Peripheral Arterial Disease (PAD) Fact Sheet
Download this fact sheet [PDF–307K]
Peripheral Arterial Disease (PAD) in the Legs
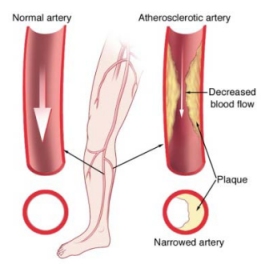
or lower extremities is the narrowing or blockage of the vessels that carry blood from the heart to the legs. It is primarily caused by the buildup of fatty plaque in the arteries, which is called atherosclerosis. PAD can occur in any blood vessel, but it is more common in the legs than the arms.

Risk Factors for PAD
- Smoking
- High blood pressure
- Atherosclerosis
- Diabetes
- High cholesterol
- Older than age 60
 Men and woman are equally affected by PAD; however, black race/ethnicity is associated with an increased risk of PAD. People of Hispanic origin may have similar to slightly higher rates of PAD compared to non-Hispanic whites. Approximately 8 million people in the United States have PAD, including 12-20% of individuals older than age 60. General population awareness of PAD is estimated at 25%, based on prior studies.2
Men and woman are equally affected by PAD; however, black race/ethnicity is associated with an increased risk of PAD. People of Hispanic origin may have similar to slightly higher rates of PAD compared to non-Hispanic whites. Approximately 8 million people in the United States have PAD, including 12-20% of individuals older than age 60. General population awareness of PAD is estimated at 25%, based on prior studies.2
Other clinical conditions and disorders of arteries can mimic the symptoms of PAD, and not all PAD is due to atherosclerosis.3-4
In this image, a normal artery is shown on the left. The right shows an artery narrowed by atherosclerosis, causing PAD. Photo courtesy of Michigan Medical Report (http://www.michiganmedicalreport.com).
Signs and Symptoms of PAD
The classic symptom of PAD is pain in the legs with exertion such as walking, which is relieved by resting. However, up to 40% of individuals with PAD have no leg pain. Symptoms of pain, ache, or cramp with walking (claudication) can occur in the buttock, hip, thigh, or calf.3
Physical signs in the leg that may indicate peripheral arterial disease include muscle atrophy, hair loss, smooth shiny skin, skin that is cool to the touch especially if accompanied by pain while walking (which is relieved by stopping walking), decreased or absent pulses in the feet, non-healing ulcers or sores in the legs or feet, and cold or numb toes.3,4
Preventing PAD
 Physical activity and exercise are important for preventing PAD and for improving symptoms of PAD.3
Physical activity and exercise are important for preventing PAD and for improving symptoms of PAD.3- Avoid use of tobacco—smoking increases the risk of PAD by 2-6 times and it worsens the symptoms of PAD.5
- Control high blood pressure, cholesterol, and diabetes.
Supervised exercise training programs can improve and prolong walking distance in individuals with PAD.
Diagnosis and Treatment of PAD
In patients with symptoms of PAD, the ankle-brachial index (ABI) is a non-invasive test that measures the blood pressure in the ankles and compares it with the blood pressure in the arms at rest and after exercise. Imaging tests such as ultrasound, magnetic resonance angiography (MRA), and computed tomographic (CT) angiography can provide additional information in diagnosing PAD.2-4
- Individuals with PAD are at risk for developing coronary artery disease and cerebrovascular disease, which could lead to a heart attack or stroke.5
- Aspirin or other similar anti-platelet medications may prevent the development of serious complications from PAD and associated atherosclerosis.3,5
- All efforts must be made to stop smoking.
- Severe cases may require surgery to bypass blocked arteries.
References
- Allison MA, Ho E, Denenberg JO, et al. Ethnic-specific prevalence of peripheral arterial disease in the United States. 2007 American Journal of Preventive Medicine 2007;32:328-333.
- Roger VL, Go AS, Lloyd-Jones DM, et. al. Heart Disease and Stroke Statistics 2011 Update: A Report From the American Heart Association. Circulation 2011;123:e18-e209.
- Creager MA, Loscalzo J. Vascular Diseases of the Extremities. In: Fauci AS, Braunwald E, Kasper DL, et al., eds. Harrison's Principles of Internal Medicine. 17e ed. New York: McGraw Hill, 2008.
- Rooke TW, Wennberg PW. Diagnosis and Management of Diseases of the Peripheral Arteries and Veins. In: Walsh RA, Simon DI, Hoit BD, et al., eds.: Hurst’s The Heart. 12e ed. New York: McGraw Hill, 2007.
- Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 Practice guidelines for the management of patients withi peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): Circulation. 2006;113:e463-654.
Get email updates
To receive email updates about this page, enter your email address:
Contact Us:
- CDC/NCCDPHP/DHDSP
4770 Buford Hwy, NE
Mail Stop F-72
Atlanta, GA 30341-3717 - Call: 800-CDC-INFO
TTY: 800-232-6348
Fax: 770-488-8151 - cdcinfo@cdc.gov



