Revised September 2012
Overview
Genetic, neurobiological, and prevention research suggest that a generalized inability to control one’s behavior and emotions predisposes an individual to substance use and other psychiatric disorders. However, knowledge of a common liability factor does not necessarily shed light on which disorders will develop, or on what sorts of treatment will be most effective. Once a specific disorder or comorbidity develops, disease-specific neuroadaptations and epigenetic modifications may come into play, induced by exposure to abused substances or other environmental factors. This symposium will present recent studies that investigate the neural substrates of behavioral regulation and new approaches to testing the usefulness of a construct of a “dysregulation syndrome” for understanding the etiology of specific disorders and how to treat them.
Neural Mechanisms Linking Behavioral Dysregulation in Substance Abuse, Psychopathology, and Stress
Anthony A. Grace, Ph.D., University of Pittsburgh
 Download the PDF Presentation (PDF, 2.2MB)
Download the PDF Presentation (PDF, 2.2MB)External stressors do not create identical responses within the nervous system. This is evident in the adaptive reactions to stress that benefit survival by motivating us to avoid dangerous situations, as well as the maladaptive reactions that lead to drug abuse, post-traumatic stress disorder, and depression. Dr. Grace presented research suggesting that stressors that vary in intensity and duration can affect the dopamine (DA) system in different ways. He began by discussing the types of stressors—noxious, physiological, and psychological—and the unique ways they affect our nervous system. Dr. Grace and his research team used footshocks, restraint, and exposure to chronic cold to simulate the effects of unique brain stressors.
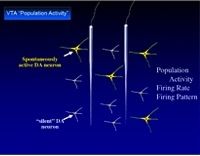
Dr. Grace explained the processes used to observe the activity of DA neurons in the ventral tegmental area (VTA) and responses to stressors, including counting the number of neurons firing spontaneously, measuring the average firing rate and neuronal patterns, and assessing amphetamine-induced locomotor activity. Results showed that intense noxious or psychological stressors activated the DA system and increased behavioral response to amphetamine. Dr. Grace explained that this condition illustrated the type of response that might occur with post-traumatic stress disorder or anxiety disorders. In contrast, mild inescapable stressors depressed the reward-related DA neurons, which is consistent with an individual’s inability to gain pleasure from enjoyable experiences in cases of depression. The uniqueness of these stress responses lends to unique impacts on an individual’s risk for abusing drugs that act on the DA system.
An Evolutionary Perspective on Behavioral Syndromes: Insights from Whole Genome Expression Data
Alison M. Bell, Ph.D., University of Illinois, Champaign-Urbana
 Download the PDF Presentation (PDF, 1MB)
Download the PDF Presentation (PDF, 1MB)External stressors do not create identical responses within the nervous system. This is evident in the adaptive reactions to stress that benefit survival by motivating us to avoid dangerous situations, as well as the maladaptive reactions that lead to drug abuse, post-traumatic stress disorder, and depression. Dr. Grace presented research suggesting that stressors that vary in intensity and duration can affect the dopamine (DA) system in different ways. He began by discussing the types of stressors—noxious, physiological, and psychological—and the unique ways they affect our nervous system. Dr. Grace and his research team used footshocks, restraint, and exposure to chronic cold to simulate the effects of unique brain stressors.
The Neurocircuitry of Emotion Regulation: The Control of Fear and Implications for Treatment of PTSD and Comorbid Disorders
Elizabeth A. Phelps, Ph.D., New York University
There are several brain regions involved in the regulation of emotion in human beings, including the prefrontal cortex, hippocampus, and amygdala. Dr. Phelps and her team of researchers used animal model research and observations of similar behavior in human beings to determine how we can control and diminish responses to fear through extinction, reconsolidation, and emotional regulation. Comparisons of research on fear conditioning in rats and humans illustrate that both species show similar responses, including increases in blood pressure, heart rate, and respiration, and the release of stress hormones. This presentation discussed coping techniques that can influence how humans regulate emotions and techniques for altering emotional responses, including disrupting the neurological/psychological process that occurs when long-term memories are drawn out, strengthened, or re-imprinted.
Extinction takes places when repeated exposure to a learned fear stimulus with no aversive consequences results in new learning that the conditioned stimulus is now safe. It forms the basis for exposure therapy treatment of phobias. Animal models show that activity in the ventral medial prefrontal cortex (vmPFC) is necessary for extinction to occur and that the amygdala plays a key role in its success. Dr. Phelps explained how cognitive therapists use emotional regulation to help patients reassess whether to associate a stimulus with a negative affect into neutral or positive emotional terms. In this case, the vmPFC controls fear by inhibiting the amygdala, which controls expression and helps with the formation and storage of memories associated with emotional events. She also explained study results relating to the reconsolidation of a conditioned fear response and the retrieval–extinction procedure, known to act on neural circuits in the brain to prevent drug craving and relapse.





