Go to Animation - Still image from BenchMarks Animation - Jet Stream Dispersing I-131 across the U.S.
One of the hopeful messages from cancer research is that most of the cases of cancer are linked to environmental causes and, in principle, can be prevented. Together, the National Cancer Institute (NCI) and the National Institute of Environmental Health Sciences have recently published a new booklet titled “Cancer and the Environment,” which focuses on the agents in the environment that cause cancer and what we can do to lower our cancer risk. Environmental causes include both lifestyle factors such as smoking and diet, as well as exposure to agents in the air and water. The following interview with Aaron Blair, Ph.D., the chief of the Occupational Epidemiology Branch in NCI’s Division of Cancer Epidemiology and Genetics, will address the contribution of various agents to our overall cancer burden.
As far back as the 1960s, several studies have concluded that by acting on what we know about the causes of cancer, we could prevent the majority of cancers. Some reports even estimate that we could reduce the incidence of cancer by as much as 80-90 percent. What is your reaction to these assessments?
Most epidemiologists and cancer researchers would agree that the relative contribution from the environment toward cancer risk is about 80-90 percent. When I use the word “environmental,” I mean it in a broad sense to include both lifestyle factors such as diet, tobacco, and alcohol, as well as radiation, infectious agents, and substances in the air, water, and soil.
This information comes from studies that have been around for a long time. For example, if you look at migrant studies you find that people who migrate from an area of high cancer risk to an area of low cancer risk, or the reverse, within their lifetime take on the cancer rates of the country to which they move. Since the gene pool changes only after many generations, this means that these changes must be environmental, not genetic. And so, the migrant studies very clearly tell us that the wide range of cancer rates is largely driven by environmental causes.
Epidemiologic studies on risk factors tell us the same thing. For decades, scientists have been conducting epidemiological investigations looking at a variety of environmental and host genetic risk factors. And, almost always, the cancer burden is much greater for environmental causes than just the hereditable genetic factors.
There are several categories of agents in the environment that we know cause cancer — tobacco, alcohol, infectious agents, diet, medical drugs, occupational exposures, and ionizing radiation. Over the years, epidemiologists have made estimates as to the percentage of new cancer cases and cancer deaths caused by these agents (see table below). For example, the estimates for cancer deaths attributable to tobacco have been consistently around 30 percent and the proportion of cancers due to occupations, air and water pollution, medicines, and medical procedures are individually much smaller – most are less than 5 percent. Which of these estimates do we know with the most certainty?
We know with considerable certainty the estimates for tobacco. It is a single agent, many studies have been done, and we can fully and completely document that tobacco is a major contributor to cancer. One other factor that falls into the certain category is ionizing radiation. We really know a lot about the cancer risks associated with exposure to ionizing radiation. This includes radiation from many sources – cosmic rays, radon, X-rays, atomic bombs, and above ground nuclear bomb tests. So, the estimates for tobacco and ionizing radiation are very solid. However, the total contribution from all the other causes of cancer, such as diet, occupational exposures, or air and water pollution, may be correct, but we are less certain. This is because they are just so much harder to study. There are many more components to consider in studies of diet, medicines, or industrial products, for example. For these categories, we never know if we have really identified all the potential factors that contribute to the cancer risk in the population.
Although the proportion of cancer deaths caused by dietary factors account for the highest percentage, they also seem to be the least reliable data. Do you agree? Why is this data so uncertain?
The estimates made by two English epidemiologists, Richard Doll and Richard Peto, in the early 1980s are still reasonable (see table below). Tobacco is a major contributor. Diet probably is a major contributor. But our knowledge and certainty about diet is much less firm than tobacco. It’s undergoing a state of flux now. Things in the diet that we thought ten years ago were very clearly linked with increases of cancer – low fiber intake, for example — are less certain now. They haven’t gone away, but there are changes in thinking and contradictory findings in studies have confused the picture. But I think the estimate that diet may contribute 30-35 percent is probably right. But the certainty about this is not great. That’s because it’s really hard to figure out what the diet is. All diets are very complex, and it’s hard to determine exactly what people have eaten over time and the amount of micronutrients. So, tobacco and diet are major contributors. The other causes of cancer (medicinal, occupational, viral, radiation) fall in about the same range of 10 percent less.
It is known that dietary factors have a strong influence on cancer cases and death, but, at the same time, no single dietary factor aside from alcohol shows a strong and consistent enough effect to establish it unequivocally as an important carcinogen or anti-carcinogen. Is this because it is inherently difficult to tease out which factors in the diet have a strong influence on health or that there are no dietary factors that have a strong effect on cancer risk?
The major limitation is that it is so difficult to characterize a person’s diet over time. Typically it’s not the diet today that is important for the cancer diagnosed today. We need to know what people ate in the past, and that is really hard to determine. Investigators are getting better at this. The interviews are getting better. There are now some molecular and biological probes that provide us some information that can be useful. Progress is being made. But, it’s still a hard road.
What are some success stories where the environmental causes of cancer have been controlled and resulted in lower cancer rates?
Tobacco is a major success story. The proportion of the U.S. population that smoke has been going down for several decades, and just within the last decade, lung cancer rates have also started to go down. There is still room for improvement, but we can look with some pride at our successes in the tobacco arena.
There are a number of occupational exposures where we have been successful in decreasing harmful exposures. It’s a little hard to document exactly what the reduction in cancer risk has been, but there is evidence that it has occurred. It’s very clear that by understanding the relationship between occupational exposures and cancer, there have been real reductions in exposure to several toxic substances — arsenic, asbestos, and benzidine, for example. There are quite a number of chemicals that are under regulation in most countries around the world and there is some evidence that rates are decreasing for some cancers that are related to these exposures.
Today, for men, more than half of the new cancer cases and deaths are from prostate, lung, and colorectal cancers. For women, over half of the new cancer cases and deaths are due to breast, lung, and colorectal cancer. Do environmental factors account for most of these cancers? What is the evidence for this? Besides tobacco, are there any strong environmental contenders linked to these cancers?
There is very solid evidence that environmental factors are the major cause of cancer, although the specific environmental factors involved differ by tumor. Tobacco smoke is the major cause of lung cancer. But there is a long list of other chemicals that cause lung cancer – arsenic, asbestos, PAHs (polyaromatic hydrocarbons), and chromium, to name a few. For breast cancer, hormone use is one of the major factors affecting risk. Prostate cancer has nothing that reaches the level of evidence of lung or breast cancer, although there are a number of strong leads. Physical inactivity is strongly linked to colorectal cancer, as well as a number of dietary factors — low fiber is probably implicated.
In the nearly twenty-five years since Doll and Peto wrote their seminal analysis of the avoidable causes of cancer (1981), what new data has emerged to modify their estimates?
The estimates are still pretty solid, however, a few things have changed. When Doll and Peto wrote their article, there was very little information on viruses and bacteria. Since then, we have a lot of information. We now know that HIV and HPV are significant risk factors for certain cancers, and the bacterium H. pylori is an important risk factor in stomach cancer. There was a suspicion in the early 1980s that viruses were linked to cancer, but there was very little conclusive human data. Another area where strong information has emerged since the l980s are the health effects of physical activity and obesity — two environmental conditions also tied to diet. For example, physical inactivity is now pretty clearly related to cancers of the colon, breast, and prostate, and associations with additional cancer sites are likely to be made in the future.
A recent report estimated that, in the United States, 14 percent of deaths from cancer in men and 20 percent of deaths in women were due to obesity and being overweight. As you alluded to in the previous answer, obesity and being overweight were not mentioned in Doll and Peto’s 1981 report. Is there any other environmental/lifestyle factor that you would predict may emerge as a significant cause of cancer deaths within the next decade or two that only accounts for a small percentage of cancer deaths now?
My hunch is that general environmental exposures (pollutants in air and water) will be understood to be more important in the future decades. These won’t account for as large a percentage of cancers as tobacco, although they could rise above the 2-5 percent range because of the large numbers of people exposed. They were on Doll and Peto’s list, but there was very little information to back up their estimates (see table below). Doll and Peto assumed that several environmental exposures in the industrial arena were the same as in the general population. Researchers are beginning to focus on potentially hazardous substances in the water and air. This is a difficult research area and is every bit as hard to study as diet. My suspicion is that we will have much more solid information in the next couple of decades about how these things may contribute to cancer. Now we’re reasoning by analogy rather than from real data.
There is currently a lot of information on obesity, but it may be that physical inactivity will turn out to be every bit as important as obesity. Obesity has gotten more attention, in part, because it’s easier to study. People remember their weight more easily than they remember physical activity patterns. In addition, to take a good physical activity history involves a much longer questionnaire than required for obesity, and even then there can be considerable misclassification. Weight is just a lot easier to study. However, weight and physical activity are tied together. It’s not exactly clear which one is the most important. Probably both contribute to cancer risk. I think in the next few decades we will get much of this sorted out. There is some evidence that people who are physically fit, but overweight, have lower total mortality rates than people who are thin and not fit. That tells you that fitness may be important for general health, and I suspect this will be the case for cancer, too. We also keep adding to the cancer sites which appear to be a linked with physical activity. It’s very clear that colorectal and breast cancers are linked to physical activity, and prostate, lung, ovarian, and endometrial cancers are probably linked, too.
It is estimated that there are over 100,000 chemicals commonly used by Americans in household cleaners, solvents, pesticides, food additives, lawn care, and other products. And every year, another 1,000 or so are introduced. However, our National Toxicology Program only tests between 5-20 suspected carcinogens every year. For some people, our ignorance about most of the products in the environment is alarming; others are encouraged by the benefits that have already been demonstrated from the control of known causes of cancer. What is your reaction to these statistics?
Our ability to identify hazardous chemicals in the environment is better than these numbers suggest. There is actually a pyramid effect here. It’s true that not many bioassays are done every year – these cost millions of dollars to do and take a long time. But there are many experimental steps undertaken prior to launching bioassays that help identify the chemicals or classes of chemicals that have the best chance of being a health problem. The bioassays are, therefore, only carried out on chemicals that have already gone through a number of tests that indicate that we ought to be concerned about them. It is correct that many chemicals have not been put through a standard bioassay, but they are usually the ones for which there are no other data to suggest they might be hazardous. So I think we’re doing a lot better than the numbers would suggest. Of course, there will be some that we miss. For example, some substance may not cause genetic alterations — one of the laboratory tests we use to screen for possible cancer-causing substances — but may cause cancer through some immune system activity. So, it will test negative and would not be considered as a candidate for a bioassay. However, another reassuring observation is that many substances that we suspected would cause cancer in animals actually do not. Of course, it is possible that they do cause cancer in humans, but, in fact, our experience has shown us that most of the chemicals we have tested don’t cause cancer.
_______________
Proportion of cancer deaths caused by different avoidable cancers
|
Causes |
Percent 1981(US)* |
Percent 1998(UK)** |
|
Tobacco |
25-40 |
29-31 |
|
Diet |
10-70 |
20-50 |
|
Medicines |
0.3-1.5 |
<1 |
|
Infection: parasites, bacteria, viruses |
10 best estimate |
10-20 |
|
Ionizing and UV light |
2-4 |
5-7 |
|
Occupation |
2-8 |
2-4 |
|
Pollution: air, water, food |
<1-5 |
1-5 |
|
Physical inactivity |
|
1-2 |
*Doll R and Peto R. The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States today. Journal of the National Cancer Institute 1981;66:1191-1308.
**Doll R. Epidemiological evidence of the effects of behavior and the environment on the risk of human cancer. Recent Results in Cancer Research 1998;154:3-21.
Animation/Video
|
|
|
| This animation requires the Flash plug-in. If you do not have the plug-in, please click here to install. | |
Text Transcript
First scene: Iodine I-131 ( I-131) was among the radioactive materials released by the atomic bomb tests. (military observers watch mushroom cloud rise above desert.)
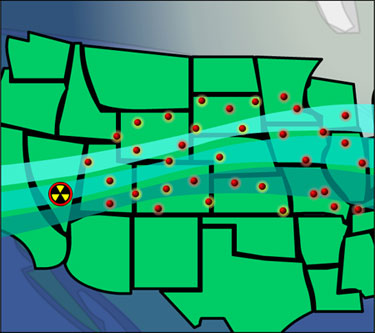
Second scene: It was carried thousands of miles away from the test areas on the winds. Because of wind and rainfall patterns, the distribution of fallout varied widely after each test. Therefore, although all areas of the U.S. received fallout from at least one nuclear weapons test, certain areas of North America received more fallout than others. (jet stream disperses I-131, shown as pulsing red dots, across the United States.)
Third scene: I-131 traveled to all states, particularly those in the Midwestern, Eastern, and Northeastern United States, where it fell with the rain. (rain contaminated with I-131 falls on a wheat field.)
Fourth scene: Some of the I-131 collected on pastures and on grasses, where it was consumed by cows and goats. (two grazing cows graze in a field contaminated by rain carrying I-131 particles.)
Fifth scene: When consumed by cows or goats, I-131 collects in the animals’ milk. Eating beef from cows exposed to I-131 carried little risk. (a dairy farmer milks a cow. I-131 particles are seen in the pail of fresh milk.)
Sixth scene: Much of the health risk associated with I-131 occurred among milk-drinkers-usually children. (a child is shown drinking milk containing I-131 particles.)
Seventh scene: From what is known about thyroid cancer and radiation, scientists think that people who were children during the period of atomic bomb testing are at higher risk for developing thyroid cancer. (the scene zooms in to the child’s neck, continuing to zoom in to show a strand of DNA. a particle of I-131 strikes the DNA, mutating it. the mutated DNA replicates, causing thyroid cancer.)
Photos/Stills
1. Iodine I-131 ( I-131) was among the radioactive materials released by released by above-ground atomic tests.
2. It was carried thousands of miles away from the test areas on the winds. Because of wind and rainfall patterns, the distribution of fallout varied widely after each test.
3. Much of the health risk associated with I-131 occurred among milk drinkers-usually children.

4. From what is known about thyroid cancer and radiation, scientists think that people who were children during the period of atomic bomb testing are at higher risk for developing thyroid cancer.

 NCI NewsCenter
NCI NewsCenter NCI Budget Data
NCI Budget Data Visuals Online
Visuals Online NCI Fact Sheets
NCI Fact Sheets Understanding Cancer Series
Understanding Cancer Series