You are here:
Related Information
- What Is Acne? (fast facts, easy-to-read)
- ¿Qué es el acné? (Esenciales: hojas informativas de fácil lectura)
- What Is Acne?

- Order a NIAMS publication to be mailed
Acne
Online version updated October 2012
Questions and Answers about Acne
This booklet contains general information about acne. It describes what acne is and how it develops, the causes of acne, and the treatment options for various forms of acne. Information is also provided on caring for the skin. If you have further questions after reading this booklet, you may wish to discuss them with your doctor.
What Is Acne?
Acne is a disorder resulting from the action of hormones and other substances on the skin’s oil glands (sebaceous glands) and hair follicles. These factors lead to plugged pores and outbreaks of lesions commonly called pimples or zits. Acne lesions usually occur on the face, neck, back, chest, and shoulders. Although acne is usually not a serious health threat, it can be a source of significant emotional distress. Severe acne can lead to permanent scarring.
- How Does Acne Develop?
- What Causes Acne?
- Who Gets Acne?
- How Is Acne Treated?
- Treatment for Blackheads, Whiteheads, and Mild Inflammatory Acne
- Treatment for Moderate-to-Severe Inflammatory Acne
- Treatment for Severe Nodular or Cystic Acne
- Treatments for Hormonally Influenced Acne in Women
- Other Treatments for Acne
- How Should People With Acne Care for Their Skin?
- What Research Is Being Conducted on Acne?
- Where Can People Find More Information About Acne?
How Does Acne Develop?
Doctors describe acne as a disease of the pilosebaceous units (PSUs). Found over most of the body, PSUs consist of a sebaceous gland connected to a canal, called a follicle, that contains a fine hair (see “Normal Pilosebaceous Unit” diagram). These units are most numerous on the face, upper back, and chest. The sebaceous glands make an oily substance called sebum that normally empties onto the skin surface through the opening of the follicle, commonly called a pore. Cells called keratinocytes line the follicle.
Normal Pilosebaceous Unit

The hair, sebum, and keratinocytes that fill the narrow follicle may produce a plug, which is an early sign of acne. The plug prevents sebum from reaching the surface of the skin through a pore. The mixture of oil and cells allows bacteria Propionibacterium acnes (P. acnes) that normally live on the skin to grow in the plugged follicles. These bacteria produce chemicals and enzymes and attract white blood cells that cause inflammation. (Inflammation is a characteristic reaction of tissues to disease or injury and is marked by four signs: swelling, redness, heat, and pain.) When the wall of the plugged follicle breaks down, it spills everything into the nearby skin—sebum, shed skin cells, and bacteria—leading to lesions or pimples.
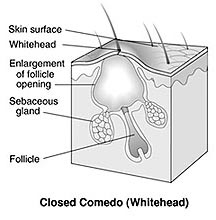
People with acne frequently have a variety of lesions, some of which are shown in the diagrams below. The basic acne lesion, called the comedo (KOM-e-do), is simply an enlarged and plugged hair follicle. If the plugged follicle, or comedo, stays beneath the skin, it is called a closed comedo and produces a white bump called a whitehead. A comedo that reaches the surface of the skin and opens up is called an open comedo or blackhead because it looks black on the skin’s surface. This black discoloration is due to changes in sebum as it is exposed to air. It is not due to dirt. Both whiteheads and blackheads may stay in the skin for a long time.
Types of Lesions


Other troublesome acne lesions can develop, including the following:
- Papules—Inflamed lesions that usually appear as small, pink bumps on the skin and can be tender to the touch.
- Pustules (pimples)—Papules topped by white or yellow pus-filled lesions that may be red at the base.
- Nodules—Large, painful, solid lesions that are lodged deep within the skin.
- Cysts—Deep, painful, pus-filled lesions that can cause scarring.
What Causes Acne?
The exact cause of acne is unknown, but doctors believe it results from several related factors. One important factor is an increase in hormones called androgens (male sex hormones). These increase in both boys and girls during puberty and cause the sebaceous glands to enlarge and make more sebum. Hormonal changes related to pregnancy or starting or stopping birth control pills can also cause acne.
Another factor is heredity or genetics. Researchers believe that the tendency to develop acne can be inherited from parents. For example, studies have shown that many school-age boys with acne have a family history of the disorder. Certain drugs, including androgens and lithium, are known to cause acne. Greasy cosmetics may alter the cells of the follicles and make them stick together, producing a plug.
Factors That Can Make Acne Worse
Factors that can cause an acne flare include:
- changing hormone levels in adolescent girls and adult women before their menstrual period starts
- oil from skin products (lubricants or cosmetics) or grease encountered in the work environment (for example, a kitchen with fry vats)
- pressure from sports helmets or equipment, backpacks, tight collars, or tight sports uniforms
- environmental irritants, such as pollution and high humidity
- squeezing or picking at blemishes
- hard scrubbing of the skin
- stress.
Myths About the Causes of Acne
There are many myths about what causes acne. Chocolate and greasy foods are often blamed, but there is little evidence that foods have much effect on the development and course of acne in most people. Another common myth is that dirty skin causes acne; however, blackheads and other acne lesions are not caused by dirt. Stress doesn’t cause acne, but research suggests that for people who have acne, stress can make it worse.
Who Gets Acne?
People of all races and ages get acne. It is most common in adolescents and young adults. For most people, acne tends to go away by the time they reach their thirties; however, some people in their forties and fifties continue to have this skin problem.
How Is Acne Treated?
Acne is often treated by dermatologists (doctors who specialize in skin problems). These doctors treat all kinds of acne, particularly severe cases. Doctors who are general or family practitioners, pediatricians, or internists may treat patients with milder cases of acne.
The goals of treatment are to heal existing lesions, stop new lesions from forming, prevent scarring, and minimize the psychological stress and embarrassment caused by this disease. Drug treatment1 is aimed at reducing several problems that play a part in causing acne:
- abnormal clumping of cells in the follicles
- increased oil production
- bacteria
- inflammation.
1 All medicines can have side effects. Some medicines and side effects are mentioned in this booklet. Some side effects may be more severe than others. You should review the package insert that comes with your medicine and ask your health care provider or pharmacist if you have any questions about the possible side effects.
Depending on the extent of the problem, the doctor may recommend one of several over-the-counter (OTC) medicines and/or prescription medicines. Some of these medicines may be topical (applied to the skin), and others may be oral (taken by mouth).
Treatment for Blackheads, Whiteheads, and Mild Inflammatory Acne
Doctors usually recommend an OTC or prescription topical medicine for people with mild signs of acne. Topical medicine is applied directly to the acne lesions or to the entire area of affected skin.
There are several OTC topical medicines used for mild acne. Each works a little differently. Following are the most common ones:
- Benzoyl peroxide. Destroys P. acnes and may also reduce oil production.
- Resorcinol. Can help break down blackheads and whiteheads.
- Salicylic acid. Helps break down blackheads and whiteheads. Also helps cut down the shedding of cells lining the hair follicles.
- Sulfur. Helps break down blackheads and whiteheads.
Topical OTC medicines are available in many forms, such as gels, lotions, creams, soaps, or pads. In some people, OTC acne medicines may cause side effects such as skin irritation, burning, or redness, which often get better or go away with continued use of the medicine. If you experience severe or prolonged side effects, you should report them to your doctor.
Treatment for Moderate-to-Severe Inflammatory Acne
People with moderate-to-severe inflammatory acne may be treated with prescription topical or oral medicines, alone or in combination.
Prescription Topical Medicines
Several types of prescription topical medicines are used to treat acne. They include:
- Antibiotics. Help stop or slow the growth of bacteria and reduce inflammation
- Vitamin A derivatives (retinoids). Unplug existing comedones (plural of comedo), allowing other topical medicines, such as antibiotics, to enter the follicles. Some may also help decrease the formation of comedones. These drugs contain an altered form of vitamin A. Some examples are tretinoin, adapalene, and tazarotene.
- Others. May kill P. acnes and reduce oil production or help stop or slow the growth of bacteria and reduce inflammation. Some examples are prescription strength benzoyl peroxide, sodium sulfacetamide/sulfur-containing products, or azelaic acid.
Like OTC topical medicines, prescription topical medicines come as creams, lotions, solutions, gels, or pads. Your doctor will consider your skin type when prescribing a product. Creams and lotions provide moisture and tend to be good choices for people with sensitive skin. If you have very oily skin or live in a hot, humid climate, you may prefer an alcohol-based gel or solution, which tends to dry the skin. Your doctor will tell you how to apply the medicine and how often to use it.
For some people, prescription topical medicines cause minor side effects, including stinging, burning, redness, peeling, scaling, or discoloration of the skin. With some medicines, such as tretinoin, these side effects usually decrease or go away after the medicine is used for a period of time. If side effects are severe or don’t go away, notify your doctor.
Prescription Oral Medicines
For patients with moderate-to-severe acne, doctors often prescribe oral antibiotics. Oral antibiotics are thought to help control acne by curbing the growth of bacteria and reducing inflammation. Prescription oral and topical medicines may be combined.
Treatment for Severe Nodular or Cystic Acne
People with nodules or cysts should be treated by a dermatologist. For patients with severe inflammatory acne that does not improve with medicines such as those described above, a doctor may prescribe isotretinoin, a retinoid (vitamin A derivative). It markedly reduces the size of the oil glands so that much less oil is produced. As a result, the growth of bacteria is decreased.
Advantages of Isotretinoin
Isotretinoin is a very effective medicine that can help prevent scarring. In those patients where acne recurs after a course of isotretinoin, the doctor may institute another course of the same treatment or prescribe other medicines.
Side-Effects of Isotretinoin
Isotretinoin can cause birth defects in the developing fetus of a pregnant woman. It is important that women of childbearing age are not pregnant and do not get pregnant while taking this medicine. You should ask your doctor when it is safe to get pregnant after you have stopped taking isotretinoin.
Some people with acne become depressed by the changes in the appearance of their skin. Changes in mood may be intensified during treatment or soon after completing a course of medicines like isotretinoin. There have been a number of reported suicides and suicide attempts in people taking isotretinoin; however, the connection between isotretinoin and suicide or depression is not known. Nevertheless, if you or someone you know feels unusually sad or has other symptoms of depression, such as loss of appetite, loss of interest in once-loved activities, or trouble concentrating, it’s important to consult your doctor.
Other possible side effects of isotretinoin include:
- dry eyes, mouth, lips, nose, or skin (very common)
- itching
- nosebleeds
- muscle aches
- sensitivity to the sun
- poor night vision
- changes in the blood, such as an increase in fats in the blood (triglycerides and cholesterol)
- change in liver function.
To be able to determine if isotretinoin should be stopped if side effects occur, your doctor may test your blood before you start treatment and periodically during treatment.
Treatments for Hormonally Influenced Acne in Women
In some women, acne is caused by an excess of androgen (male) hormones. Clues that this may be the case include hirsutism (excessive growth of hair on the face or body), premenstrual acne flares, irregular menstrual cycles, and elevated blood levels of certain androgens.
The doctor may prescribe one of several drugs to treat women with this type of acne:
- Birth control pills. Help suppress the androgen produced by the ovaries.
- Low-dose corticosteroid drugs. Help suppress the androgen produced by the adrenal glands.
- Antiandrogen drugs. Reduce the excessive oil production.
Side effects of antiandrogen drugs may include irregular menstruation, tender breasts, headaches, and fatigue.
Other Treatments for Acne
Doctors may use other types of procedures in addition to drug therapy to treat patients with acne. For example, the doctor may remove the patient’s comedones during office visits. Sometimes the doctor will inject corticosteroids directly into lesions to help reduce the size and pain of inflamed cysts and nodules.
Early treatment is the best way to prevent acne scars. Once scarring has occurred, the doctor may suggest a medical or surgical procedure to help reduce the scars. A superficial laser may be used to treat irregular scars. Dermabrasion (or microdermabrasion), which is a form of “sanding down” scars, is sometimes used. Another treatment option for deep scars caused by cystic acne is the transfer of fat from another part of the body to the scar. A doctor may also inject a synthetic filling material under the scar to improve its appearance.
How Should People With Acne Care for Their Skin?
Clean Skin Gently
If you have acne, you should gently wash your face with a mild cleanser, once in the morning and once in the evening, as well as after heavy exercise. Wash your face from under the jaw to the hairline and be sure to thoroughly rinse your skin.
Ask your doctor or another health professional for advice on the best type of cleanser to use.
Using strong soaps or rough scrub pads is not helpful and can actually make the problem worse. Astringents are not recommended unless the skin is very oily, and then they should be used only on oily spots.
It is also important to shampoo your hair regularly. If you have oily hair, you may want to wash it every day.
Avoid Frequent Handling of the Skin
Avoid rubbing and touching skin lesions. Squeezing, pinching or picking blemishes can lead to the development of scars or dark blotches.
Shave Carefully
Men who shave and who have acne should test both electric and safety razors to see which is more comfortable. When using a safety razor, make sure the blade is sharp and soften your beard thoroughly with soap and water before applying shaving cream. Shave gently and only when necessary to reduce the risk of nicking blemishes.
Avoid a Sunburn or Suntan
Many of the medicines used to treat acne can make you more prone to sunburn. A sunburn that reddens the skin or suntan that darkens the skin may make blemishes less visible and make the skin feel drier. However, these benefits are only temporary, and there are known risks of excessive sun exposure, such as more rapid skin aging and a risk of developing skin cancer.
Choose Cosmetics Carefully
While undergoing acne treatment, you may need to change some of the cosmetics you use. All cosmetics, such as foundation, blush, eye shadow, lubricants, and hair-care products should be oil free. Choose products labeled noncomedogenic (meaning they don’t promote the formation of closed pores). In some people, however, even these products may make acne worse.
What Research Is Being Conducted on Acne?
Medical researchers are looking for new drugs to treat acne, particularly topical antibiotics to replace some of those in current use. As with many other types of bacterial infections, doctors are finding that, over time, the bacteria that are associated with acne are becoming resistant to treatment with certain antibiotics, though it is not clear how significant a problem this resistance represents.
Scientists continue to conduct research to better understand how acne develops so that they can identify new targets to treat the disorder. Researchers supported by the National Institutes of Health have discovered that certain genes are highly expressed in the skin lesions of patients with acne. In addition, these scientists are better understanding the inflammatory response that contributes to the development of the disorder.
Other areas of National Institutes of Health (NIH)-supported research involve exploring the role of the innate (primitive) immune system in the development of acne, and examining the mechanism of action of isotretinoin on the sebaceous glands.
Information on research is available from the following resources:
- NIH Clinical Research Trials and You helps people learn more about clinical trials, why they matter, and how to participate. Visitors to the website will find information about the basics of participating in a clinical trial, first-hand stories from actual clinical trial volunteers, explanations from researchers, and links to how to search for a trial or enroll in a research-matching program.
- ClinicalTrials.gov offers up-to-date information for locating federally and privately supported clinical trials for a wide range of diseases and conditions.
- NIH RePORTER is an electronic tool that allows users to search a repository of both intramural and extramural NIH-funded research projects from the past 25 years and access publications (since 1985) and patents resulting from NIH funding.
- PubMed is a free service of the U.S. National Library of Medicine that lets you search millions of journal citations and abstracts in the fields of medicine, nursing, dentistry, veterinary medicine, the health care system, and preclinical sciences.
Where Can People Find More Information About Acne?
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
Information Clearinghouse
National Institutes of Health
1 AMS Circle
Bethesda, MD 20892-3675
Phone: 301-495-4484
Toll Free: 877-22-NIAMS (877-226-4267)
TTY: 301-565-2966
Fax: 301-718-6366
Email: NIAMSinfo@mail.nih.gov
Website: http://www.niams.nih.gov
Other Resources
American Academy of Dermatology (AAD)
Website: http://www.aad.org
For additional contact information, visit the NIAMS website or call the NIAMS Information Clearinghouse.
Acknowledgments
The NIAMS gratefully acknowledges the assistance of the the following individuals in the preparation and review of the original version of this booklet: Laurence H. Miller, M.D., Chevy Chase, MD; Kenneth A. Katz, M.D., M.Sc., University of Pennsylvania School of Medicine, Philadelphia, PA; Edward W. Cowen, M.D., National Cancer Institute, NIH; and Alan Moshell, M.D., NIAMS, NIH.
The mission of the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), a part of the U.S. Department of Health and Human Services’ National Institutes of Health (NIH), is to support research into the causes, treatment, and prevention of arthritis and musculoskeletal and skin diseases; the training of basic and clinical scientists to carry out this research; and the dissemination of information on research progress in these diseases. The NIAMS Information Clearinghouse is a public service sponsored by the NIAMS that provides health information and information sources. Additional information can be found on the NIAMS website at www.niams.nih.gov.
For Your Information
This publication contains information about medications used to treat the health condition discussed here. When this publication was developed, we included the most up-to-date (accurate) information available. Occasionally, new information on medication is released.
For updates and for any questions about any medications you are taking, please contact
-
U.S. Food and Drug Administration
Toll Free: 888–INFO–FDA (888–463–6332)
Website: http://www.fda.gov
For updates and questions about statistics, please contact
-
Centers for Disease Control and Prevention's National Center for Health Statistics
Website: http://www.cdc.gov/nchs
This publication is not copyrighted. Readers are encouraged to duplicate and distribute as many copies as needed.
Additional copies of this publication are available from:
-
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
Information Clearinghouse
National Institutes of Health1 AMS Circle
Bethesda, MD 20892-3675
Phone: 301-495-4484
Toll Free: 877-22-NIAMS (877-226-4267)
TTY: 301-565-2966
Fax: 301-718-6366
Email: NIAMSinfo@mail.nih.gov
Website: http://www.niams.nih.gov
NIH Publication No. 06–4998