What is screening?
Screening is looking for cancer before a person has any symptoms. This can help find cancer at an early stage. When abnormal tissue or cancer is found early, it may be easier to treat. By the time symptoms appear, cancer may have begun to spread.
Scientists are trying to better understand which people are more likely to get certain types of cancer. They also study the things we do and the things around us to see if they cause cancer. This information helps doctors recommend who should be screened for cancer, which screening tests should be used, and how often the tests should be done.
It is important to remember that your doctor does not necessarily think you have cancer if he or she suggests a screening test. Screening tests are given when you have no cancer symptoms.
If a screening test result is abnormal, you may need to have more tests done to find out if you have cancer. These are called diagnostic tests.
General Information About Cervical Cancer
Key Points for This Section
- Cervical cancer is a disease in which malignant (cancer) cells form in the cervix.
- Screening for cervical cancer using the Pap test has decreased the number of new cases of cervical cancer and the number of deaths due to cervical cancer since 1950.
- Human papillomavirus (HPV) infection is the major risk factor for development of cervical cancer.
Cervical cancer is a disease in which malignant (cancer) cells form in the cervix.
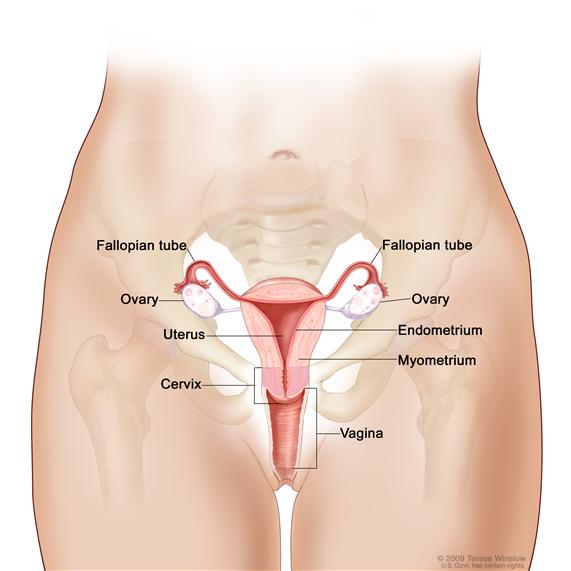
The cervix is the lower, narrow end of the uterus (the hollow, pear-shaped organ where a fetus grows). The cervix leads from the uterus to the vagina (birth canal).
Cervical cancer usually develops slowly over time. Before cancer appears in the cervix, the cells of the cervix go through changes known as dysplasia, in which cells that are not normal begin to appear in the cervical tissue. Later, cancer cells start to grow and spread more deeply into the cervix and to surrounding areas.
See the following PDQ summaries for more information about cervical cancer:
Screening for cervical cancer using the Pap test has decreased the number of new cases of cervical cancer and the number of deaths due to cervical cancer since 1950.
Cervical dysplasia occurs more often in women who are in their 20s and 30s. Death from cervical cancer is rare in women younger than 30 years and in women of any age who have regular screenings with the Pap test. The Pap test is used to detect cancer and changes that may lead to cancer. The chance of death from cervical cancer increases with age. Deaths from cervical cancer occur more often in black women than in white women.
Human papillomavirus (HPV) infection is the major risk factor for development of cervical cancer.
Although most women with cervical cancer have the human papillomavirus (HPV) infection, not all women with an HPV infection will develop cervical cancer. Many different types of HPV can affect the cervix and only some of them cause abnormal cells that may become cancer. Some HPV infections go away without treatment.
HPV infections are spread mainly through sexual contact. Women who become sexually active at a young age and have many sexual partners are at increased risk for HPV infections.
Other risk factors for cervical cancer include:
- Giving birth to many children.
- Having many sexual partners.
- Having first sexual intercourse at a young age.
- Smoking cigarettes.
- Using oral contraceptives ("the Pill").
- Having a weakened immune system.
Cervical Cancer Screening
Key Points for This Section
Tests are used to screen for different types of cancer.
Some screening tests are used because they have been shown to be helpful both in finding cancers early and in decreasing the chance of dying from these cancers. Other tests are used because they have been shown to find cancer in some people; however, it has not been proven in clinical trials that use of these tests will decrease the risk of dying from cancer.
Scientists study screening tests to find those with the fewest risks and most benefits. Cancer screening trials also are meant to show whether early detection (finding cancer before it causes symptoms) decreases a person's chance of dying from the disease. For some types of cancer, the chance of recovery is better if the disease is found and treated at an early stage.
Clinical trials that study cancer screening methods are taking place in many parts of the country. Information about ongoing clinical trials is available from the NCI Web site.
Studies show that screening for cervical cancer helps decrease the number of deaths from the disease.
Regular screening of women between the ages of 25 and 60 years with the Pap test decreases their chance of dying from cervical cancer. In women younger than 25 years, screening with the Pap test may show changes in the cells of the cervix that are not cancer but lead to further testing and possibly treatment. Screening with the Pap test is not helpful in women older than 60 years who have had recent negative Pap tests.
A Pap test is commonly used to screen for cervical cancer.
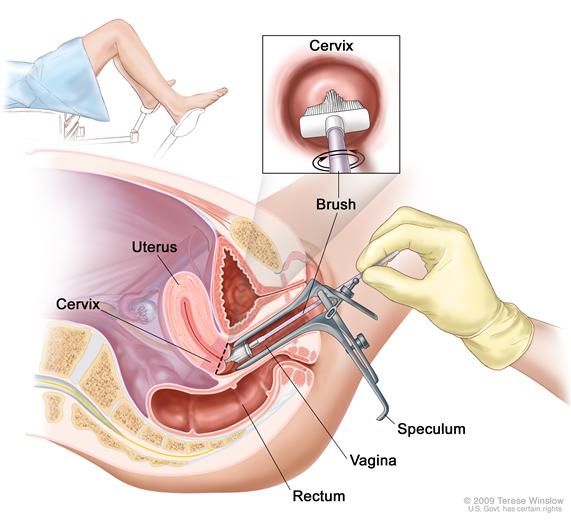
A Pap test is a procedure to collect cells from the surface of the cervix and vagina. A piece of cotton, a brush, or a small wooden stick is used to gently scrape cells from the cervix and vagina. The cells are viewed under a microscope to find out if they are abnormal. This procedure is also called a Pap smear. A new method of collecting and viewing cells has been developed, in which the cells are placed into a liquid before being placed on a slide. It is not known if the new method will work better than the standard method to reduce the number of deaths from cervical cancer.
After certain positive Pap test results, an HPV DNA test or an HPV RNA test may be done .
These tests are used to find out if the HPV infection that is causing the abnormal cells is one that is linked to cervical cancer. In women aged 30 or older, an HPV DNA test and the Pap test are used to screen for HPV infection. In women younger than 30 years, HPV infections are common but usually do not last long or cause problems.
Other screening tests are being studied in clinical trials.
Screening clinical trials are taking place in many parts of the country. Information about ongoing clinical trials is available from the NCI Web site.
Risks of Cervical Cancer Screening
Key Points for This Section
Decisions about screening tests can be difficult. Not all screening tests are helpful and most have risks. Before having any screening test, you may want to discuss the test with your doctor. It is important to know the risks of the test and whether it has been proven to reduce the risk of dying from cancer.
The risks of cervical cancer screening include the following:
False-negative test results can occur.
Screening test results may appear to be normal even though cervical cancer is present. A woman who receives a false-negative test result (one that shows there is no cancer when there really is) may delay seeking medical care even if she has symptoms.
False-positive test results can occur.
Screening test results may appear to be abnormal even though no cancer is present. Also, some abnormal cells in the cervix never become cancer. A false-positive test result (one that shows there is cancer when there really isn't) can cause anxiety and is usually followed by more tests and procedures (such as colposcopy, cryotherapy, or LEEP), which also have risks. The long-term effects of these procedures on fertility and pregnancy are not known.
Women aged 20 to 24 are most likely to have abnormal Pap test results that lead to further testing and treatment. HPV DNA tests find many infections that will not lead to dysplasia or cervical cancer, especially in women younger than 30 years.
Your doctor can advise you about your risk for cervical cancer and your need for screening tests.
Studies show that the number of cases of cervical cancer and deaths from cervical cancer are greatly reduced by screening with Pap tests. Many doctors recommend a Pap test be done every year. New studies have shown that after a woman has a Pap test and the results show no sign of abnormal cells, the Pap test can be repeated every 2 to 3 years.
The Pap test is not a helpful screening test for cervical cancer in the following groups of women:
- Women who are younger than 25 years.
- Women who have had a total hysterectomy (surgery to remove the uterus and cervix) for a condition that is not cancer.
- Women who are aged 60 years or older and have a Pap test result that shows no abnormal cells. These women are very unlikely to have abnormal Pap test results in the future.
The decision about how often to have a Pap test is best made by you and your doctor.
Changes to This Summary (07/19/2012)
The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above.
Changes were made to this summary to match those made to the health professional version.
Questions or Comments About This Summary
If you have questions or comments about this summary, please send them to Cancer.gov through the Web site’s Contact Form. We can respond only to email messages written in English.
Get More Information From NCI
Call 1-800-4-CANCER
For more information, U.S. residents may call the National Cancer Institute's (NCI's) Cancer Information Service toll-free at 1-800-4-CANCER (1-800-422-6237) Monday through Friday from 8:00 a.m. to 8:00 p.m., Eastern Time. A trained Cancer Information Specialist is available to answer your questions.
Chat online
The NCI's LiveHelp® online chat service provides Internet users with the ability to chat online with an Information Specialist. The service is available from 8:00 a.m. to 11:00 p.m. Eastern time, Monday through Friday. Information Specialists can help Internet users find information on NCI Web sites and answer questions about cancer.
Write to us
For more information from the NCI, please write to this address:
- NCI Public Inquiries Office
- Suite 3036A
- 6116 Executive Boulevard, MSC8322
- Bethesda, MD 20892-8322
Search the NCI Web site
The NCI Web site provides online access to information on cancer, clinical trials, and other Web sites and organizations that offer support and resources for cancer patients and their families. For a quick search, use the search box in the upper right corner of each Web page. The results for a wide range of search terms will include a list of "Best Bets," editorially chosen Web pages that are most closely related to the search term entered.
There are also many other places to get materials and information about cancer treatment and services. Hospitals in your area may have information about local and regional agencies that have information on finances, getting to and from treatment, receiving care at home, and dealing with problems related to cancer treatment.
Find Publications
The NCI has booklets and other materials for patients, health professionals, and the public. These publications discuss types of cancer, methods of cancer treatment, coping with cancer, and clinical trials. Some publications provide information on tests for cancer, cancer causes and prevention, cancer statistics, and NCI research activities. NCI materials on these and other topics may be ordered online or printed directly from the NCI Publications Locator. These materials can also be ordered by telephone from the Cancer Information Service toll-free at 1-800-4-CANCER (1-800-422-6237).
About PDQ
PDQ is a comprehensive cancer database available on NCI's Web site.
PDQ is the National Cancer Institute's (NCI's) comprehensive cancer information database. Most of the information contained in PDQ is available online at NCI's Web site. PDQ is provided as a service of the NCI. The NCI is part of the National Institutes of Health, the federal government's focal point for biomedical research.
PDQ contains cancer information summaries.
The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries are available in two versions. The health professional versions provide detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions provide current and accurate cancer information.
Images in the PDQ summaries are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in the PDQ summaries, along with many other cancer-related images, are available in Visuals Online, a collection of over 2,000 scientific images.
The PDQ cancer information summaries are developed by cancer experts and reviewed regularly.
Editorial Boards made up of experts in oncology and related specialties are responsible for writing and maintaining the cancer information summaries. The summaries are reviewed regularly and changes are made as new information becomes available. The date on each summary ("Date Last Modified") indicates the time of the most recent change.
PDQ also contains information on clinical trials.
A clinical trial is a study to answer a scientific question, such as whether a method of finding cancer earlier can help people to live longer. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients and those who are at risk for cancer. During screening clinical trials, information is collected about the effects of a new screening method and how well it works. If a clinical trial shows that a new method is better than one currently being used, the new method may become "standard." People who are at high risk for a certain type of cancer may want to think about taking part in a clinical trial.
Listings of clinical trials are included in PDQ and are available online at NCI's Web site. Descriptions of the trials are available in health professional and patient versions. Many cancer doctors who take part in clinical trials are also listed in PDQ. For more information, call the Cancer Information Service 1-800-4-CANCER (1-800-422-6237).

