 |
||
| http://ghr.nlm.nih.gov/ A service of the U.S. National Library of Medicine® | ||
The official name of this gene is “keratin 16.”
KRT16 is the gene's official symbol. The KRT16 gene is also known by other names, listed below.
The KRT16 gene provides instructions for making a protein called keratin 16 or K16. Keratins are a group of tough, fibrous proteins that form the structural framework of certain cells, particularly cells that make up the skin, hair, and nails. Keratin 16 is produced in the nails, the skin on the palms of the hands and soles of the feet, and the oral mucosa that lines the inside of the mouth.
Keratin 16 partners with a similar protein, keratin 6a, to form molecules called keratin intermediate filaments. These filaments assemble into dense networks that provide strength and resilience to the skin, nails, and other tissues. Networks of keratin filaments protect these tissues from being damaged by friction and other everyday physical stresses. Keratin 16 is also among several keratins involved in wound healing.
The KRT16 gene belongs to a family of genes called KRT (keratins).
A gene family is a group of genes that share important characteristics. Classifying individual genes into families helps researchers describe how genes are related to each other. For more information, see What are gene families? (http://ghr.nlm.nih.gov/handbook/howgeneswork/genefamilies) in the Handbook.
At least four KRT16 gene mutations have been found to cause focal palmoplantar keratoderma. This condition causes painful blisters and calluses to develop on the soles of the feet and, less commonly, on the palms of the hands. It is sometimes considered a mild form (variant) of pachyonychia congenita (described below) because the blisters and calluses are similar. However, most people with focal palmoplantar keratoderma do not have the severe nail abnormalities or other skin problems that are characteristic of pachyonychia congenita.
Two of the KRT16 gene mutations associated with focal palmoplantar keratoderma change single protein building blocks (amino acids) in the keratin 16 protein. Another mutation deletes a large region of the keratin 16 protein. These genetic changes alter the structure of the keratin 16 protein and interfere with the assembly of the keratin intermediate filament network. Skin cells with defective keratin are fragile and prone to damage, making the skin less resistant to friction and minor trauma.
The soles of the feet experience a significant amount of friction compared with many other parts of the body and must bear the body's weight, which may help explain why blisters and calluses occur primarily in this area in people with focal palmoplantar keratoderma. However, it is unclear why some mutations in the KRT16 gene cause this condition and others lead to the more severe features of pachyonychia congenita.
At least 19 mutations in the KRT16 gene have been identified in people with pachyonychia congenita. In most cases, this condition becomes apparent within the first few months of life, but KRT16 gene mutations are also associated with a rare form of the disorder (pachyonychia congenita tarda) that appears in adolescence or early adulthood. Most of the KRT16 gene mutations associated with pachyonychia congenita change single amino acids in keratin 16. A few mutations delete a small number of amino acids from the protein.
The KRT16 gene mutations responsible for pachyonychia congenita change the structure of keratin 16, preventing it from interacting effectively with keratin 6a and interfering with the assembly of the keratin intermediate filament network. Without this network, skin cells become fragile and are easily damaged, making the skin less resistant to friction and minor trauma. Even normal activities such as walking can cause skin cells to break down, resulting in the formation of severe, painful blisters and calluses. Additionally, fragile skin cells may abnormally produce more keratin in response to damage, which makes the skin problems worse. Defective keratin 16 also disrupts the growth and function of cells in the nails and oral mucosa, which explains why the signs and symptoms of pachyonychia congenita also affect these tissues.
Cytogenetic Location: 17q21.2
Molecular Location on chromosome 17: base pairs 39,766,029 to 39,769,078
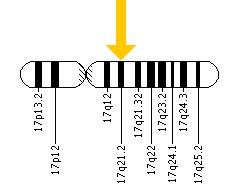
The KRT16 gene is located on the long (q) arm of chromosome 17 at position 21.2.
More precisely, the KRT16 gene is located from base pair 39,766,029 to base pair 39,769,078 on chromosome 17.
See How do geneticists indicate the location of a gene? (http://ghr.nlm.nih.gov/handbook/howgeneswork/genelocation) in the Handbook.
You and your healthcare professional may find the following resources about KRT16 helpful.
You may also be interested in these resources, which are designed for genetics professionals and researchers.
See How are genetic conditions and genes named? (http://ghr.nlm.nih.gov/handbook/mutationsanddisorders/naming) in the Handbook.
acids ; amino acid ; blister ; callus ; cell ; cytokeratin ; domain ; gene ; intermediate filaments ; keratin ; keratoderma ; molecule ; motif ; mucosa ; mutation ; pachyonychia ; palmoplantar keratoderma ; protein ; resilience ; sign ; stress ; symptom ; tissue ; trauma
You may find definitions for these and many other terms in the Genetics Home Reference Glossary (http://ghr.nlm.nih.gov/glossary).
The resources on this site should not be used as a substitute for professional medical care or advice. Users seeking information about a personal genetic disease, syndrome, or condition should consult with a qualified healthcare professional. See How can I find a genetics professional in my area? (http://ghr.nlm.nih.gov/handbook/consult/findingprofessional) in the Handbook.