficacy of maintenance treatment in preventing a future episode of depression has been clearly demonstrated only with medication. The following principles apply:
Maintenance medication treatment should be considered for selected cases after acute and continuation treatment. Patients who have had three previous episodes of depression should be maintained for one to several years on medication at the same dose that was effective in the acute phase of treatment.
Maintenance medication treatment should be considered for patients with two episodes of major depressive disorder who also have:
First-degree relative with bipolar disorder or recurrent major depression.
History of recurrence within 1 year after previously effective medication was discontinued.
Early onset (before age 20) of the first episode.
Both episodes were severe, sudden, or life-threatening in the past 3-years.
Maintenance psychotherapy can be useful in selected situations with recurrent major depressive disorder, such as women who want to become pregnant and bear a child in a drug-free condition or individuals who must be medication-free for a limited time period. Although maintenance psychotherapy has not been shown to prevent recurrence, one study suggests that it may help to delay the onset of the next episode.
13. Seek consultation
Consult with or referral to a mental health specialist (e.g., psychiatrist, psychologist, psychiatric nurse, social worker) can be useful in the following situations:
The general guidelines cannot be followed or may not be suitable for the individual patient.
The patient fails to respond fully to one or two medication trials.
The patient is actively suicidal.
The patient is suffering very severe psychotic or bipolar depression.
The presence of psychotic features makes hospitalization a consideration.
The patient's symptoms suggest a complex psychiatric or general medical diagnosis.
The patient shows persistent psychosocial problems.
Formal psychotherapy is a consideration.
Specialized treatments, such as electroconvulsive or light therapy, are a consideration.
The patient or clinician wishes a second opinion.
Back Cover
AHCPR invites comments and suggestions from users for consideration in development and updating of guidelines. Please send written comments to Director, Office of the Forum for Quality and Effectiveness in Health Care, AHCPR, Executive Office Center, Suite 401, 2101 East Jefferson Street, Rockville, MD 20852.
This document is in the public domain and may be used and reprinted without special permission, except for those copyrighted materials noted for which further reproduction is prohibited without the specific permission of copyright holders. AHCPR appreciates citations as to source, and the suggested format is as follows:
Depression Guideline Panel. Depression in Primary Care: Detection, Diagnosis, and Treatment.
Quick Reference Guide for Clinicians, Number 5.
Rockville, MD.
U.S. Department of Health and Human Services,
Public Health Service,
Agency for Health Care Policy and Research.
AHCPR Publication No. 93-0552. April 1993. <//DD>
Bibliography
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd rev. ed. Washington, DC: American Psychiatric Press; 1987.
- Depression Guideline Panel. Depression in Primary Care: Volume 1, Diagnosis and Detection. Clinical Practice Guideline, Number 5. Rockville, MD. U.S. Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research. AHCPR Publication No. 93-0550. March 1993.
- Depression Guideline Panel. Depression in Primary Care: Volume 2, Treatment of Major Depression. Clinical Practice Guideline, Number 5. Rockville, MD. U.S. Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research. AHCPR Publication No. 93-0551. March 1993.
- Depression Guideline Panel. Depression in Primary Care: Guideline Report. Rockville, MD. U.S. Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research. Forthcoming.
- Goodwin FK, Jamison KR. Manic-depressive illness. New York: Oxford University Press;1990.
AHCPR Publication No. 93-0552.
National Library of Medicine DOCLINE Information: MED/93251256
-
Depression in Primary Care: Detection, Diagnosis, and Treatment - AHCPR Quick Re...
Depression in Primary Care: Detection, Diagnosis, and Treatment - AHCPR Quick Reference GuidesBookshelf
-
Supportive Therapy in Burn Care - NIH Consensus Statements
Supportive Therapy in Burn Care - NIH Consensus StatementsBookshelf
-
Autologous Peripheral Stem-Cell Transplantation - AHCPR Health Technology Assess...
Autologous Peripheral Stem-Cell Transplantation - AHCPR Health Technology AssessmentsBookshelf
-
Pain Control after Surgery: A Patient's Guide - AHCPR Consumer Guides
Pain Control after Surgery: A Patient's Guide - AHCPR Consumer GuidesBookshelf
-
Adjuvant Chemotherapy for Breast Cancer - NIH Consensus Statements
Adjuvant Chemotherapy for Breast Cancer - NIH Consensus StatementsBookshelf
Your browsing activity is empty.
Activity recording is turned off.
See more...