Office of Medicare Hearings and Appeals (OMHA)
Understanding the Appeals Process
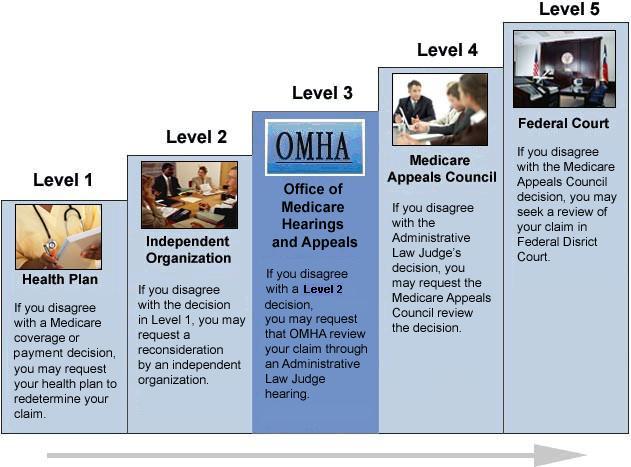
OMHA is responsible for Level 3 claims appeals. The entry point of the appeals process depends on the part of the Medicare program that covers the disputed benefit or whether the beneficiary is enrolled in a Medicare Advantage plan. For more information on the different entry points based on Medicare Part, see Appeals Process by Medicare Type.
There are five levels in the Medicare claims appeal process. The appeals process begins at Level 1. Select a level below to learn more about any of the appeals levels (text only version of graphic).
Guaranteed Rights
If you are a Medicare beneficiary, you have certain guaranteed rights. One of these is the right to a fair process to appeal decisions about your health care coverage or payment. No matter what kind of Medicare you have, you may have the right to appeal these decisions.
You can appeal if:
- A service or item you received isn’t covered, and you think it should be;
- A service or item is denied, and you think it should be paid; and/or
- You question the amount that Medicare paid.
You can also appeal other decisions of the Medicare program on non-medical issues. An example of such an issue is your eligibility for the Medicare program if your application to enroll in Medicare was denied.
Please note that the Office of Medicare Hearings and Appeals is responsible only for the Level 3 claims appeals and certain Medicare eligibility and Part B premium appeals. OMHA is not responsible for levels 1, 2, 4, and 5 of the appeals process. OMHA provides additional information on other levels of appeals to help you understand the appeals process in a broad context.