- Home
- Search for Research Summaries, Reviews, and Reports
EHC Component
- EPC Project
Topic Title
Full Report
- Research Review Apr. 13, 2011
Related Products for this Topic
- Clinician Summary Apr. 13, 2011
- Consumer Summary Apr. 13, 2011
- La Guías Sumaria de los Consumidores Aug. 15, 2011
- Policymaker Summary Nov. 21, 2011
- Executive Summary Apr. 13, 2011
Related Links for this Topic
Original Nomination
Research Protocol – Dec. 9, 2009
Traumatic Brain Injury and Depression – Research Protocol Document
Formats
- View PDF (PDF) 122 kB
- Help with Viewers, Players, and Plug-ins
Table of Contents
- Background and Objectives for the Systematic Review
- The Key Questions
- Analytic Framework
- Methods
- References
- Definition of Terms
- Summary of Protocol Amendments
Background and Objectives for the Systematic Review
Traumatic brain injury (TBI) occurs when external force from events such as falls, assault, motor vehicle accidents or from blasts injures the brain. It may occur as a result of a direct hit to the head, or from rapidly accelerating and decelerating wind accompanied by pressure changes that can injure the brain directly or propel other objects into the head (as from a blast).1 TBI is often accompanied by symptoms that may be severe or mild, and in cases of mild TBI (mTBI), can include nausea, headache, balance problems, blurred vision, memory loss or difficulty concentrating.2
TBIs are associated with a range of short- and long-term sequelae, including physical, cognitive, behavioral and emotional outcomes.3 Symptoms of depression appear common in individuals who have sustained a TBI, with estimates of post-TBI depression ranging from 15% to 77% in the published literature.4-6 Depression associated with TBI can manifest shortly after injury or well into the future,7, 8 and rates reported are likely affected by timing of screening and tools used to do so.
In their review of TBI rehabilitation, in which they selected studies from MEDLINE, CINAHL, and PsycINfo, Gordon et al. identified a total of 74 studies addressing psychiatric functioning after a TBI.9 Their assessment was that TBI is associated with high rates of depression (up to more than half of cases) and of other axis I and axis II conditions, including paranoid, schizoid and avoidant personality. Furthermore, depression was noted to be comorbid with other psychiatric conditions, including addiction or anxiety, in a number of studies.
Depression that does occur post-injury may be related to neuroanatomic or pathophysiological changes (i.e., brain lesions and specific location of lesions) or to situational concerns about disability or poor functional status.7, 10 It seems likely that the etiology of the depression could affect the potential effectiveness of treatment strategies with, for example, situational depression more conducive to psychotherapy.
Whether the etiology of the depression is neurobiological or situational may also affect the time of onset; earlier onset depression may be more likely to have a neuroanatomic source, while later onset may be associated with a realization of the level of impairment and low likelihood of substantial improvement. This also raises issues for timing screening for depression as earlier screening may be likely to capture depression with a pathophysiological etiology than later screening – and conversely, may miss later depression that is situational or associated with plateaus in improvement.
The Key Questions
The Preliminary Key Questions serve as a starting point for Key Informant discussions and aid in the development of Draft Key Questions. Key Informants use these questions to ensure that the proposed topic represents an important decisional dilemma in health care. Based on their review, Key Informants also critique how well the correct patients, interventions, comparators, outcomes, and other factors have been identified. During the topic refinement process the Vanderbilt EPC created a list of 22 questions that could potentially be answered in a comparative effectiveness review. The EPC with the guidance from the Technical Expert Group (TEG) narrowed the list of questions to the most informative and important questions, seven in total. The intent of this exercise is to assess the state of the literature regarding this topic and to formulate appropriate key-questions for a subsequent CER During interactions with content experts and the AHRQ Task Order Officer, one question was eliminated due to the low yield of information likely to result. The remaining key questions are listed below.
- Does the area of the brain injured, the severity of the injury, the mechanism or context of injury, or time to recognition of the traumatic brain injury or other patient factors influence the probability of developing incident clinical depression?
- When should patients who suffer traumatic brain injury be screened for depression, with what tools and in what setting?
- Among individuals with TBI and depression, what is the prevalence of concomitant psychiatric/behavioral conditions, including anxiety disorders, PTSD, substance abuse and major psychiatric disorders?
- What are the outcomes (short and long term, including harm) of treatment for depression amongst traumatic brain injury patients utilizing: a) psychotropic medications, b) individual/group psychotherapy, c) neuropsychological rehabilitation, d) community-based rehabilitation, e) CAM, f) neuromodulation therapies and g) other?
- Where head-to-head comparisons are available, which treatment modalities are equivalent or superior with respect to benefits, short- and long-term risks, quality of life, or costs of care?
- Are the short- and long-term outcomes of treatment for depression after TBI modified by individual characteristics, such as age, pre-existing mental health status or medical conditions, functional status, and social support?
| Population |
|
|---|---|
| Interventions |
|
| Comparators |
|
| Outcomes |
|
| Timing |
|
| Settings |
|
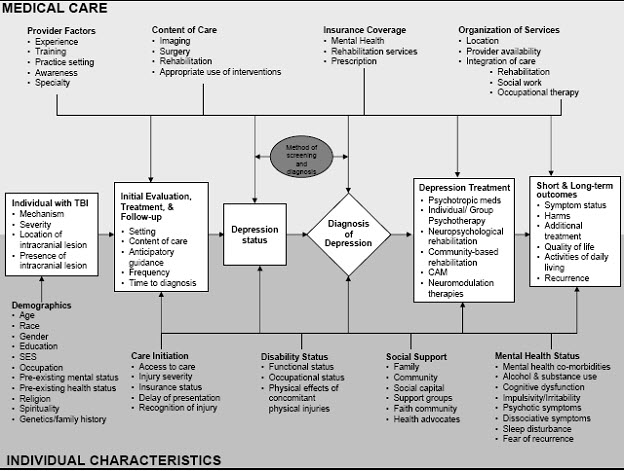
Analytic Framework
Provide an analytic framework to illustrate the population, interventions, outcomes, and adverse effects that will guide the literature search and synthesis.
Methods
We will systematically search, review, and analyze the scientific evidence for each key question and any subsidiary questions. In doing so, we will look for variations in reported results for mechanism and location of injury as well as context in which the injury was received. The steps that we are taking to accomplish the literature review are described below.
A. Criteria for Inclusion/Exclusion of Studies in the Review
| Category | Criteria | |
|---|---|---|
| Study population | Adults aged ≥18 years old | |
| Study settings and geography | Developed nations: United States, Canada, United Kingdom, Western Europe, Japan, Australia, New Zealand, Israel, South America | |
| Publication languages | English only | |
| Admissible evidence (study design and other criteria) | Admissible designs | Randomized controlled trials, cohorts with comparison, case-control, and case series (n ≥ 50) |
| Other criteria |
|
|
Inclusion and exclusion criteria based on study size have yet to be determined. The EPC will record the study size of any study that would be excluded only because it has less than 50 participants. The EPC will then set a study size cut-off based on the number of key or sentinel papers that would be excluded.
B. Searching for the Evidence: Literature Search Strategies for Identification of Relevant Studies to Answer the Key Questions
Search Literature. We will begin with a search on topic that include various entries including but not limited to “traumatic brain injury”, “head injury” “depressive disorder”, and “depression”. We will initial search MEDLINE©, but given the complexity of the topic expand our search to include the following databases, PsycINFO, EMBASE, CINAHL, and PILOTS. The various search strategies used each database are included below.
| Search # | Terms |
|---|---|
| #1 | (Brain Concussion[mh] OR brain injuries[mh:noexp] OR Brain Hemorrhage, Traumatic[mh] OR Epilepsy, Post-Traumatic[mh] OR Head Injuries, Closed[mh] OR Head Injuries, Penetrating[mh] OR Intracranial Hemorrhage, Traumatic[mh] OR Craniocerebral Trauma[mh] OR TBI[tiab] OR head injuries[tiab] OR head injury[tiab] OR traumatic brain injury[tiab] OR traumatic brain injuries[tiab] OR neurotrauma[tiab] OR diffuse axonal injury[mh] OR diffuse axonal injury[tiab] OR Contrecoup contusion[tiab] OR brain trauma[tiab] OR head trauma[tiab]) |
| #2 | Depressive Disorder[mh] OR Depression[mh] OR depressive[tiab] OR depression[tiab] OR depressed[tiab] OR sadness[tiab] OR sad[tiab] OR hopelessness[tiab] OR suicidal[tiab] OR suicide[tiab] OR Mental Disorders[mh:noexp] OR mood[tiab] |
| #3 | #1 AND #2 AND eng[la] AND humans[mh] |
| #4 | #3 AND case reports[pt] |
| #5 | #3 AND letter[pt] |
| #6 | #3 AND comment[pt] |
| #7 | #3 AND editorial[pt] |
| #8 | #3 AND practice guideline[pt] |
| #9 | #3 AND news[pt] |
| #10 | #3 AND review[pt] |
| #11 | #3 NOT (#4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10) |
| Search # | Terms |
|---|---|
| #1 | DE=("head injuries" or "brain concussion" or "traumatic brain injury") or KW=("head injury" or "head injuries" or "traumatic brain injury" or "traumatic brain injuries" OR "craniocerebral trauma" or neurotrauma or "brain trauma" OR "head trauma" OR TBI) |
| #2 | DE=("depression emotion" or "major depression" or "hopelessness" or "sadness" or "suicidal ideation" or "suicide") or KW=(depressive or sad or hopeless or sadness) |
| #3 | #1 AND #2 AND LA=(English) AND PO=(Human) |
| #4 | #3 AND PT=(letter) |
| #5 | #3 AND PT=(comment/reply) |
| #6 | #3 AND PT=(editorial) |
| #10 | #3 NOT (#4 OR #5 OR #6) |
| Search # | Terms |
|---|---|
| #1 | head injury/ or brain concussion/ or brain contusion/ or diffuse axonal injury/ or postconcussion syndrome/ or traumatic brain injury/ or ("craniocerebral trauma" or "brain trauma" or "head trauma" or TBI or "traumatic brain injury" or "traumatic head injury" or "traumatic brain injuries" or "traumatic head injuries").ab. or ("craniocerebral trauma" or "brain trauma" or "head trauma" or TBI or "traumatic brain injury" or "traumatic head injury" or "traumatic brain injuries" or "traumatic head injuries").ti. |
| #2 | mental disease/ or mood disorder/ or depression/ or major depression/ or suicidal ideation/ or hopelessness/ or (depressive or sad or sadness or hopeless).ti. or (depressive or sad or sadness or hopeless).ab. |
| #3 | #1 and #2 and english.lg. and human/ |
| #4 | #3 and conference paper.pt. |
| #5 | #3 and editorial.pt. |
| #6 | #3 and letter.pt. |
| #7 | #3 and note.pt. |
| #8 | #3 and review.pt. |
| #9 | #3 and short survey.pt. |
| #10 | #3 not (#4 or #5 or #6 or #7 or #8 or #9) |
| Search # | Terms |
|---|---|
| #1 | ("traumatic brain injury") or (MH "Brain Injuries+") OR "neurotrauma" OR "brain injuries" OR "TBI" OR "concussion" OR "head injuries" OR "head injury" OR "head trauma" OR "brain trauma" |
| #2 | ((MH "Depression+") OR "depressive disorder" OR "sadness" OR "depressed" OR (MH "Suicide") or (MH "Suicide, Attempted") or (MH "Suicidal Ideation") OR "suicide" OR "hopelessness" or (MH "Hopelessness") OR "mood") |
| #3 | #1 AND #2 |
| #4 | #3 AND Exclude MEDLINE Records |
| #5 | #4 AND Limit to English Language; Publication Type: Clinical Trial, Proceedings, Research, Systematic Review |
| Search # | Terms |
|---|---|
| #1 | (DE="head injuries") or("brain concussion" OR concussion OR "traumatic brain injury" OR "TBI" OR neurotrauma OR "traumatic brain injuries" OR "head trauma" OR "craniocerebral trauma" OR "brain injury" OR "brain injuries" ) |
| #2 | (DE="depressive disorders") or(depression OR depressed OR depressive OR suicidal OR suicide OR sadness OR hopelessness) |
| #3 | #1 AND #2 |
| #3 | #3 AND English Only AND Journal Articles Only |
| #4 | #3 AND Peer-Reviewed Journals subset* |
Review Abstracts. We will review our preliminary inclusion/exclusion criteria, below, during the initial conference call and again during the first conference call with the TEP; revise the criteria, as appropriate, based on the input from the calls. The revisions are subject to constraints of the existing scope of work (time and budget).
We will review all titles and abstracts identified through new searches against our inclusion/exclusion criteria. Each abstract is being reviewed by the Scientific Director, Content Lead, Content Experts, Associate Director, Library Scientists, and/or Project Manager. When differences between the reviewers arise, we err on the side of inclusion. For studies without adequate information to make the determination, we are retrieving the full articles and are reviewing them against the inclusion/exclusion criteria.
C. Data Abstraction and Data Management
Develop Data Collection Forms. We will develop data collection forms that include questions on identifying information for the article, study design, methods, and results. After reviewing a sample of relevant articles, the team will design the data collection form and test it on multiple articles before initiating data abstraction. We expect that the data collection form will undergo several revisions based upon these tests.
Retrieve and Review Articles. We will retrieve and review all articles meeting our predetermined inclusion/exclusion criteria or for which we have insufficient information to make a determination. The abstractor(s), the Scientific Director, and the Content Leads will reassess each retained article against the inclusion/exclusion. For the studies meeting the second-round assessment, the abstractors will extract key data elements from the article(s) and enter them into the abstraction form. The Project Manager will review abstraction forms against the original articles for quality control. Differences between the abstractor and the Project Manager will be resolved by consensus.
We have developed a simple categorization scheme for coding the reasons that articles, at the stage of full review, are not finally included in the report. The abstractor notes the reason for exclusion on the article cover page. We then record that code in EndNote®, our bibliography software, so that we can later compile a listing of excluded articles and the reasons for such exclusions.
D. Assessment of Methodological Quality of Individual Studies
Assess Quality of Articles. For this quality rating step, we expect to adapt one of the types of grading schemes noted as “best practices” in the EPC’s review of systems to rate evidence. Two senior staff will separately assign quality grades; in our experience quality grading is conducted most efficiently and consistently by senior staff. We will record quality grades in the evidence tables.
E. Data Synthesis
Prepare Evidence Tables. We will enter data from the data abstraction forms into evidence tables, using predetermined abbreviations and acronyms and otherwise attending to consistency across entries from the outset. The dimensions (i.e., areas of special focus, or the columns) of each evidence table will vary by key question, but the tables will contain some common elements, such as author, year of publication, study location (e.g., country, city, state) and time period, population description, sample size, and study type (e.g., randomized controlled trial, prospective observational study, etc). Among other data, we will include any information on prevalence and variation in practice.
F. Grading the Evidence for Each Key Question
We will develop explicit criteria for rating the overall strength of the collective evidence on each key question into qualitative categories (e.g., good, fair, poor). In so doing, we will use established concepts of the quantity of evidence (e.g., numbers of studies, aggregate ending sample sizes), the quality of evidence (from the quality ratings on individual articles), and the coherence or consistency of findings across similar and dissimilar studies and in comparison to known or theoretically sound ideas of clinical or behavioral knowledge. We will make these judgments for each of the main key questions and any subquestions, if appropriate.
References
- Okie S. Traumatic brain injury in the war zone. N Engl J Med. 2005 May 19;352(20):2043-7.
- Defense and Veterans Brain Injury Center Working Group on the Acute Management of Mild Traumatic Brain Injury in Military Operational Settings. Clinical Practice Guideline and Recommendations, December 22, 2006. 2006.
- Rehabilitation of persons with traumatic brain injury. NIH Consens Statement. 1998 Oct 26-28;16(1):1-41.
- Kim E, Lauterbach EC, Reeve A, et al. Neuropsychiatric complications of traumatic brain injury: a critical review of the literature (a report by the ANPA Committee on Research). J Neuropsychiatry Clin Neurosci. 2007 Spring;19(2):106-27.
- O'Donnell ML, Creamer M, Pattison P, et al. Psychiatric morbidity following injury. Am J Psychiatry. 2004 Mar;161(3):507-14.
- Varney NR, Martzke JS and Roberts RJ. Major depression in patients with closed head injury. Neuropsychology. 1987;1:7-9.
- Jorge RE, Robinson RG, Starkstein SE, et al. Depression and anxiety following traumatic brain injury. J Neuropsychiatry Clin Neurosci. 1993 Fall;5(4):369-74.
- Holsinger T, Steffens DC, Phillips C, et al. Head injury in early adulthood and the lifetime risk of depression. Arch Gen Psychiatry. 2002 Jan;59(1):17-22.
- Gordon WA, Zafonte R, Cicerone K, et al. Traumatic brain injury rehabilitation: state of the science. Am J Phys Med Rehabil. 2006 Apr;85(4):343-82.
- Busch CR and Alpern HP. Depression after mild traumatic brain injury: a review of current research. Neuropsychol Rev. 1998 Jun;8(2):95-108.
Definition of Terms
Not applicable.
Summary of Protocol Amendments
In the event of protocol amendments, the date of each amendment will be accompanied by a description of the change and the rationale.
NOTE: The following protocol elements are standard procedures for all protocols.
- Review of Key Questions
For Comparative Effectiveness reviews (CERs) the key questions were posted for public comment and finalized after review of the comments. For other systematic reviews,
key questions submitted by partners are reviewed and refined as needed by the EPC and the Technical Expert Panel (TEP) to assure that the questions are specific and explicit about what information is being reviewed. - Technical Expert Panel (TEP)
A TEP panel is selected to provide broad expertise and perspectives specific to the topic under development. Divergent and conflicted opinions are common and perceived as health scientific discourse that results in a thoughtful, relevant systematic review. Therefore study questions, design and/or methodological approaches do not necessarily represent the views of individual technical and content experts. The TEP provides information to the EPC to identify literature search strategies, review the draft report and recommend approaches to specific issues as requested by the EPC. The TEP does not do analysis of any kind nor contribute to the writing of the report. - Peer Review
Approximately five experts in the field will be asked to peer review the draft report and provide comments. The peer reviewer may represent stakeholder groups such as professional or advocacy organizations with knowledge of the topic. On some specific reports such as reports requested by the Office of Medical Applications of Research, National Institutes of Health there may be other rules that apply regarding participation in the peer review process. Peer review comments on the preliminary draft of the report are considered by the EPC in preparation of the final draft of the report. The synthesis of the scientific literature presented in the final report does not necessarily represent the views of individual reviewers. The dispositions of the peer review comments are documented and will, for CERs and Technical briefs, be published three months after the publication of the Evidence report.
It is our policy not to release the names of the Peer reviewers or TEP panel members until the report is published so that they can maintain their objectivity during the review process.
 E-mail Updates
E-mail Updates
