Studies Uncover Associations between Human Papillomavirus and Oral Cancer
Posted By Linda Perrett On October 18, 2010 @ 1:42 pm In HPV,Oral Cancer,cancer | Comments Disabled
NCI-supported research is contributing to the understanding of how the human papillomavirus (HPV) causes oral cancer. These research efforts are identifying factors and behaviors that may put some people at high risk for the disease.
While oral cancer caused by tobacco use has declined over the past 30 years, oral cancers associated with HPV have skyrocketed. In fact, about 70 percent of all newly diagnosed cases of oral cancer are attributable to HPV infection, usually by sexual activity—the same factor responsible for the majority of cervical cancer cases in women.
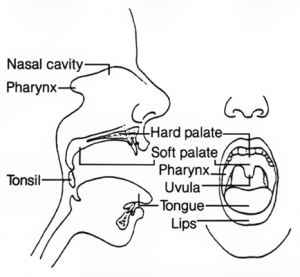
HPV has many different strains, or types. HPV 6 and 11 cause genital warts. HPV 16 and 18 are high-risk types that cause cervical, anal-genital, and oropharyngeal cancer, also called head and neck cancer or oral cancer. Oropharyngeal cancer forms in tissues of the oropharynx, the part of the throat at the back of the mouth that includes the soft palate, the base of the tongue, and the tonsils. Most oropharyngeal cancers are classified as squamous cell carcinomas that begin in flat cells that line the oropharynx.
Unraveling HPV’s Role in Oral Cancer
NCI-supported investigator, Maura Gillison, M.D., Ph.D., is a professor of internal medicine and epidemiology at the Ohio State University Comprehensive Cancer Center. Prior to joining OSUCCC, she was an associate professor at Johns Hopkins Medical Institutions.
Gillison heads a laboratory at OSUCCC where scientists harness the power of molecular biology and epidemiology to study HPV viruses that cause oral cancers. Factors identified in her laboratory are then often tested in humans. Her studies were the first to:
- Uncover the link between HPV and oral cancer and that men were at high risk for disease;
- Find that HPV-positive and HPV-negative head and neck cancers are caused by distinct sets of risk factors and are thus two different diseases; and
- Show that patients with HPV-positive head and neck cancer have better survival rates than those with HPV-negative cancer.
HPV Causes Oral Cancer—Men at Highest Risk of Disease
Gillison led a study that provided compelling evidence that HPV causes oral cancer and identified that men who had multiple sex partners were at high risk for disease. This study was chosen by the American Society of Clinical Oncology as one of the six major clinical cancer advances of 2007.
The study consisted of 100 patients, all with newly diagnosed oropharyngeal squamous cell carcinoma, and 200 people without a history of cancer. Oral-mucosal and blood serum samples were collected from all of the study participants and tumor samples were collected from the cancer patients. Samples for all of the study participants were analyzed for the presence of HPV DNA or antibodies that would indicate prior exposure to HPV-16. Data on risk factors (i.e. sexual habits, alcohol consumption, etc.) were collected from all participants.
The scientists found that past exposure to HPV-16, as measured by presence of antibodies to the virus in serum samples, was strongly associated with oropharyngeal cancer. They also discovered that antibodies against HPV-16 were found in 64 percent of patients but only four percent of people without cancer.
Data collected on risk factors verified that HPV-16 caused oropharynx cancer in people, whether or not they smoked tobacco or drank alcohol. Evidence linked its development to prior exposure to HPV-16 and a high lifetime number of vaginal-sex partners (26 or more) or oral-sex partners (six or more), and reported that men were at high risk for disease.
“The finding that men were at high risk of HPV-16 related oropharyngeal cancer ignited the debate over vaccinating young boys and men against HPV using Gardasil, a HPV-vaccine already used to protect girls and women against cervical cancer,” said Gillison. In 2009, a FDA advisory panel voted to recommend the expanded use of the Gardasil for males age nine to 26 for the prevention of genital warts caused by HPV 6 and 11; an added benefit may be protection against certain anal-genital and oropharyngeal cancers.
The 2007 study was published in the New England Journal of Medicine.
PV-Positive and HPV-Negative Head and Neck Cancers May be Two Distinct Diseases
Patients with HPV-16-positive head and neck squamous cell carcinoma (HNSCCS) have different risk factors than those with HPV 16-negative HNSCCS, indicating that they should be considered as two distinct diseases, according to a study led by Gillison.
In this study, 240 patients were diagnosed with HNSCCS at Johns Hopkins Hospital, Baltimore, Md., and their status—either HPV-16-positive or HPV-16-negative—was identified. Next, scientists matched two cancer-free control subjects, by age and sex, to each one of the patients. Data on risk factors (i.e. sexual habits, alcohol consumption, etc.) were collected from all participants.
Gillison and her colleagues reported that HPV-16-positive HNSCCS was found in 92 of 240 patients. HPV-16 positive HNSCC was associated with sexual behavior and exposure to marijuana but not with tobacco smoking, alcohol drinking, or poor oral hygiene. By contrast, HPV-16-negative HNSCCS was associated with tobacco smoking, alcohol drinking, and poor oral hygiene, but not with any measure of sexual behavior or marijuana use. The investigators had included measures of marijuana use in their survey because of inconsistent associations between its use and development of head and neck cancer in prior studies.
“To me, this is my most important work,” said Gillison. “Explaining the underlying diverse nature of head and neck cancer is the key to improved prevention and treatment for cancer patients.”
The 2008 study was published in the Journal of the National Cancer Institute.
PV-Positive Head and Neck Cancer Patients Have Higher Survival Rates Than Those with HPV-Negative Disease
 [3]The status of a HPV tumor is a strong and independent prognostic factor for survival among patients with oropharyngeal cancer. Patients with HPV-16 positive HNSCC have better overall survival rates than those with HPV-16-negative disease, according to findings from a multi-group, international study lead by Gillison.
[3]The status of a HPV tumor is a strong and independent prognostic factor for survival among patients with oropharyngeal cancer. Patients with HPV-16 positive HNSCC have better overall survival rates than those with HPV-16-negative disease, according to findings from a multi-group, international study lead by Gillison.
In a phase III trial conducted by the Radiation Therapy Oncology Group (RTOG), a clinical cooperative group funded primarily by NCI grants, investigators studied survival rates of 323 patients with stage III or IV oropharyngeal cancer. Of the study participants, 206 patients had HPV-16-positive HNSCC and 117 had HPV-16-negative HNSCC. All patients were treated with a combination of radiation therapy and chemotherapy.
After three years, the survival rate for patients with HPV-16-positive HNSCC was 82.4 percent, compared to 57.1 percent for patients HPV-16-negative HNSCC. Progression-free survival (refers to patients who still have cancer, but their cancer is not progressing) for patients with HPV-16-positive HNSCC was 73.7 percent, compared to 43.4 percent for patients with HPV-16-negative HNSCC. After factoring in common determinants for survival, such as patient age, race, and tumor stage, the investigators found that HPV-16-positive HNSCC patients had a 58 percent reduction in risk of death, compared to the patients with HPV-16-negative HNSCC.
“NCI support of the cooperative groups, such as the RTOG, has been essential in determining the optimal therapy for patients with HPV-positive head and neck cancer,” said Gillison. “As a result of this study, both the RTOG, as well as the Eastern Cooperative Oncology Group, have designed clinical trials specifically for patients with HPV-positive head and neck cancer.”
The 2010 study was published in the New England Journal of Medicine.
For more information about HPV transmission, watch our animation on HPV Infection and Transformation [4]
Article printed from NCI Benchmarks: http://benchmarks.cancer.gov
URL to article: http://benchmarks.cancer.gov/2010/10/studies-uncover-associations-between-human-papillomavirus-and-oral-cancer/
URLs in this post:
[1] Image: http://benchmarks.cancer.gov/2010/10/studies-uncover-associations-between-human-papillomavirus-and-oral-cancer/benchmarksoctthumb-2/
[2] Image: http://benchmarks.cancer.gov/2010/10/studies-uncover-associations-between-human-papillomavirus-and-oral-cancer/gillison-2/
[3] Image: http://benchmarks.cancer.gov/2010/10/studies-uncover-associations-between-human-papillomavirus-and-oral-cancer/drawing-of-mouth-3/
[4] HPV Infection and Transformation: http://benchmarks.cancer.gov/2010/10/hpv-infection-and-transformation-animation/
Click here to print.