In the Clinic
Childhood Cancers in Translation
Despite the fact that approximately 80 percent of children with acute lymphoblastic leukemia (ALL) are cured with current chemotherapy regimens, ALL remains a leading cause of death from cancer in childhood. Furthermore, side effects of standard therapies have lifelong consequences for many survivors of childhood ALL. Alan Wayne, M.D., Head of the Hematologic Diseases Section of CCR’s Pediatric Oncology Branch, works with a team of investigators to develop novel targeted approaches to treat ALL and other childhood leukemias and lymphomas in hopes that these new therapies will prove more potent and less toxic than those currently available.
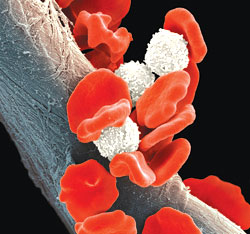
Image shows that, in leukemia, abnormal white blood cells proliferate and circulate. (Photo: iStockphoto.com)
When asked how he got his start in leukemia research, Alan Wayne explains that early in childhood he was given a microscope along with glass slides of cases of acute lymphoblastic leukemia (ALL) from his father, an internist and hematologist. A National Science Foundation-sponsored high school summer internship at the Roswell Park Memorial Institute with the late Jun Minowada, M.D., who developed many of the modern leukemia cell lines, further steered his interests toward blood cancers. Years later, he worked as a resident, fellow, and then faculty member at the Children’s Hospital and Dana-Farber Cancer Institute in Boston where the late Sidney Farber, M.D., achieved the first remissions in childhood ALL.
Decades after those formative experiences, Wayne serves as the Clinical Director of the CCR’s Pediatric Oncology Branch. He directs a clinical research program focused on ALL, including two ongoing clinical trials for relapsed ALL that were developed as a result of translational research conducted by CCR investigators.
A Targeted Toxin
Moxetumomab pasudotox, also known as CAT-8015 or HA22, is the product of work undertaken in the laboratory of Ira Pastan, M.D., Chief of the Laboratory of Molecular Biology at CCR. [see “A Better Immunotoxin,” CCR connections Vol. 2 No. 1]. It is a recombinant immunotoxin—an engineered drug made up of two components. One component is an antibody-derived molecule that binds to a protein called CD22 on the surface of cells. The other component is a potent bacterial toxin known as pseudomonas exotoxin A that causes cell death by inhibiting protein synthesis.

Image shows a standard approach in the treatment of many blood-based cancers that have relapsed after transplantation is to transfuse lymphocytes (a type of white blood cell) from the transplant donor. In the WT-1 immunotherapy trial, white blood cells called mononuclear cells are also isolated from the donor. These cells are matured in the laboratory into immune cells called dendritic cells, and then exposed to protein molecules that are found primarily in cancer cells. The dendritic cells will take up the tumor peptides, process them, and display them on the cell surface, where they will be “visible” to other immune cells. Then, the dendritic cells are injected into the patient, where it is hoped they will stimulate an immune response that selectively targets and kills cells that have the target molecules. (Image: NIH Medical Arts)
Moxetumomab pasudotox is a second generation anti-CD22 immunotoxin that was derived from a predecessor agent, CAT-3888 or BL22. MedImmune, LLC is sponsoring a multicenter phase I clinical trial of moxetumomab pasudotox that is being conducted at the NIH, the Dana-Farber Cancer Institute/ Children’s Hospital Boston, and St. Jude Children’s Research Hospital.

Photo shows Research Nurses Sharon Mavroukakis (left) and Cindy Delbrook (right) displaying the documentation on WT-1 immunotherapy submitted to the Food and Drug Administration for the Investigational New Drug application. (Photo: A. Wayne)
A Fortified Immunotherapy
Another ongoing clinical trial that includes children with relapsed ALL is a vaccine-based approach that is designed to boost an anticancer immune response after stem cell transplantation. A standard approach in the treatment of many blood- based cancers that have relapsed after transplantation is to transfuse lymphocytes (a type of white blood cell) from the transplant donor. Such donor lymphocyte infusions (DLI) are extremely effective in some forms of leukemia, but are only rarely useful in the treatment of relapsed ALL. This new trial represents an attempt to try to improve the efficacy of DLI for ALL and other blood cancers.
Relapsed ALL, like a number of other cancers, is often associated with the expression of a protein known as Wilms Tumor-1 or WT-1. The immune response includes a class of cells known as dendritic cells that process proteins and present them to other cells of the immune system. This directs immune effector cells to recognize and destroy target cells. In this trial, dendritic cells derived from the donor of a prior stem cell transplant are programmed to present WT-1. These cells are then administered to the transplant recipient in an attempt to direct a DLI-associated immune response against ALL cells that express WT-1. The phase 1/2 WT-1 vaccine trial, which began in 2008, is open to children and adults from age 1 to 75.
Rare and Resistant
Children with relapsed ALL make up approximately 25 percent of the pediatric cancer patients that are currently participating in clinical trials conducted by the Pediatric Oncology Branch. But the Branch is pioneering multiple treatments for refractory childhood cancers.
Lee Helman, M.D., Head of the Molecular Oncology Section in CCR’s Pediatric Oncology Branch, has recently completed an international phase 2 study of a human monoclonal antibody against IGFR1, a molecule expressed in several cancer types. The trial included more than 140 patients with Ewing’s sarcoma (EWS), and although the overall response rate was very low, some patients had durable complete remissions.

Photo shows Crystal Mackall, M.D., working in the clinic.(Photo: E. Branson)
“Compared to anything else available to treat refractory EWS, we haven’t seen anything like it,” reported Helman. “We have a 14-year-old girl who came to us last Christmas time who was told there was nothing left to do for her. Now she is in complete remission, coming to get this antibody every three weeks. The multiple pulmonary nodules we saw are just completely gone and she has regained her normal weight.”
The [Pediatric Oncology] Branch is pioneering multiple treatments for refractory childhood cancers.
The challenge and frustration for Helman is that they don’t yet understand why only certain patients responded so well. “We still don’t know how to stratify them. And the frustration has been that the community really feels that this is worth pursuing but the companies that make these antibodies have seen much less activity in adult cancers and aren’t so interested in EWS.”
Helman notes that most patients that showed a response to the drug did relapse after a few months. However, the treatment involved only a single agent. As Crystal Mackall, M.D., Head of the Pediatric Oncology Branch observed, “We’d love to find a magic bullet that could be used as a single agent. But the ultimate success is going to come from a combination of approaches that together reduce the tumor burden and prevent recurrence.”


