Virtual Colonoscopy
To commemorate March as National Colon Cancer Prevention month, this edition of BenchMarks focuses on potential new screening methodologies for the early detection of colorectal cancers. An interview with Ernest Hawk, M.D., chief of Gastrointestinal and Other Cancers Research Group at the National Cancer Institute (NCI), covers colorectal cancer screening tools and compares and contrasts colonoscopy (or optical colonoscopy) with virtual colonoscopy.
Colorectal cancer is the second leading cancer killer in the United States. It is estimated that 146,940 people in this country will be diagnosed with colorectal cancer and 56,730 people will die of the disease. Experts believe that over 90% of all colorectal cancers can be cured through early detection and treatment.
Who should be screened for colorectal cancer and how often?
Currently, it’s recommended that Americans 50 years and older should be screened for colorectal cancer. If there’s a tendency towards colon cancer in the family, as evidenced by a close relative with either adenomas or cancer, it’s advised to start 10 years earlier and to use a more sensitive and specific technique. But for the general population, it’s 50 years and older.
How many people over the age of 50 actually get screened by the current processes?
The unfortunate thing is colorectal cancer should largely be a preventable illness, but in the United States at the moment only 30 to 40 percent of people who should be screened have actually been screened. That leaves us a lot of ground to make up.
It seems clear, then, that there is a pressing need for additional screening technologies. What are the available screening methods for detection of colon cancer?
While there is always room for technological improvements, we need to do a better job of using the current screening technologies. Because, despite their limitations, they have been proven effective in reducing the burden of disease. There are five regimens that are currently recommended, providing practitioners and patients with a menu of screening options. They include annual fecal occult blood testing (FOBT) – that is, looking for blood in the stool; flexible sigmoidoscopy every five years; colonoscopy every 10 years; air-contrast barium enema every five years; and a combination of FOBT with flexible sigmoidoscopy, each at their usual intervals.
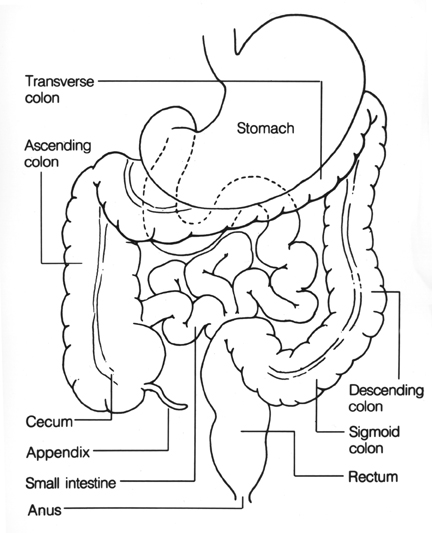
Each of these tests have various advantages and disadvantages; for example, they vary in sensitivity and specificity — that is, how well they detect colon cancer or polyps when they’re present and reassure us when they’re absent. Colon cancer is the end-result of a prolonged process during which changes in genes in the cells lining the intestine accumulate, resulting in abnormal growths called polyps. If polyps accumulate additional genetic changes, a fraction of them may become cancerous. We tend to worry about polyps becoming cancerous as they grow; for example, polyps greater than one centimeter in diameter are usually removed because they present a high cancer risk.
What prevents people from going in to get screened?
There are a wide variety of reasons why people aren’t screened. A lot of it has to do with whether they recognize that they should be screened. Do they know the current screening guidelines? If not, has colorectal cancer screening been recommended to them by their health care provider? Unfortunately, some recent surveys suggest that colorectal cancer screening is not routinely recommended by health care providers, despite evidence of its benefit. After overcoming that challenge, other issues like convenience, cost, availability, and embarrassment represent significant barriers for some patients. Fortunately, colon cancer screening – even colonoscopy – is now paid for by Medicare, so cost is not as big a barrier as it has been in the past.
What is it about optical colonoscopy that is considered the “gold standard” for colorectal cancer screening?
Colonoscopy is considered the gold standard for colorectal cancer screening by some groups but not by others. The American College of Gastroentology recommends colonoscopy as a preferred approach to colorectal screening. By contrast, the Centers for Disease Control and Prevention recommend colonoscopy as one of the five acceptable colorectal cancer screening options outlined above. However, optical colonoscopy is considered the gold standard by some professionals because it allows complete and direct visualization of the entire colon, thereby providing the opportunity to identify precancerous polyps and cancer, and then to do diagnostic biopsies or therapeutic removal of these lesions, all in one setting.
What is virtual colonoscopy?
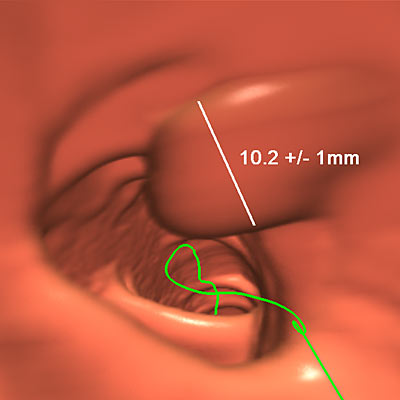
Virtual colonoscopy is a new technique that uses X-rays delivered through a CT scanner to take cross-sectional views through the abdomen, and then reconstruct those views in a special way using computer software. The result is a set of images that provide a radiologist with essentially the same sort of view of the colon as a gastroenterologist would have by doing an optical colonoscopy with a tube inserted into the colon. The advantages really have to do with the fact that the technique is relatively quick, fairly sensitive, and only minimally invasive.
How is a virtual colonoscopy performed?
A patient undergoes a routine bowel preparation at home the night before the exam by taking laxatives to purge the colon of waste matter. Then, on the day of the exam, a small amount of air is introduced into the colon via the rectum. The introduction of air is the only invasive component of the exam. The exam itself consists of lying on a table to have a series of very fast X-rays taken. It only takes a few minutes to complete, as opposed to optical colonoscopy, which can take a half hour or more. The big drawback at the moment is that virtual colonoscopy is not widely available and not yet definitively tested.
What are the benefits of a virtual colonoscopy over an optical colonoscopy?
The speed, relatively low level of invasiveness, and potential for broad availability are virtual colonoscopy’s major advantages at the moment.
A virtual colonoscopy only takes on the order of a few minutes to actually do the exam, and probably 15 minutes to 30 minutes more to read the exam.
Why does an optical colonoscopy take so much longer?
Optical colonoscopy takes a longer period of time because the procedure itself takes more time than a virtual colonoscopy exam and because sedatives are used — medicines to dull the patient’s senses so that they’re not fully aware of what’s going on. So, the exam usually takes a half hour or so and then there’s the additional time to administer and recover from the sedatives. Finally, it is important to have someone available to drive the patient home because the effects of the sedative can last a couple of hours. Virtual colonoscopy gets around some of these aspects of convenience and cost.
What are the disadvantages of a virtual colonoscopy compared to an optical colonoscopy?
The biggest limitation of virtual colonoscopy at the moment is that patients still need to go through the same bowel preparatory regime; patients really don’t like that. In addition, there is still the need for some instrumentation to put air into the colon. Other big drawbacks at the moment are its limited availability and lack of definitive testing or validation. These are the key issues holding virtual colonoscopy back from being widely appreciated and implemented.
What is your opinion on studies demonstrating the effectiveness of virtual colonoscopy?
There have been three or four large trials conducted over the past five years comparing virtual colonoscopy to optical colonoscopy. The key comparisons involve the testing of relative sensitivity – that is, determining whether virtual colonoscopy is as good as optical colonoscopy is at identifying adenomatous polyps or cancers. The first two or three of those studies showed virtual colonoscopy had significant limitations, in that it was not able to identify polyps — in particular smaller polyps — as reliably as optical colonoscopy.
However, there was a major report published by Dr. Perry Pickard and colleagues in the Dec. 4, 2003, issue of the New England Journal of Medicine. That study reported that virtual colonoscopy was quite comparable to optical colonoscopy in terms of the lesions it could identify. The study stimulated new interest in the technique among researchers and, to some extent, among the public at large.
Of course, that was only one study. Typically in medicine, we like to have a couple of studies to confirm a result before we really believe it. At the moment, additional work is needed to validate these findings and to see if the very promising sensitivity and specificity of virtual colonoscopy in that particular study will hold when the technique is applied in the broader medical community.
What else needs to happen in order for this technique to be ready for widespread patient usage?
What really needs to happen at this point is for the New England Journal of Medicine study to be re-evaluated in a much broader study. That study, conducted in Bethesda, was unique in several ways. First of all, it was one of the first times we looked at a true screening population – that is, in patients at average risk for colorectal cancer. Most prior studies had looked at a different population of patients – those with prior adenomas or cancers. This is important because the results in one group may not reflect those seen in another. In addition, Dr. Pickard’s study involved only three centers and used state-of-the-art techniques — they had multi-detector scanners, which improve the sensitivity of this technology; they used a stool and fecal water tagging procedure (to aid the physician in correctly identifying polyps) that hadn’t been done in the same way previously; they used software to reconstruct images in a specific way, which hadn’t been used previously. And finally, they used a limited number of radiologists who had been specifically trained in the virtual colonoscopy technique. For these four reasons, the study was quite unique. Now this finding needs to be replicated more broadly in more centers across the country to see if these excellent results hold up or not.
How long do you think this validation process could take?
There are a couple of studies being proposed to try to validate and build on the results from Dr. Pickard’s group. I’m aware of one study in particular, proposed by a national network of NCI-funded radiologists, that we’re hoping to see initiated within the next year. We anticipate that it would take a couple years for results from these trials, so I would say we may be three years or so away from having the best evidence to say whether this screening technique will provide a compelling new option.
In your opinion, do you think virtual colonoscopy will ever render optical colonoscopy obsolete?
I guess the answer to that question depends on what aspects of virtual colonoscopy and optical colonoscopy you’re asking about. If you’re talking about virtual colonoscopy versus optical colonoscopy for first-line colorectal cancer screening, I would say that, yes, virtual colonoscopy may very well supplant much of the screening currently done by optical colonoscopy. But even if that occurs, it will never make optical colonoscopy obsolete, per se, because there will probably always be patients that prefer the “one-stop shopping” approach offered by optical colonoscopy. That is, the opportunities to screen, diagnose, and treat colorectal polyps and small cancers in one procedure. In addition, it cannot replace the usefulness of optical colonoscopy for subsequent diagnosis and treatment. Indeed, virtual colonoscopy is probably most efficient and acceptable to patients when it is accompanied by the “real-time” availability of subsequent optical colonoscopy for those with a lesion. Without that sort of immediate access to optical colonoscopy, patients with lesions would have to go through another preparative regimen and colonoscopic exam at a later date, thus diminishing whatever convenience and cost advantage virtual colonoscopy may offer.
In any case, there’s a lot more work that needs to be done before we have good data to answer that question with more than speculation.
What other new colorectal cancer screening technologies are being investigated?
There are several attempts to improve upon old technologies, like ways to improve the sensitivity of assays that identify blood in the stool – improved fecal occult blood tests.
But perhaps the most promising new strategy is the one that’s designed to identify mutations or signatures of colon cancer in stool specimens. This procedure is called an MTAP, or multi-targeted assay panel. There are a few different groups working on it, and one major company has invested in it. The idea is to screen not for blood in the colon, which can be derived from cancers or other lesions, but rather to screen more specifically for the molecular determinants of cancer – that is, their molecular “signatures” in the stool. It’s been shown to be highly sensitive for identifying large polyps and cancer in the colorectum (that is, lesions one centimeter and larger) in preliminary studies, but the definitive phase III trials are ongoing now. It’ll be several years yet until we know whether it’s really going to be effective or not.
Animation/Video
Dr. Ernest Hawk of the National Cancer Institute’s Cancer Prevention Division describes the tests that are used to detect colon cancer beginning at age 50.
View Video Clip on NIHSeniorHealth.gov
The following clip is a ‘virtual’ tour of the colon. The left side of the screen is an exterior representation of the colon and the right side of the screen is a tour of the inside of the colon.
| This movie requires the QuickTime plug-in. If you do not have the plugin, please click here to install. | |
Text Transcript
The following clip is a ‘virtual’ tour of the colon. The left side of the screen is an exterior representation of the colon and the right side of the screen is a tour of the inside of the colon.
The image presented is a computer generated ‘virtual’ tour of the colon and rectum. It starts at the rectum and descends through the colon, winding through reddish tissue in a twisting tour of the tunnel that comprises the colon, passing polyps and other growths that could be cause for further evaluation.
Audio Clips
- Dr. Ernest Hawk of the National Cancer Institute’s Cancer Prevention Division describes the tests that are used to detect colon cancer beginning at age 50.
( Audio – Length: 3:14 )
Text Transcript
Dr. Ernest Hawk of the National Cancer Institute’s Cancer Prevention Division describes the tests that are used to detect colon cancer beginning at age 50.
Narrator: Most cancers in their early, most treatable stages don’t exhibit any symptoms. Colon cancer might be prevented if polyps that lead to the cancer are detected and removed.
Dr. Ernest Hawk of the National Cancer Institute’s Cancer Prevention Division describes the tests that are used to detect colon cancer beginning at age 50.
Dr. Ernest Hawk: The first of them is probably the most well-proven and that’s fecal occult blood testing, or looking for blood in the stool. Both polyps, as well as cancers, can bleed and you can identify that by doing a special test that’s done at home. The results are given to your physician and we know that the use of that test can result in about a 30% reduction in colon cancer deaths. So that test is relatively convenient — that is, it doesn’t require any special procedures — but some people are not particularly attracted to the methods that are involved.
Narrator: Another test is a flexible sigmoidoscopy which is an examination of the rectum and lower colon using a lighted instrument.
Dr. Ernest Hawk: And they look at the last part of the colon. Can go in about 50 centimeters — about a couple of feet — and look at the lining, look for polyps, as well as cancer. That’s another very effective method. So it requires going into a doctor’s office, doesn’t require any sort of anesthesia, but it takes 15 minutes or so.
The third option is a barium enema. That’s an x-ray examination of the colon where you go into a hospital, typically, have an enema to clear out the colon. Subsequently, a radiologist takes you into the x-ray room, puts a dye into the colon and then takes x-ray pictures. That, again, takes half an hour or so. It has slightly less sensitivity — it can’t find polyps quite as well as some of the other tests — but it’s perfectly acceptable, as well as one of the several methods.
And lastly, there’s colonoscopy where a physician takes a lighted tube and looks at the entire lining of the colon, several feet long. That procedure typically requires some amount of anesthesia so a doctor gives you medicine — makes you a little bit drowsy. It takes about 15 minutes to half an hour. And that procedure — its benefits really are that it can both identify cancers and polyps, but also treat those that are not complicated. So if a small, pre-cancerous growth polyp is identified, it can be removed in the same setting.
Narrator: Dr. Hawk says whatever test you and your doctor determine is right for you — fecal occult blood test, sigmoidoscopy, barium enema, colonoscopy, or a combination of some of these — if you are 50 or over, the important thing is to get tested.
Dr. Ernest Hawk: I think the big message is that people need to be screened. For any one of — for any individual, each of those tests have plusses and minuses that are best decided in the context of the patient and the physician making the decision that’s best for them. So I don’t know that there’s any one test that’s better for seniors versus another. The important message is that you need to avail yourself of at least one of them.
|
*QuickTime, Winamp, Real Player, or Microsoft Windows Media Player is required to access these files. If you do not have these media players, you can download them free of charge from Apple.com, Winamp.com, Real.com, and Microsoft. |
Photos/Stills
|
 NCI NewsCenter
NCI NewsCenter NCI Budget Data
NCI Budget Data Visuals Online
Visuals Online NCI Fact Sheets
NCI Fact Sheets Understanding Cancer Series
Understanding Cancer Series